Abstract
The endocannabinoid system (ECS) actively participates in several physiological processes within the central nervous system. Among such, its involvement in the downregulation of the N-methyl-D-aspartate receptor (NMDAr) through a modulatory input at the cannabinoid receptors (CBr) has been established. After its production via the kynurenine pathway (KP), quinolinic acid (QUIN) can act as an excitotoxin through the selective overactivation of NMDAr, thus participating in the onset and development of neurological disorders. In this work, we evaluated whether the pharmacological inhibition of fatty acid amide hydrolase (FAAH) by URB597, and the consequent increase in the endogenous levels of anandamide, can prevent the excitotoxic damage induced by QUIN. URB597 (0.3 mg/kg/day × 7 days, administered before, during and after the striatal lesion) exerted protective effects on the QUIN-induced motor (asymmetric behavior) and biochemical (lipid peroxidation and protein carbonylation) alterations in rats. URB597 also preserved the structural integrity of the striatum and prevented the neuronal loss (assessed as microtubule-associated protein-2 and glutamate decarboxylase localization) induced by QUIN (1 μL intrastriatal, 240 nmol/μL), while modified the early localization patterns of CBr1 (CB1) and NMDAr subunit 1 (NR1). Altogether, these findings support the concept that the pharmacological manipulation of the endocannabinoid system plays a neuroprotective role against excitotoxic insults in the central nervous system.







Similar content being viewed by others
References
Zádori D, Klivényi P, Szalárdy L, Fülöp F, Toldi J, Vécsei L (2012) Mitochondrial disturbances, excitotoxicity, neuroinflammation and kynurenines: novel therapeutic strategies for neurodegenerative disorders. J Neurol Sci 322:187–191
Essa M, Braidy N, Vijayan K, Subash S, Guillemin G (2013) Excitotoxicity in the pathogenesis of autism. Neurotox Res J 23:393–400
Iacobucci G, Popescu G (2017) NMDA receptors: linking physiological output to biophysical operation. Nat Rev Neurosci 18:236–249
Rami A, Ferger D, Krieglstein J (1997) Blockade of calpain proteolytic activity rescues neurons from glutamate excitotoxicity. Neurosci Res 27:93–97
Majewski M, Kozlowska A, Thoene M, Lepiarczyk E, Grzegorzewski W (2016) Overview of the role of vitamins and minerals on the kynurenine pathway in health and disease. J Physiol Pharmacol 67:3–19
Pérez-De La Cruz V, Konigsberg M, Santamaría A (2007) Kynurenine pathway and disease: an overview. CNS Neurol Disord Drug Targets 6:398–410
Ghorayeb I, Bezard E, Fernagut P, Bioulac B, Tison F (2005) Animal models of parkinsonism. Rev Neurol (Paris) 161:907–915
Ramaswamy S, McBride J, Kordower J (2007) Animal models of Huntington’s disease. ILAR J 48:356–373
More S, Kumar H, Cho D, Yun Y, Choi D (2016) Toxin-induced experimental models of learning and memory impairment. Int J Mol Sci 17:E1447
Stone T, Mackay G, Forrest C, Clark C, Darlington L (2003) Tryptophan metabolites and brain disorders. Clin Chem Lab Med 41:852–859
Braidy N, Grant R, Adams S, Brew B, Guillemin G (2009) Mechanism for quinolinic acid cytotoxicity in human astrocytes and neurons. Neurotox Res J 16:77–86
Pérez-De La Cruz V, Elinos-Calderón D, Carrillo-Mora P, Silvia-Adaya D, Konigsberg M, Morán J, Ali S, Chánez-Cárdenas M et al (2010) Time-course correlation of early toxic events in three models of striatal damage: modulation by proteases inhibition. Neurochem Int 56:834–842
