Abstract
Astrocytes are specialized cells capable of regulating inflammatory responses in neurodegenerative diseases or traumatic brain injury. In addition to playing an important role in neuroinflammation, these cells regulate essential functions for the preservation of brain tissue. Therefore, the search for therapeutic alternatives to preserve these cells and maintain their functions contributes in some way to counteract the progress of the injury and maintain neuronal survival in various brain pathologies. Among these strategies, the conditioned medium from human adipose-derived mesenchymal stem cells (CM-hMSCA) has been reported with a potential beneficial effect against several neuropathologies. In this study, we evaluated the potential effect of CM-hMSCA in a model of human astrocytes (T98G cells) subjected to scratch injury. Our findings demonstrated that CM-hMSCA regulates the cytokines IL-2, IL-6, IL-8, IL-10, GM-CSF, and TNF-α, downregulates calcium at the cytoplasmic level, and regulates mitochondrial dynamics and the respiratory chain. These actions are accompanied by modulation of the expression of different proteins involved in signaling pathways such as AKT/pAKT and ERK1/2/pERK, and may mediate the localization of neuroglobin (Ngb) at the cellular level. We also confirmed that Ngb mediated the protective effects of CM-hMSCA through regulation of proteins involved in survival pathways and oxidative stress. In conclusion, regulation of brain inflammation combined with the recovery of fundamental cellular aspects in the face of injury makes CM-hMSCA a promising candidate for the protection of astrocytes in brain pathologies.








Similar content being viewed by others
Change history
09 December 2021
A Correction to this paper has been published: https://doi.org/10.1007/s12035-021-02618-0
References
Chen WW, Zhang X, Huang WJ (2016) Role of neuroinflammation in neurodegenerative diseases (review). Mol Med Rep 13(4):3391–3396. https://doi.org/10.3892/mmr.2016.4948
Gonzalez H, Elgueta D, Montoya A, Pacheco R (2014) Neuroimmune regulation of microglial activity involved in neuroinflammation and neurodegenerative diseases. J Neuroimmunol 274(1–2):1–13. https://doi.org/10.1016/j.jneuroim.2014.07.012
Villegas-Llerena C, Phillips A, Garcia-Reitboeck P, Hardy J, Pocock JM (2016) Microglial genes regulating neuroinflammation in the progression of Alzheimer's disease. Curr Opin Neurobiol 36:74–81. https://doi.org/10.1016/j.conb.2015.10.004
Karve IP, Taylor JM, Crack PJ (2016) The contribution of astrocytes and microglia to traumatic brain injury. Br J Pharmacol 173(4):692–702. https://doi.org/10.1111/bph.13125
Sochocka M, Diniz BS, Leszek J (2017) Inflammatory response in the CNS: friend or foe? Mol Neurobiol 54(10):8071–8089. https://doi.org/10.1007/s12035-016-0297-1
Pedraza-Alva G, Perez-Martinez L, Valdez-Hernandez L, Meza-Sosa KF, Ando-Kuri M (2015) Negative regulation of the inflammasome: keeping inflammation under control. Immunol Rev 265(1):231–257. https://doi.org/10.1111/imr.12294
Ulusoy C, Zibandeh N, Yildirim S, Trakas N, Zisimopoulou P, Kucukerden M, Tasli H, Tzartos S et al (2015) Dental follicle mesenchymal stem cell administration ameliorates muscle weakness in MuSK-immunized mice. J Neuroinflammation 12:231. https://doi.org/10.1186/s12974-015-0451-0
Trubiani O, Giacoppo S, Ballerini P, Diomede F, Piattelli A, Bramanti P, Mazzon E (2016) Alternative source of stem cells derived from human periodontal ligament: a new treatment for experimental autoimmune encephalomyelitis. Stem Cell Res Ther 7:1. https://doi.org/10.1186/s13287-015-0253-4
Baez-Jurado E, Hidalgo-Lanussa O, Guio-Vega G, Ashraf GM, Echeverria V, Aliev G, Barreto GE (2018) Conditioned medium of human adipose mesenchymal stem cells increases wound closure and protects human astrocytes following scratch assay in vitro. Mol Neurobiol 55(6):5377–5392. https://doi.org/10.1007/s12035-017-0771-4
Baez-Jurado E, Vega GG, Aliev G, Tarasov VV, Esquinas P, Echeverria V, Barreto GE (2018) Blockade of neuroglobin reduces protection of conditioned medium from human mesenchymal stem cells in human astrocyte model (T98G) under a scratch assay. Mol Neurobiol 55(3):2285–2300. https://doi.org/10.1007/s12035-017-0481-y
Konala VB, Mamidi MK, Bhonde R, Das AK, Pochampally R, Pal R (2016) The current landscape of the mesenchymal stromal cell secretome: a new paradigm for cell-free regeneration. Cytotherapy 18(1):13–24. https://doi.org/10.1016/j.jcyt.2015.10.008
Guillen MI, Platas J, Perez Del Caz MD, Mirabet V, Alcaraz MJ (2018) Paracrine anti-inflammatory effects of adipose tissue-derived mesenchymal stem cells in human monocytes. Front Physiol 9:661. https://doi.org/10.3389/fphys.2018.00661
Guo ZY, Sun X, Xu XL, Zhao Q, Peng J, Wang Y (2015) Human umbilical cord mesenchymal stem cells promote peripheral nerve repair via paracrine mechanisms. Neural Regen Res 10(4):651–658. https://doi.org/10.4103/1673-5374.155442
Mita T, Furukawa-Hibi Y, Takeuchi H, Hattori H, Yamada K, Hibi H, Ueda M, Yamamoto A (2015) Conditioned medium from the stem cells of human dental pulp improves cognitive function in a mouse model of Alzheimer's disease. Behav Brain Res 293:189–197. https://doi.org/10.1016/j.bbr.2015.07.043
Pischiutta F, Brunelli L, Romele P, Silini A, Sammali E, Paracchini L, Marchini S, Talamini L et al (2016) Protection of brain injury by amniotic mesenchymal stromal cell-secreted metabolites. Crit Care Med 44(11):e1118–e1131. https://doi.org/10.1097/CCM.0000000000001864
Mekhemar MK, Adam-Klages S, Kabelitz D, Dorfer CE, Fawzy El-Sayed KM (2018) TLR-induced immunomodulatory cytokine expression by human gingival stem/progenitor cells. Cell Immunol 326:60–67. https://doi.org/10.1016/j.cellimm.2017.01.007
Fawzy El-Sayed KM, Dorfer CE (2016) Gingival mesenchymal stem/progenitor cells: a unique tissue engineering gem. Stem Cells Int 2016:7154327–7154316. https://doi.org/10.1155/2016/7154327
Torrente D, Avila MF, Cabezas R, Morales L, Gonzalez J, Samudio I, Barreto GE (2014) Paracrine factors of human mesenchymal stem cells increase wound closure and reduce reactive oxygen species production in a traumatic brain injury in vitro model. Hum Exp Toxicol 33(7):673–684. https://doi.org/10.1177/0960327113509659
Song M, Jue SS, Cho YA, Kim EC (2015) Comparison of the effects of human dental pulp stem cells and human bone marrow-derived mesenchymal stem cells on ischemic human astrocytes in vitro. J Neurosci Res 93(6):973–983. https://doi.org/10.1002/jnr.23569
Huang W, Lv B, Zeng H, Shi D, Liu Y, Chen F, Li F, Liu X et al (2015) Paracrine factors secreted by MSCs promote astrocyte survival associated with GFAP downregulation after ischemic stroke via p38 MAPK and JNK. J Cell Physiol 230(10):2461–2475. https://doi.org/10.1002/jcp.24981
Sun H, Benardais K, Stanslowsky N, Thau-Habermann N, Hensel N, Huang D, Claus P, Dengler R et al (2013) Therapeutic potential of mesenchymal stromal cells and MSC conditioned medium in amyotrophic lateral sclerosis (ALS)—in vitro evidence from primary motor neuron cultures, NSC-34 cells, astrocytes and microglia. PLoS One 8(9):e72926. https://doi.org/10.1371/journal.pone.0072926
Baez E, Echeverria V, Cabezas R, Avila-Rodriguez M, Garcia-Segura LM, Barreto GE (2016) Protection by neuroglobin expression in brain pathologies. Front Neurol 7:146. https://doi.org/10.3389/fneur.2016.00146
Amri F, Ghouili I, Amri M, Carrier A, Masmoudi-Kouki O (2017) Neuroglobin protects astroglial cells from hydrogen peroxide-induced oxidative stress and apoptotic cell death. J Neurochem 140(1):151–169. https://doi.org/10.1111/jnc.13876
Chen YX, Zeng ZC, Sun J, Zeng HY, Huang Y, Zhang ZY (2015) Mesenchymal stem cell-conditioned medium prevents radiation-induced liver injury by inhibiting inflammation and protecting sinusoidal endothelial cells. J Radiat Res 56(4):700–708. https://doi.org/10.1093/jrr/rrv026
Yu Z, Poppe JL, Wang X (2013) Mitochondrial mechanisms of neuroglobin's neuroprotection. Oxidative Med Cell Longev 2013:756989. https://doi.org/10.1155/2013/756989
Lan WB, Lin JH, Chen XW, Wu CY, Zhong GX, Zhang LQ, Lin WP, Liu WN et al (2014) Overexpressing neuroglobin improves functional recovery by inhibiting neuronal apoptosis after spinal cord injury. Brain Res 1562:100–108. https://doi.org/10.1016/j.brainres.2014.03.020
Lechauve C, Augustin S, Roussel D, Sahel JA, Corral-Debrinski M (2013) Neuroglobin involvement in visual pathways through the optic nerve. Biochim Biophys Acta 1834(9):1772–1778. https://doi.org/10.1016/j.bbapap.2013.04.014
Avivi A, Gerlach F, Joel A, Reuss S, Burmester T, Nevo E, Hankeln T (2010) Neuroglobin, cytoglobin, and myoglobin contribute to hypoxia adaptation of the subterranean mole rat Spalax. Proc Natl Acad Sci U S A 107(50):21570–21575. https://doi.org/10.1073/pnas.1015379107
Zhao S, Yu Z, Zhao G, Xing C, Hayakawa K, Whalen MJ, Lok JM, Lo EH et al (2012) Neuroglobin-overexpression reduces traumatic brain lesion size in mice. BMC Neurosci 13:67. https://doi.org/10.1186/1471-2202-13-67
Yu Z, Liu N, Liu J, Yang K, Wang X (2012) Neuroglobin, a novel target for endogenous neuroprotection against stroke and neurodegenerative disorders. Int J Mol Sci 13(6):6995–7014. https://doi.org/10.3390/ijms13066995
Taylor JM, Kelley B, Gregory EJ, Berman NE (2014) Neuroglobin overexpression improves sensorimotor outcomes in a mouse model of traumatic brain injury. Neurosci Lett 577:125–129. https://doi.org/10.1016/j.neulet.2014.03.012
Zhou Z, Chen Y, Zhang H, Min S, Yu B, He B, Jin A (2013) Comparison of mesenchymal stromal cells from human bone marrow and adipose tissue for the treatment of spinal cord injury. Cytotherapy 15(4):434–448. https://doi.org/10.1016/j.jcyt.2012.11.015
Avila-Rodriguez M, Garcia-Segura LM, Hidalgo-Lanussa O, Baez E, Gonzalez J, Barreto GE (2016) Tibolone protects astrocytic cells from glucose deprivation through a mechanism involving estrogen receptor beta and the upregulation of neuroglobin expression. Mol Cell Endocrinol 433:35–46. https://doi.org/10.1016/j.mce.2016.05.024
Sasaki S, Futagi Y, Kobayashi M, Ogura J, Iseki K (2015) Functional characterization of 5-oxoproline transport via SLC16A1/MCT1. J Biol Chem 290(4):2303–2311. https://doi.org/10.1074/jbc.M114.581892
Cabezas R, Avila MF, Gonzalez J, El-Bacha RS, Barreto GE (2015) PDGF-BB protects mitochondria from rotenone in T98G cells. Neurotox Res 27(4):355–367. https://doi.org/10.1007/s12640-014-9509-5
Mimura J, Kosaka K, Maruyama A, Satoh T, Harada N, Yoshida H, Satoh K, Yamamoto M et al (2011) Nrf2 regulates NGF mRNA induction by carnosic acid in T98G glioblastoma cells and normal human astrocytes. J Biochem 150(2):209–217. https://doi.org/10.1093/jb/mvr065
Bourguignon LY, Gilad E, Peyrollier K, Brightman A, Swanson RA (2007) Hyaluronan-CD44 interaction stimulates Rac1 signaling and PKN gamma kinase activation leading to cytoskeleton function and cell migration in astrocytes. J Neurochem 101(4):1002–1017. https://doi.org/10.1111/j.1471-4159.2007.04485.x
Ouyang YB, Xu LJ, Emery JF, Lee AS, Giffard RG (2011) Overexpressing GRP78 influences Ca2+ handling and function of mitochondria in astrocytes after ischemia-like stress. Mitochondrion 11(2):279–286. https://doi.org/10.1016/j.mito.2010.10.007
Vomelova I, Vaníčková Z, Šedo A (2009) Technical note methods of RNA purification. All ways (should) lead to Rome. Folia Biologica (Praha) 55:243–251
Scientific TF (2015) Real-time PCR Solutions.