Howlett AC, Barth F, Bonner TI, Cabral G, Casellas P, Devane WA, Felder CC, Herkenham M et al (2002) International Union of Pharmacology. XXVII . Classification of cannabinoid receptors. Pharmacol Rev 54:161–202
Kendall D, Yudowski G (2016) Cannabinoid receptors in the central nervous system: their signaling and roles in disease. Front Cell Neurosci 10:294
Ashton J, Friberg D, Darlington C, Smith P (2006) Expression of the cannabinoid CB2 receptor in the rat cerebellum: an immunohistochemical study. Neuroscience 396:113–116
Lauckner J, Hille B, Mackie K (2005) The cannabinoid agonist WIN55,212-2 increases intracellular calcium via CB1 receptor coupling to Gq/11 G proteins. Proc Natl Acad Sci 102:19144–19149
Basavarajappa B, Shivakumar M, Joshi V, Subbanna S (2017) Endocannabinoid system in neurodegenerative disorders. J Neurochem 142:624–648
De Petrocellis L, Cascio M, Di Marzo V (2004) The endocannabionid system: a general view and latest additions. Br J Pharmacol 141:765–774
Palazuelos J, Aguado T, Pazos M, Julien B, Carrasco C, Resel E, Sagredo O, Benito C et al (2009) Microglial CB2 cannabinoid receptors are neuroprotective in Huntington’s disease excitotoxicity. Brain 132:3152–3164
Fowler C (2006) The cannabinoid system and its pharmacological manipulation—a review, with emphasis upon the uptake and hydrolysis of anandamide. Fundam Clin Pharmacol 20(6):549–562
Hillard C, Jarrahian A (2003) Cellular accumulation of anandamide: consensus and controversy. Brain J Pharmacol 140:802–808
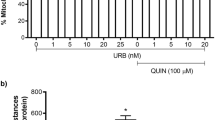
Maya-López M, Ruiz-Contreras H, de Jesús Negrete-Ruiz M, Martínez-Sánchez J, Benítez-Valenzuela J, Colín-González A, Villeda-Hernández J et al (2017) URB597 reduces biochemical, behavioral and morphological alterations in two neurotoxic models in rats. Biomed Pharmacother 88:745–753
Pelicao R, Santos M, Freitas-Lima L, Meyrelles S, Vasquez E, Nakamura-Palacios E, Rodrigues L (2016) URB597 inhibits oxidative stress induced by alcohol binging in the prefrontal cortex of adolescent rats. Neurosci Lett 15:17–22
Nazari M, Komaki A, Karamian R, Shahidi S, Sarihi A, Asadbegi M (2016) The interactive role of CB1 and GABA B receptors in hippocampal synaptic plasticity in rats. Brain Res Bull 120:123–130
Sánchez-Blázquez P, Rodríguez-Muñoz M, Vicente-Sánchez A, Garzón J (2013) Cannabinoid receptors couple to NMDA receptors to reduce the production of NO and the mobilization of zinc induced by glutamate. Antioxid Redox Signal 19(15):1766–1782
Sánchez-Blázquez P, Rodríguez-Muñóz M, Garzón J (2014) The cannabinoid receptor 1 associates with NMDA receptors to produce glutamatergic hypofunction: implications in psychosis and schizophrenia. Front Pharmacol 4:169
Rodríguez-Muños M, Sánchez-Blázquez P, Merlos M, Garzón-Niño J (2016) Endocannabinoid control of glutamate NMDA receptors: the therapeutic potential and consequences of dysfunction. Oncotarget 34:55840–55862
O’Sullivan S (2007) Cannabinoids go nuclear: evidence for activation of peroxisome proliferator-activated receptors. Br J Pharmacol 152:576–582
O’Sullivan S (2016) An update on PPAR activation by cannabinoids. Br J Pharmacol 12:1899–1910
Escamilla-Ramírez A, García E, Palencia-Hernández G, Colín-González A, Galván-Arzate S, Túnez I, Sotelo J, Santamaría A (2017) URB597 and the cannabinoid WIN55,212-2 reduce behavioral and neurochemical deficits induced by MPTP in mice: possible role of redox modulation and NMDA receptors. Neurotox Res 34:532–544