Taylor SC, Berkelman T, Yadav G, Hammond M (2013) A defined methodology for reliable quantification of Western blot data. Mol Biotechnol 55(3):217–226. https://doi.org/10.1007/s12033-013-9672-6
Gassmann M, Grenacher B, Rohde B, Vogel J (2009) Quantifying Western blots: pitfalls of densitometry. Electrophoresis 30(11):1845–1855. https://doi.org/10.1002/elps.200800720
Voloboueva LA, Lee SW, Emery JF, Palmer TD, Giffard RG (2010) Mitochondrial protection attenuates inflammation-induced impairment of neurogenesis in vitro and in vivo. J Neurosci 30(37):12242–12251. https://doi.org/10.1523/JNEUROSCI.1752-10.2010
Cassina P, Cassina A, Pehar M, Castellanos R, Gandelman M, de Leon A, Robinson KM, Mason RP et al (2008) Mitochondrial dysfunction in SOD1G93A-bearing astrocytes promotes motor neuron degeneration: prevention by mitochondrial-targeted antioxidants. J Neurosci 28(16):4115–4122. https://doi.org/10.1523/JNEUROSCI.5308-07.2008
Wang H, Joseph JA (1999) Quantifying cellular oxidative stress by dichlorofluorescein assay using microplate reader. Free Radic Biol Med 27(5–6):612–616
Alarifi S, Ali D, Alkahtani S (2015) Nanoalumina induces apoptosis by impairing antioxidant enzyme systems in human hepatocarcinoma cells. Int J Nanomedicine 10:3751–3760. https://doi.org/10.2147/IJN.S82050
Pokrzywinski KL, Tilney CL, Warner ME, Coyne KJ (2017) Cell cycle arrest and biochemical changes accompanying cell death in harmful dinoflagellates following exposure to bacterial algicide IRI-160AA. Sci Rep 7:45102. https://doi.org/10.1038/srep45102
Jeong SH, Kim HK, Song IS, Noh SJ, Marquez J, Ko KS, Rhee BD, Kim N et al (2014) Echinochrome a increases mitochondrial mass and function by modulating mitochondrial biogenesis regulatory genes. Marine Drugs 12(8):4602–4615. https://doi.org/10.3390/md12084602
Oliva CR, Moellering DR, Gillespie GY, Griguer CE (2011) Acquisition of chemoresistance in gliomas is associated with increased mitochondrial coupling and decreased ROS production. PLoS One 6(9):e24665. https://doi.org/10.1371/journal.pone.0024665
Hidalgo-Lanussa O, Avila-Rodriguez M, Baez-Jurado E, Zamudio J, Echeverria V, Garcia-Segura LM, Barreto GE (2018) Tibolone reduces oxidative damage and inflammation in microglia stimulated with palmitic acid through mechanisms involving estrogen receptor beta. Mol Neurobiol 55(7):5462–5477. https://doi.org/10.1007/s12035-017-0777-y
Li Q, Lau A, Morris TJ, Guo L, Fordyce CB, Stanley EF (2004) A syntaxin 1, Galpha(o), and N-type calcium channel complex at a presynaptic nerve terminal: analysis by quantitative immunocolocalization. J Neurosci 24(16):4070–4081. https://doi.org/10.1523/JNEUROSCI.0346-04.2004
Amor S, Puentes F, Baker D, van der Valk P (2010) Inflammation in neurodegenerative diseases. Immunology 129(2):154–169. https://doi.org/10.1111/j.1365-2567.2009.03225.x
Stephenson J, Nutma E, van der Valk P, Amor S (2018) Inflammation in CNS neurodegenerative diseases. Immunology 154(2):204–219. https://doi.org/10.1111/imm.12922
Kokiko-Cochran ON, Godbout JP (2018) The inflammatory continuum of traumatic brain injury and Alzheimer's disease. Front Immunol 9:672. https://doi.org/10.3389/fimmu.2018.00672
Chung WS, Allen NJ, Eroglu C (2015) Astrocytes control synapse formation, function, and elimination. Cold Spring Harb Perspect Biol 7(9):a020370. https://doi.org/10.1101/cshperspect.a020370
Becerra-Calixto A, Cardona-Gomez GP (2017) The role of astrocytes in neuroprotection after brain stroke: potential in cell therapy. Front Mol Neurosci 10:88. https://doi.org/10.3389/fnmol.2017.00088
Kimelberg HK, Nedergaard M (2010) Functions of astrocytes and their potential as therapeutic targets. Neurotherapeutics 7(4):338–353. https://doi.org/10.1016/j.nurt.2010.07.006
Cekanaviciute E, Buckwalter MS (2016) Astrocytes: integrative regulators of neuroinflammation in stroke and other neurological diseases. Neurotherapeutics 13(4):685–701. https://doi.org/10.1007/s13311-016-0477-8
Colombo E, Farina C (2016) Astrocytes: key regulators of neuroinflammation. Trends Immunol 37(9):608–620. https://doi.org/10.1016/j.it.2016.06.006
Le Thuc O, Blondeau N, Nahon JL, Rovere C (2015) The complex contribution of chemokines to neuroinflammation: switching from beneficial to detrimental effects. Ann N Y Acad Sci 1351:127–140. https://doi.org/10.1111/nyas.12855
Kempuraj D, Thangavel R, Selvakumar GP, Zaheer S, Ahmed ME, Raikwar SP, Zahoor H, Saeed D et al (2017) Brain and peripheral atypical inflammatory mediators potentiate neuroinflammation and neurodegeneration. Front Cell Neurosci 11:216. https://doi.org/10.3389/fncel.2017.00216
Cunningham CJ, Redondo-Castro E, Allan SM (2018) The therapeutic potential of the mesenchymal stem cell secretome in ischaemic stroke. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism:271678X18776802. https://doi.org/10.1177/0271678X18776802
Valencia J, Blanco B, Yanez R, Vazquez M, Herrero Sanchez C, Fernandez-Garcia M, Rodriguez Serrano C, Pescador D et al (2016) Comparative analysis of the immunomodulatory capacities of human bone marrow- and adipose tissue-derived mesenchymal stromal cells from the same donor. Cytotherapy 18(10):1297–1311. https://doi.org/10.1016/j.jcyt.2016.07.006
Gimeno ML, Fuertes F, Barcala Tabarrozzi AE, Attorressi AI, Cucchiani R, Corrales L, Oliveira TC, Sogayar MC et al (2017) Pluripotent nontumorigenic adipose tissue-derived muse cells have immunomodulatory capacity mediated by transforming growth factor-beta1. Stem Cells Transl Med 6(1):161–173. https://doi.org/10.5966/sctm.2016-0014
Gao F, Chiu SM, Motan DA, Zhang Z, Chen L, Ji HL, Tse HF, Fu QL et al (2016) Mesenchymal stem cells and immunomodulation: current status and future prospects. Cell Death Dis 7:e2062. https://doi.org/10.1038/cddis.2015.327
Hariri RJ, Chang VA, Barie PS, Wang RS, Sharif SF, Ghajar JB (1994) Traumatic injury induces interleukin-6 production by human astrocytes. Brain Res 636(1):139–142
Liu C, Cui G, Zhu M, Kang X, Guo H (2014) Neuroinflammation in Alzheimer's disease: chemokines produced by astrocytes and chemokine receptors. Int J Clin Exp Pathol 7(12):8342–8355
Phuagkhaopong S, Ospondpant D, Kasemsuk T, Sibmooh N, Soodvilai S, Power C, Vivithanaporn P (2017) Cadmium-induced IL-6 and IL-8 expression and release from astrocytes are mediated by MAPK and NF-kappaB pathways. Neurotoxicology 60:82–91. https://doi.org/10.1016/j.neuro.2017.03.001
Gijbels K, Van Damme J, Proost P, Put W, Carton H, Billiau A (1990) Interleukin 6 production in the central nervous system during experimental autoimmune encephalomyelitis. Eur J Immunol 20(1):233–235. https://doi.org/10.1002/eji.1830200134
Jiang Y, Deacon R, Anthony DC, Campbell SJ (2008) Inhibition of peripheral TNF can block the malaise associated with CNS inflammatory diseases. Neurobiol Dis 32(1):125–132. https://doi.org/10.1016/j.nbd.2008.06.017
Lucas SM, Rothwell NJ, Gibson RM (2006) The role of inflammation in CNS injury and disease. Br J Pharmacol 147(Suppl 1):S232–S240. https://doi.org/10.1038/sj.bjp.0706400
Tehranian R, Andell-Jonsson S, Beni SM, Yatsiv I, Shohami E, Bartfai T, Lundkvist J, Iverfeldt K (2002) Improved recovery and delayed cytokine induction after closed head injury in mice with central overexpression of the secreted isoform of the interleukin-1 receptor antagonist. J Neurotrauma 19(8):939–951. https://doi.org/10.1089/089771502320317096
Guida E, Stewart A (1998) Influence of hypoxia and glucose deprivation on tumour necrosis factor-alpha and granulocyte-macrophage colony-stimulating factor expression in human cultured monocytes. Cell Physiol Biochem 8(1–2):75–88. https://doi.org/10.1159/000016272
Opal SM, DePalo VA (2000) Anti-inflammatory cytokines. Chest 117(4):1162–1172
Xia W, Peng GY, Sheng JT, Zhu FF, Guo JF, Chen WQ (2015) Neuroprotective effect of interleukin-6 regulation of voltage-gated Na(+) channels of cortical neurons is time- and dose-dependent. Neural Regen Res 10(4):610–617. https://doi.org/10.4103/1673-5374.155436
Erta M, Quintana A, Hidalgo J (2012) Interleukin-6, a major cytokine in the central nervous system. Int J Biol Sci 8(9):1254–1266. https://doi.org/10.7150/ijbs.4679
Jiang T, Cadenas E (2014) Astrocytic metabolic and inflammatory changes as a function of age. Aging Cell 13(6):1059–1067. https://doi.org/10.1111/acel.12268
Chen XL, Wang Y, Peng WW, Zheng YJ, Zhang TN, Wang PJ, Huang JD, Zeng QY (2018) Effects of interleukin-6 and IL-6/AMPK signaling pathway on mitochondrial biogenesis and astrocytes viability under experimental septic condition. Int Immunopharmacol 59:287–294. https://doi.org/10.1016/j.intimp.2018.04.020
Jiang CL, Lu CL (1998) Interleukin-2 and its effects in the central nervous system. Biol Signals Recept 7(3):148–156. https://doi.org/10.1159/000014541
Xie L, Choudhury GR, Winters A, Yang SH, Jin K (2015) Cerebral regulatory T cells restrain microglia/macrophage-mediated inflammatory responses via IL-10. Eur J Immunol 45(1):180–191. https://doi.org/10.1002/eji.201444823
Bhela S, Varanasi SK, Jaggi U, Sloan SS, Rajasagi NK, Rouse BT (2017) The plasticity and stability of regulatory T cells during viral-induced inflammatory lesions. J Immunol 199(4):1342–1352. https://doi.org/10.4049/jimmunol.1700520
Rothhammer V, Quintana FJ (2015) Control of autoimmune CNS inflammation by astrocytes. Semin Immunopathol 37(6):625–638. https://doi.org/10.1007/s00281-015-0515-3
Bajetto A, Bonavia R, Barbero S, Schettini G (2002) Characterization of chemokines and their receptors in the central nervous system: physiopathological implications. J Neurochem 82(6):1311–1329
Hao P, Liang Z, Piao H, Ji X, Wang Y, Liu Y, Liu R, Liu J (2014) Conditioned medium of human adipose-derived mesenchymal stem cells mediates protection in neurons following glutamate excitotoxicity by regulating energy metabolism and GAP-43 expression. Metab Brain Dis 29(1):193–205. https://doi.org/10.1007/s11011-014-9490-y
Bruno V, Copani A, Besong G, Scoto G, Nicoletti F (2000) Neuroprotective activity of chemokines against N-methyl-D-aspartate or beta-amyloid-induced toxicity in culture. Eur J Pharmacol 399(2–3):117–121
Mamik MK, Ghorpade A (2016) CXCL8 as a potential therapeutic target for HIV-associated neurocognitive disorders. Curr Drug Targets 17(1):111–121
Meiron M, Zohar Y, Anunu R, Wildbaum G, Karin N (2008) CXCL12 (SDF-1alpha) suppresses ongoing experimental autoimmune encephalomyelitis by selecting antigen-specific regulatory T cells. J Exp Med 205(11):2643–2655. https://doi.org/10.1084/jem.20080730