Colín-González A, Orozco-Ibarra M, Chánez-Cárdenas M, Rangel-López E, Santamaría A, Pedraza-Chaverri J, Barrera-Oviedo D, Maldonado P (2013) Heme oxygenase-1 (HO-1) upregulation delays morphological and oxidative damage induced in an excitotoxic/pro-oxidabt model in the rat striatum. Neuroscience 12:91–101
Paxinos G, Watson C (1998) The rat brain in stereotaxic coordinates, 4th ed. Academic Press
Borlongan C, Randall T, Cahill D, Sanberg P (1995) Asymmetrical motor behavior in rats with unilateral striatal excitotoxic lesions as revealed by the elevated body swing test. Brain Res 676:231–234
González R, Woods R (2008) Digital image processing, 3rd edn. Pearson Prentice Hall, USA
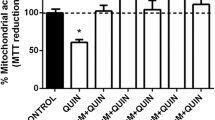
Rangel-López E, Colín-González A, Paz-Loyola A, Pinzón E, Torres I, Serratos I, Castellanos P, Wajner M et al (2015) Cannabinoid receptor agonists reduce the short-term mitochondrial dysfunction and oxidative stress linked to excitotoxicity in the rat brain. Neuroscience 285:97–106
Dunbar J, Hitchcock K, Latimer M, Rugg E, Ward N, Winn P (1992) Exctitotoxic lesions of the pedunculopontine tegmental nucleus of the rat. II. Examination of eating and drinking, rotation, and reaching and grasping following unilateral ibotenate of quinolinate lesions. Brain Res 589:194–206
Trigo-Damas I, Del Rey N, Blesa J (2018) Novel models for Parkinson’s disease and their impact on future drug discovery. Expert Opin Drug Discovery 13:229–239
Santamaría A, Salvatierra-Sánchez R, Vázquez-Román B, Santiago-López D, Villeda-Hernández J, Galván-Arzate S, Jiménez-Capdeville M et al (2003) Protective effects of the antioxidant selenium on quinolinic acid-induced neurotoxicity in rats: In vitro and in vivo studies. J Neurochem 86:479–488
Holley S, Joshi P, Parievsky A, Galvan L, Chen J, Fisher Y, Huynh M, Cepeda C et al (2015) Enhanced GABAergic inputs contribute to functional alterations of cholinergic interneurons in the R6/2 mouse model of Huntington’s disease. eNeuro 2:e0008
Kerr S, Armati P, Guillemin G, Brew B (1998) Chronic exposure of human neurons to quinolonic acid results in neuronal changes consistent with AIDS dementia complex. AIDS 5:355–363
Qin Y, Soghomonian J, Chesselet M (1992) Effects of quinolinic acid on messenger RNAs encoding somatostatin and glutamic acid decarboxylases in the striatum of adult rats. Exp Neurol 115:200–211
Santana-Martínez R, Galván-Arzáte S, Hernández-Pando R, Chánez-Cárdenaz M, Avila-Chávez E, López-Acosta G, Pedraza-Chaverrí J, Santamaría A et al (2014) Sulphoraphane reduces the alterations induced by quinolinic acid: Modulation of glutathione levels. Neuroscience 272:188–198
Rios C, Santamaría A (1991) Quinolinic acid is a potent lipid peroxidant in rat brain homogenates. Neurochem Res 16:1139–1143
Santamaría A, Galván-Arzate S, Lisý V, Ali S, Duhart H, Osorio-Rico L, Ríos C, St’astný F (2001) Quinolinic acid induces oxidative stress in rat brain synaptosomes. Neuroreport 12:871–874
Rodríguez-Martínez E, Camacho A, Maldonado P, Pedraza-Chaverrí J, Santamaría D, Galván-Arzate S, Santamaría A (2000) Effect of quinolinic acid on endogenous antioxidants in rat corpus striatum. Brain Res 858:436–439
Howlett A, Abood M (2017) CB1 and CB2 receptor pharmacology. Adv Pharmacol 80:169–206
Casteels C, Martinez E, Bormans G, Camon L, de Vera N, Baekelandt V, Planas A, Laere K (2010) Type 1 cannabinoid receptor mapping with [18F]MK-9470 PET in the rat brain after quinolinic acid lesion: a comparison to dopamine receptors and glucose metabolism. Eur J Nucl Med Mol Imaging 37:2354–2363