Chaudhry H, Zhou J, Zhong Y, Ali MM, McGuire F, Nagarkatti PS, Nagarkatti M (2013) Role of cytokines as a double-edged sword in sepsis. In Vivo 27(6):669–684
Linero I, Chaparro O (2014) Paracrine effect of mesenchymal stem cells derived from human adipose tissue in bone regeneration. PLoS One 9(9):e107001. https://doi.org/10.1371/journal.pone.0107001
Kilroy GE, Foster SJ, Wu X, Ruiz J, Sherwood S, Heifetz A, Ludlow JW, Stricker DM et al (2007) Cytokine profile of human adipose-derived stem cells: expression of angiogenic, hematopoietic, and pro-inflammatory factors. J Cell Physiol 212(3):702–709. https://doi.org/10.1002/jcp.21068
Wei X, Du Z, Zhao L, Feng D, Wei G, He Y, Tan J, Lee WH et al (2009) IFATS collection: the conditioned media of adipose stromal cells protect against hypoxia-ischemia-induced brain damage in neonatal rats. Stem Cells 27(2):478–488. https://doi.org/10.1634/stemcells.2008-0333
Kupcova Skalnikova H (2013) Proteomic techniques for characterisation of mesenchymal stem cell secretome. Biochimie 95(12):2196–2211. https://doi.org/10.1016/j.biochi.2013.07.015
Deng LX, Hu J, Liu N, Wang X, Smith GM, Wen X, Xu XM (2011) GDNF modifies reactive astrogliosis allowing robust axonal regeneration through Schwann cell-seeded guidance channels after spinal cord injury. Exp Neurol 229(2):238–250. https://doi.org/10.1016/j.expneurol.2011.02.001
Cirillo G, Bianco MR, Colangelo AM, Cavaliere C, Daniele de L, Zaccaro L, Alberghina L, Papa M (2011) Reactive astrocytosis-induced perturbation of synaptic homeostasis is restored by nerve growth factor. Neurobiol Dis 41(3):630–639. https://doi.org/10.1016/j.nbd.2010.11.012
Dimitrov DH, Lee S, Yantis J, Honaker C, Braida N (2014) Cytokine serum levels as potential biological markers for the psychopathology in schizophrenia. Adv Psychiatry 2014:1–7
Holliday J, Gruol DL (1993) Cytokine stimulation increases intracellular calcium and alters the response to quisqualate in cultured cortical astrocytes. Brain Res 621(2):233–241
Galic MA, Riazi K, Pittman QJ (2012) Cytokines and brain excitability. Front Neuroendocrinol 33(1):116–125. https://doi.org/10.1016/j.yfrne.2011.12.002
Shinotsuka T, Yasui M, Nuriya M (2014) Astrocytic gap junctional networks suppress cellular damage in an in vitro model of ischemia. Biochem Biophys Res Commun 444(2):171–176. https://doi.org/10.1016/j.bbrc.2014.01.035
Helleringer R, Chever O, Daniel H, Galante M (2017) Oxygen and glucose deprivation induces Bergmann glia membrane depolarization and ca(2+) rises mainly mediated by K(+) and ATP increases in the extracellular space. Front Cell Neurosci 11:349. https://doi.org/10.3389/fncel.2017.00349
Reuss B, von Bohlen und Halback O (2003) Fibroblast growth factors and their receptors in the central nervous system. Cell Tissue Res 313(2):139–157. https://doi.org/10.1007/s00441-003-0756-7
Wilkins A, Kemp K, Ginty M, Hares K, Mallam E, Scolding N (2009) Human bone marrow-derived mesenchymal stem cells secrete brain-derived neurotrophic factor which promotes neuronal survival in vitro. Stem Cell Res 3(1):63–70. https://doi.org/10.1016/j.scr.2009.02.006
Papazian I, Kyrargyri V, Evangelidou M, Voulgari-Kokota A, Probert L (2018) Mesenchymal stem cell protection of neurons against glutamate excitotoxicity involves reduction of NMDA-triggered calcium responses and surface GluR1, and is partly mediated by TNF. Int J Mol Sci 19 (3). https://doi.org/10.3390/ijms19030651
Taoufik E, Valable S, Muller GJ, Roberts ML, Divoux D, Tinel A, Voulgari-Kokota A, Tseveleki V et al (2007) FLIP(L) protects neurons against in vivo ischemia and in vitro glucose deprivation-induced cell death. J Neurosci 27(25):6633–6646. https://doi.org/10.1523/JNEUROSCI.1091-07.2007
Marchetti L, Klein M, Schlett K, Pfizenmaier K, Eisel UL (2004) Tumor necrosis factor (TNF)-mediated neuroprotection against glutamate-induced excitotoxicity is enhanced by N-methyl-D-aspartate receptor activation. Essential role of a TNF receptor 2-mediated phosphatidylinositol 3-kinase-dependent NF-kappa B pathway. J Biol Chem 279(31):32869–32881. https://doi.org/10.1074/jbc.M311766200
Probert L (2015) TNF and its receptors in the CNS: the essential, the desirable and the deleterious effects. Neuroscience 302:2–22. https://doi.org/10.1016/j.neuroscience.2015.06.038
Morales AP, Carvalho AC, Monteforte PT, Hirata H, Han SW, Hsu YT, Smaili SS (2011) Endoplasmic reticulum calcium release engages Bax translocation in cortical astrocytes. Neurochem Res 36(5):829–838. https://doi.org/10.1007/s11064-011-0411-8
Verkhratsky A, Rodriguez JJ, Parpura V (2012) Calcium signalling in astroglia. Mol Cell Endocrinol 353(1–2):45–56. https://doi.org/10.1016/j.mce.2011.08.039
Johnson GG, White MC, Wu JH, Vallejo M, Grimaldi M (2014) The deadly connection between endoplasmic reticulum, Ca2+, protein synthesis, and the endoplasmic reticulum stress response in malignant glioma cells. Neuro-Oncology 16(8):1086–1099. https://doi.org/10.1093/neuonc/nou012
Begum G, Kintner D, Liu Y, Cramer SW, Sun D (2012) DHA inhibits ER Ca2+ release and ER stress in astrocytes following in vitro ischemia. J Neurochem 120(4):622–630. https://doi.org/10.1111/j.1471-4159.2011.07606.x
Hajnoczky G, Robb-Gaspers LD, Seitz MB, Thomas AP (1995) Decoding of cytosolic calcium oscillations in the mitochondria. Cell 82(3):415–424
Reyes RC, Parpura V (2008) Mitochondria modulate Ca2+−dependent glutamate release from rat cortical astrocytes. J Neurosci 28(39):9682–9691. https://doi.org/10.1523/JNEUROSCI.3484-08.2008
Parpura V, Grubisic V, Verkhratsky A (2011) Ca(2+) sources for the exocytotic release of glutamate from astrocytes. Biochim Biophys Acta 1813(5):984–991. https://doi.org/10.1016/j.bbamcr.2010.11.006
Voulgari-Kokota A, Fairless R, Karamita M, Kyrargyri V, Tseveleki V, Evangelidou M, Delorme B, Charbord P et al (2012) Mesenchymal stem cells protect CNS neurons against glutamate excitotoxicity by inhibiting glutamate receptor expression and function. Exp Neurol 236(1):161–170. https://doi.org/10.1016/j.expneurol.2012.04.011
Cheng B, Furukawa K, O'Keefe JA, Goodman Y, Kihiko M, Fabian T, Mattson MP (1995) Basic fibroblast growth factor selectively increases AMPA-receptor subunit GluR1 protein level and differentially modulates Ca2+ responses to AMPA and NMDA in hippocampal neurons. J Neurochem 65(6):2525–2536
Ranieri M, Brajkovic S, Riboldi G, Ronchi D, Rizzo F, Bresolin N, Corti S, Comi GP (2013) Mitochondrial fusion proteins and human diseases. Neurol Res Int 2013:293893. https://doi.org/10.1155/2013/293893
Burte F, Carelli V, Chinnery PF, Yu-Wai-Man P (2015) Disturbed mitochondrial dynamics and neurodegenerative disorders. Nat Rev Neurol 11(1):11–24. https://doi.org/10.1038/nrneurol.2014.228
Qi X, Disatnik MH, Shen N, Sobel RA, Mochly-Rosen D (2011) Aberrant mitochondrial fission in neurons induced by protein kinase C{delta} under oxidative stress conditions in vivo. Mol Biol Cell 22(2):256–265. https://doi.org/10.1091/mbc.E10-06-0551
Stojanovski D, Koutsopoulos OS, Okamoto K, Ryan MT (2004) Levels of human Fis1 at the mitochondrial outer membrane regulate mitochondrial morphology. J Cell Sci 117(Pt 7):1201–1210. https://doi.org/10.1242/jcs.01058
Elgass K, Pakay J, Ryan MT, Palmer CS (2013) Recent advances into the understanding of mitochondrial fission. Biochim Biophys Acta 1833(1):150–161. https://doi.org/10.1016/j.bbamcr.2012.05.002
Szabadkai G, Simoni AM, Bianchi K, De Stefani D, Leo S, Wieckowski MR, Rizzuto R (2006) Mitochondrial dynamics and Ca2+ signaling. Biochim Biophys Acta 1763(5–6):442–449. https://doi.org/10.1016/j.bbamcr.2006.04.002
Bravo-Sagua R, Parra V, Lopez-Crisosto C, Diaz P, Quest AF, Lavandero S (2017) Calcium transport and signaling in mitochondria. Comp Physiol 7(2):623–634. https://doi.org/10.1002/cphy.c160013
Ogunbileje JO, Porter C, Herndon DN, Chao T, Abdelrahman DR, Papadimitriou A, Chondronikola M, Zimmers TA et al (2016) Hypermetabolism and hypercatabolism of skeletal muscle accompany mitochondrial stress following severe burn trauma. Am J Phys Endocrinol Metab 311(2):E436–E448. https://doi.org/10.1152/ajpendo.00535.2015
Eisner V, Picard M, Hajnóczky G (2018) Mitochondrial dynamics in adaptive and maladaptive cellular stress responses. Nat Cell Biol 1
Tondera D, Grandemange S, Jourdain A, Karbowski M, Mattenberger Y, Herzig S, Da Cruz S, Clerc P et al (2009) SLP-2 is required for stress-induced mitochondrial hyperfusion. EMBO J 28(11):1589–1600. https://doi.org/10.1038/emboj.2009.89
Jagasia R, Grote P, Westermann B, Conradt B (2005) DRP-1-mediated mitochondrial fragmentation during EGL-1-induced cell death in C. elegans. Nature 433(7027):754–760. https://doi.org/10.1038/nature03316
Fannjiang Y, Cheng WC, Lee SJ, Qi B, Pevsner J, McCaffery JM, Hill RB, Basanez G et al (2004) Mitochondrial fission proteins regulate programmed cell death in yeast. Genes Dev 18(22):2785–2797. https://doi.org/10.1101/gad.1247904
Chang CR, Blackstone C (2010) Dynamic regulation of mitochondrial fission through modification of the dynamin-related protein Drp1. Ann N Y Acad Sci 1201:34–39. https://doi.org/10.1111/j.1749-6632.2010.05629.x
Alavi MV, Fuhrmann N (2013) Dominant optic atrophy, OPA1, and mitochondrial quality control: understanding mitochondrial network dynamics. Mol Neurodegener 8:32. https://doi.org/10.1186/1750-1326-8-32
Mishra P, Chan DC (2016) Metabolic regulation of mitochondrial dynamics. J Cell Biol 212(4):379–387. https://doi.org/10.1083/jcb.201511036
Gomes LC, Di Benedetto G, Scorrano L (2011) During autophagy mitochondria elongate, are spared from degradation and sustain cell viability. Nat Cell Biol 13(5):589–598. https://doi.org/10.1038/ncb2220
Lee YJ, Jeong SY, Karbowski M, Smith CL, Youle RJ (2004) Roles of the mammalian mitochondrial fission and fusion mediators Fis1, Drp1, and Opa1 in apoptosis. Mol Biol Cell 15(11):5001–5011. https://doi.org/10.1091/mbc.e04-04-0294
Cereghetti GM, Costa V, Scorrano L (2010) Inhibition of Drp1-dependent mitochondrial fragmentation and apoptosis by a polypeptide antagonist of calcineurin. Cell Death Differ 17(11):1785–1794. https://doi.org/10.1038/cdd.2010.61
Frank S, Gaume B, Bergmann-Leitner ES, Leitner WW, Robert EG, Catez F, Smith CL, Youle RJ (2001) The role of dynamin-related protein 1, a mediator of mitochondrial fission, in apoptosis. Dev Cell 1(4):515–525