Dowie M, Howard M, Nicholson L, Faull R, Hannan A, Glass M (2010) Behavioural and molecular consequences of chronic cannabinoid treatment in Huntington’s disease transgenic mice. Neuroscience 170:324–336
Sagredo O, Pazos M, Valdeolivas S, Fernández-Ruiz J (2012) Cannabinoids: novel medicines for the treatment of Huntington’s disease. Recent Patents CNS Drug Discov 7:41–48
Pintor A, Tebano M, Martire A, Grieco R, Galluzzo M, Scattoni M, Pézzola A, Cocurello R et al (2006) The cannabinoid receptor agonists WIN 55,212-2 attenuates the effects induced by quinolinic acid in the rat striatum. Neuropharmacology 51:1004–1012
Chiarlone A, Bellocchio L, Blázquez C, Resel E, Soria-Gómez E, Cannich A, Ferrero J, Sagredo O et al (2014) A restricted population of CB1 cannabinoid receptors with neuroprotective activity. Proc Natl Acad Sci Press 111:8257–8262
Diaz-Alonso J, Paraíso-Luna J, Navarrete C, del Rïo C, Cantarero I, Palomares B, Aguareles J, Fernández-Ruiz J et al (2016) VCE-003.2, a novel cannabigerol derivative, enhances neuronal progenitor cell survival and alleviates symptomatology in murine models of Huntington’s disease. Sci Rep 6:29789
Rodríguez-Muñoz M, Cortés-Montero E, Pozo-Rodrigálvarez A, Sánchez-Blázquez P, Garzón-Niño J (2015) The ON:OFF switch, σ1R-HINT1 protein, controls GPCR-NMDA receptor cross-regulation: Implications in neurological disorders. Oncotarget 6:35458–35477
Panlilio LV, Justinova Z, Goldberg SR (2010) Animal models of cannabinoid reward. Br J Pharmacol 160:499–510
Acknowledgements
Gabriela Aguilera-Portillo presents this article as the first author as it encompasses her work and efforts to obtain a Ph.D. degree at the Universidad Autónoma Metropolitana-Iztapalapa (Mexico). Authors express sincere gratitude to the Programa de Posgrado en Biología Experimental from the Universidad Autónoma Metropolitana-Iztapalapa for all the support provided throughout this study. We gratefully acknowledge the technical assistance of Dr. Ana Laura Colín-González. We also thank to the TUBITAK-SBAG (Project No.: 315S088).
Funding
This work was supported by CONACyT-TUBITAK Grant 265991 (A.S.). Gabriela Aguilera-Portillo received a scholarship from CONACyT (CVU486539).
Author information
Authors and Affiliations
Contributions
GAP, AC, CK, IT, MK, and AS conceived and designed the experiments. GAP, ERL, JVH, GP, and AS performed the experiments and analyzed the data. GAP and AS wrote the paper. ÇK, ZE, AC, MK, GAP, and AS developed the theory and contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no competing interests.
Research Involving Animals
Procedures carried out with animals were strictly developed to comply with the local guidelines for the use and care of laboratory animals (Norma Oficial Mexicana NOM-062-ZOO-2001), and the “Guidelines for the Use of Animals in Neuroscience Research” from the Society of Neuroscience. All experiments performed were timely approved by the Ethics Committee of the Instituto Nacional de Neurología y Neurocirugía. All efforts were made to minimize animal suffering during the experiments.
Rights and permissions
About this article
Cite this article
Aguilera-Portillo, G., Rangel-López, E., Villeda-Hernández, J. et al. The Pharmacological Inhibition of Fatty Acid Amide Hydrolase Prevents Excitotoxic Damage in the Rat Striatum: Possible Involvement of CB1 Receptors Regulation. Mol Neurobiol 56, 844–856 (2019). https://doi.org/10.1007/s12035-018-1129-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-018-1129-2