Frezza C, Cipolat S, Martins de Brito O, Micaroni M, Beznoussenko GV, Rudka T, Bartoli D, Polishuck RS et al (2006) OPA1 controls apoptotic cristae remodeling independently from mitochondrial fusion. Cell 126(1):177–189. https://doi.org/10.1016/j.cell.2006.06.025
Elachouri G, Vidoni S, Zanna C, Pattyn A, Boukhaddaoui H, Gaget K, Yu-Wai-Man P, Gasparre G et al (2011) OPA1 links human mitochondrial genome maintenance to mtDNA replication and distribution. Genome Res 21(1):12–20. https://doi.org/10.1101/gr.108696.110
Olichon A, Baricault L, Gas N, Guillou E, Valette A, Belenguer P, Lenaers G (2003) Loss of OPA1 perturbates the mitochondrial inner membrane structure and integrity, leading to cytochrome c release and apoptosis. J Biol Chem 278(10):7743–7746. https://doi.org/10.1074/jbc.C200677200
Mizushima N (2005) The pleiotropic role of autophagy: from protein metabolism to bactericide. Cell Death Differ 12(Suppl 2):1535–1541. https://doi.org/10.1038/sj.cdd.4401728
Klionsky DJ, Emr SD (2000) Autophagy as a regulated pathway of cellular degradation. Science 290(5497):1717–1721
Wu YT, Tan HL, Huang Q, Kim YS, Pan N, Ong WY, Liu ZG, Ong CN et al (2008) Autophagy plays a protective role during zVAD-induced necrotic cell death. Autophagy 4(4):457–466
Cecconi F, Levine B (2008) The role of autophagy in mammalian development: cell makeover rather than cell death. Dev Cell 15(3):344–357. https://doi.org/10.1016/j.devcel.2008.08.012
White KE, Davies VJ, Hogan VE, Piechota MJ, Nichols PP, Turnbull DM, Votruba M (2009) OPA1 deficiency associated with increased autophagy in retinal ganglion cells in a murine model of dominant optic atrophy. Invest Ophthalmol Vis Sci 50(6):2567–2571. https://doi.org/10.1167/iovs.08-2913
Kane MS, Alban J, Desquiret-Dumas V, Gueguen N, Ishak L, Ferre M, Amati-Bonneau P, Procaccio V et al (2017) Autophagy controls the pathogenicity of OPA1 mutations in dominant optic atrophy. J Cell Mol Med 21(10):2284–2297. https://doi.org/10.1111/jcmm.13149
Gomes LC, Scorrano L (2011) Mitochondrial elongation during autophagy: a stereotypical response to survive in difficult times. Autophagy 7(10):1251–1253. https://doi.org/10.4161/auto.7.10.16771
Gomes LC, Scorrano L (2013) Mitochondrial morphology in mitophagy and macroautophagy. Biochim Biophys Acta 1833(1):205–212. https://doi.org/10.1016/j.bbamcr.2012.02.012
Hackenbrock CR (1968) Chemical and physical fixation of isolated mitochondria in low-energy and high-energy states. Proc Natl Acad Sci U S A 61(2):598–605
Pidoux G, Witczak O, Jarnaess E, Myrvold L, Urlaub H, Stokka AJ, Kuntziger T, Tasken K (2011) Optic atrophy 1 is an A-kinase anchoring protein on lipid droplets that mediates adrenergic control of lipolysis. EMBO J 30(21):4371–4386. https://doi.org/10.1038/emboj.2011.365
Seo BB, Nakamaru-Ogiso E, Flotte TR, Matsuno-Yagi A, Yagi T (2006) In vivo complementation of complex I by the yeast Ndi1 enzyme. Possible application for treatment of Parkinson disease. J Biol Chem 281(20):14250–14255. https://doi.org/10.1074/jbc.M600922200
Marella M, Seo BB, Yagi T, Matsuno-Yagi A (2009) Parkinson's disease and mitochondrial complex I: a perspective on the Ndi1 therapy. J Bioenerg Biomembr 41(6):493–497. https://doi.org/10.1007/s10863-009-9249-z
Seo BB, Nakamaru-Ogiso E, Cruz P, Flotte TR, Yagi T, Matsuno-Yagi A (2004) Functional expression of the single subunit NADH dehydrogenase in mitochondria in vivo: a potential therapy for complex I deficiencies. Hum Gene Ther 15(9):887–895. https://doi.org/10.1089/hum.2004.15.887
Yu Z, Zhang Y, Liu N, Yuan J, Lin L, Zhuge Q, Xiao J, Wang X (2016) Roles of neuroglobin binding to mitochondrial complex III subunit cytochrome c1 in oxygen-glucose deprivation-induced neurotoxicity in primary neurons. Mol Neurobiol 53(5):3249–3257. https://doi.org/10.1007/s12035-015-9273-4
Ma WW, Hou CC, Zhou X, Yu HL, Xi YD, Ding J, Zhao X, Xiao R (2013) Genistein alleviates the mitochondria-targeted DNA damage induced by beta-amyloid peptides 25-35 in C6 glioma cells. Neurochem Res 38(7):1315–1323. https://doi.org/10.1007/s11064-013-1019-y
Hawkins PT, Anderson KE, Davidson K, Stephens LR (2006) Signalling through class I PI3Ks in mammalian cells. Biochem Soc Trans 34(Pt 5):647–662. https://doi.org/10.1042/BST0340647
Anderson CN, Tolkovsky AM (1999) A role for MAPK/ERK in sympathetic neuron survival: protection against a p53-dependent, JNK-independent induction of apoptosis by cytosine arabinoside. J Neurosci 19(2):664–673
de Oliveira MR, Ferreira GC, Schuck PF, Dal Bosco SM (2015) Role for the PI3K/Akt/Nrf2 signaling pathway in the protective effects of carnosic acid against methylglyoxal-induced neurotoxicity in SH-SY5Y neuroblastoma cells. Chem Biol Interact 242:396–406. https://doi.org/10.1016/j.cbi.2015.11.003
Le Belle JE, Orozco NM, Paucar AA, Saxe JP, Mottahedeh J, Pyle AD, Wu H, Kornblum HI (2011) Proliferative neural stem cells have high endogenous ROS levels that regulate self-renewal and neurogenesis in a PI3K/Akt-dependant manner. Cell Stem Cell 8(1):59–71. https://doi.org/10.1016/j.stem.2010.11.028
Zhang Q, Liu G, Wu Y, Sha H, Zhang P, Jia J (2011) BDNF promotes EGF-induced proliferation and migration of human fetal neural stem/progenitor cells via the PI3K/Akt pathway. Molecules 16(12):10146–10156. https://doi.org/10.3390/molecules161210146
Zhao J, Cheng YY, Fan W, Yang CB, Ye SF, Cui W, Wei W, Lao LX et al (2015) Botanical drug puerarin coordinates with nerve growth factor in the regulation of neuronal survival and neuritogenesis via activating ERK1/2 and PI3K/Akt signaling pathways in the neurite extension process. CNS Neurosci Ther 21(1):61–70. https://doi.org/10.1111/cns.12334
Nguyen TL, Kim CK, Cho JH, Lee KH, Ahn JY (2010) Neuroprotection signaling pathway of nerve growth factor and brain-derived neurotrophic factor against staurosporine induced apoptosis in hippocampal H19-7/IGF-IR [corrected]. Exp Mol Med 42(8):583–595. https://doi.org/10.3858/emm.2010.42.8.060
Lotfinia M, Kadivar M, Piryaei A, Pournasr B, Sardari S, Sodeifi N, Sayahpour FA, Baharvand H (2016) Effect of secreted molecules of human embryonic stem cell-derived mesenchymal stem cells on acute hepatic failure model. Stem Cells Dev 25(24):1898–1908. https://doi.org/10.1089/scd.2016.0244
Zagoura DS, Roubelakis MG, Bitsika V, Trohatou O, Pappa KI, Kapelouzou A, Antsaklis A, Anagnou NP (2012) Therapeutic potential of a distinct population of human amniotic fluid mesenchymal stem cells and their secreted molecules in mice with acute hepatic failure. Gut 61(6):894–906. https://doi.org/10.1136/gutjnl-2011-300908
Toma C, Pittenger MF, Cahill KS, Byrne BJ, Kessler PD (2002) Human mesenchymal stem cells differentiate to a cardiomyocyte phenotype in the adult murine heart. Circulation 105(1):93–98
Na HK, Kim EH, Jung JH, Lee HH, Hyun JW, Surh YJ (2008) (−)-Epigallocatechin gallate induces Nrf2-mediated antioxidant enzyme expression via activation of PI3K and ERK in human mammary epithelial cells. Arch Biochem Biophys 476(2):171–177. https://doi.org/10.1016/j.abb.2008.04.003
Liu J, Yu Z, Guo S, Lee SR, Xing C, Zhang C, Gao Y, Nicholls DG et al (2009) Effects of neuroglobin overexpression on mitochondrial function and oxidative stress following hypoxia/reoxygenation in cultured neurons. J Neurosci Res 87(1):164–170. https://doi.org/10.1002/jnr.21826
Duong TT, Witting PK, Antao ST, Parry SN, Kennerson M, Lai B, Vogt S, Lay PA et al (2009) Multiple protective activities of neuroglobin in cultured neuronal cells exposed to hypoxia re-oxygenation injury. J Neurochem 108(5):1143–1154. https://doi.org/10.1111/j.1471-4159.2008.05846.x
Yu Z, Xu J, Liu N, Wang Y, Li X, Pallast S, van Leyen K, Wang X (2012) Mitochondrial distribution of neuroglobin and its response to oxygen-glucose deprivation in primary-cultured mouse cortical neurons. Neuroscience 218:235–242. https://doi.org/10.1016/j.neuroscience.2012.05.054
Fiocchetti M, Cipolletti M, Leone S, Naldini A, Carraro F, Giordano D, Verde C, Ascenzi P et al (2016) Neuroglobin in breast cancer cells: effect of hypoxia and oxidative stress on protein level, localization, and anti-apoptotic function. PLoS One 11(5):e0154959. https://doi.org/10.1371/journal.pone.0154959
De Marinis E, Fiocchetti M, Acconcia F, Ascenzi P, Marino M (2013) Neuroglobin upregulation induced by 17beta-estradiol sequesters cytocrome c in the mitochondria preventing H2O2-induced apoptosis of neuroblastoma cells. Cell Death Dis 4:e508. https://doi.org/10.1038/cddis.2013.30
Gorgun FM, Zhuo M, Singh S, Englander EW (2014) Neuroglobin mitigates mitochondrial impairments induced by acute inhalation of combustion smoke in the mouse brain. Inhal Toxicol 26(6):361–369. https://doi.org/10.3109/08958378.2014.902147
Cabezas R, Vega-Vela NE, Gonzalez-Sanmiguel J, Gonzalez J, Esquinas P, Echeverria V, Barreto GE (2018) PDGF-BB preserves mitochondrial morphology, attenuates ROS production, and upregulates neuroglobin in an astrocytic model under rotenone insult. Mol Neurobiol 55(4):3085–3095. https://doi.org/10.1007/s12035-017-0567-6
Jin K, Mao X, Xie L, Greenberg DA (2012) Interactions between vascular endothelial growth factor and neuroglobin. Neurosci Lett 519(1):47–50. https://doi.org/10.1016/j.neulet.2012.05.018
Zhu L, Huang L, Wen Q, Wang T, Qiao L, Jiang L (2017) Recombinant human erythropoietin offers neuroprotection through inducing endogenous erythropoietin receptor and neuroglobin in a neonatal rat model of periventricular white matter damage. Neurosci Lett 650:12–17. https://doi.org/10.1016/j.neulet.2017.03.024
Acknowledgments
The authors thank Dr. Jorge Andrés Afanador and the staff of the cosmetic surgery Clinic DHARA in Bogotá, Colombia, for the adipose tissue samples. This work was supported in part by grants PUJ IDs 6260 and 7115 to GEB and 6278 to JG and scholarship for doctoral studies awarded by the Vicerrectoría Académica of PUJ to EB.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
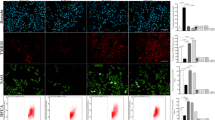
Fig. S1
(DOCX 364 kb)
Rights and permissions
About this article
Cite this article
Baez-Jurado, E., Guio-Vega, G., Hidalgo-Lanussa, O. et al. Mitochondrial Neuroglobin Is Necessary for Protection Induced by Conditioned Medium from Human Adipose-Derived Mesenchymal Stem Cells in Astrocytic Cells Subjected to Scratch and Metabolic Injury. Mol Neurobiol 56, 5167–5187 (2019). https://doi.org/10.1007/s12035-018-1442-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-018-1442-9