Abstract
Angiogenesis is the physiological process that results in the formation of new blood vessels develop from pre-existing vasculature and plays a significant role in several physiological and pathological processes. Inhibiting angiogenesis, a crucial mechanism in the growth and metastasis of cancer, has been proposed as a potential anticancer therapy. Different studies showed the beneficial effects of angiogenesis inhibitors either in patients suffering from different cancers, alone or in combination with conventional therapies. Even though there are currently a number of efficient anti-angiogenic drugs, including monoclonal antibodies and kinase inhibitors, the associated toxicity profile and their affordability constraints are prompting researchers to search for a safe and affordable angiostatic agent for cancer treatment. Endostatin is one of the endogenous anti-angiogenic candidates that have been extensively pursued for the treatment of cancer, but even over three decades after its discovery, we have not made much advancement in employing it as an anticancer therapeutic despite of its remarkable anti-angiogenic effect with low toxicity profile. A recombinant human endostatin (rh-Es) variant for non-small cell lung cancer was approved by China in 2006 and has since been used effectively. Several other successful clinical trials related to endostatin for various malignancies are either ongoing or have already been completed with promising results. Thus, in this review, we have provided an overview of existing anti-angiogenic drugs developed for cancer therapy, with a summary of tumour angiogenesis in the context of Endostatin, and clinical status of rh-Es in cancer treatment. Furthermore, we briefly discuss the various strategies to improve endostatin features (poor pharmacokinetic properties) for developing rh-Es as a safe and effective agent for cancer treatment.
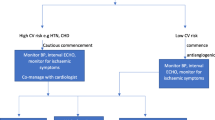
Graphical abstract






Similar content being viewed by others
Data availability
No data was used for the research described in the article.
Consent to publish
Not applicable.
Abbreviations
- Bfgf:
-
Basic fibroblast growth factor
- CBR:
-
Clinical beneficial rate
- EC:
-
Endothelial cells
- ECM:
-
Extracellular matrix
- FDA:
-
Food and Drug Administration
- FGF:
-
Fibroblast growth factor
- HCC:
-
Hepatocellular carcinoma
- HIF:
-
Hypoxia-inducible factor
- HELP:
-
Half-life extension partners
- IFN:
-
Interferon
- KI:
-
Kinase inhibitor
- mAb:
-
Monoclonal antibodies
- MMP:
-
Matrix metalloproteinase
- NMPA:
-
National Medical Products Administration
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
- PCH:
-
Pulmonary capillary hemangiomatosis
- PEG:
-
Polyethylene glycol
- PK:
-
Pharmacokinetic
- rh-Es:
-
Recombinant human endostatin
- RPLS:
-
Reversible posterior leukoencephalopathy syndrome
- RNA:
-
Ribonucleic acids
- SFDA:
-
State Food and Drug Administration of China
- SPARC:
-
Secreted Protein Acidic And Cysteine Rich
- TGF:
-
Transforming growth factor
- TNF:
-
Tumour necrosis factor
- TS-2:
-
Transglutaminase-2
- TSP-1:
-
Thrombospondin-1
- VEGF:
-
Vascular endothelial growth factor
References
Tumour-National Cancer Institute (NCI) dictionary of cancer terms. NCI; 2023. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/tumour. Accessed 3 March 2023.
WHO. Cancer. World Health Organization (WHO); 2023. https://www.who.int. Accessed 3 March 2023.
Upadhyay A. Cancer: An unknown territory; rethinking before going ahead. Genes Dis. 2021;8(5):655–61.
Luzzi KJ, MacDonald IC, Schmidt EE, et al. Multistep nature of metastatic inefficiency: dormancy of solitary cells after successful extravasation and limited survival of early micrometastases. Am J Pathol. 1998;153(3):865–73.
Jones S, Chen WD, Parmigiani G, et al. Comparative lesion sequencing provides insights into tumor evolution. Proc Natl Acad Sci USA. 2008;105(11):4283–8.
Joensuu H. Systemic chemotherapy for cancer: from weapon to treatment. Lancet Oncol. 2008;9(3):304–304.
Borghaei H, Smith MR, Campbell KS. Immunotherapy of cancer. Eur J Pharmacol. 2009;625(1–3):41–54.
Baskar R, Lee KA, Yeo R, Yeoh KW. Cancer and radiation therapy: current advances and future directions. Int J Med Sci. 2012;9(3):193–9.
El-Kenawi AE, El-Remessy AB. Angiogenesis inhibitors in cancer therapy: mechanistic perspective on classification and treatment rationales. Br J Pharmacol. 2013;170(4):712–29.
Ke X, Shen L. Molecular targeted therapy of cancer: the progress and future prospect. Front Lab Med. 2017;1(2):69–75.
Abraham J, Ocen J, Staffurth J. Hormonal therapy for cancer. Medicine. 2022;44(1):30–3.
Lacouture M, Sibaud V. Toxic side effects of targeted therapies and immunotherapies affecting the skin, oral mucosa, hair, and nails. Am J Clin Dermatol. 2018;19(Suppl 1):31–9.
Herrmann J. Vascular toxic effects of cancer therapies. Nat Rev Cardiol. 2020;17(8):503–22.
Weis SM, Cheresh DA. Tumor angiogenesis: molecular pathways and therapeutic targets. Nat Med. 2011;17(11):1359–70.
Katayama Y, Uchino J, Chihara Y, et al. Tumor neovascularization and developments in therapeutics. Cancers (Basel). 2019;11(3):316–316.
Folkman J. Tumor angiogenesis. Adv Cancer Res. 1974;19:331–58.
Sun Y, Wang JW, Liu YY, et al. Long-term results of a randomized, double-blind, and placebo-controlled phase III trial: Endostar (rh-endostatin) versus placebo in combination with vinorelbine and cisplatin in advanced non-small cell lung cancer. Thorac Cancer. 2013;4(4):440–8.
Li BL, Hu XL, Zhao XH, Sun HG, Zhou CY, Zhang Y. Endostar combined with irinotecan/calcium folinate/5-fluorouracil (FOLFIRI) for treating advanced colorectal cancer: a clinical study. J Chemother. 2015;27(5):301–6.
Griffioen AW, Dudley AC. The rising impact of angiogenesis research. Angiogenesis. 2022;25(4):435–7.
Nishida N, Yano H, Nishida T, Kamura T, Kojiro M. Angiogenesis in cancer. Vasc Health Risk Manag. 2006;2(3):213–9.
Bussolino F, Mantovani A, Persico G. Molecular mechanisms of blood vessel formation. Trends Biochem Sci. 1997;22(7):251–6.
Gupta MK, Qin RY. Mechanism and its regulation of tumor-induced angiogenesis. World J Gastroenterol. 2003;9(6):1144–55.
Hanahan D, Folkman J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell. 1996;86(3):353–64.
Paku S, Paweletz N. First steps of tumor-related angiogenesis. Lab Investig. 1991;65(3):334–46.
Aspriţoiu VM, Stoica I, Bleotu C, Diaconu CC. Epigenetic regulation of angiogenesis in development and tumors progression: potential implications for cancer treatment. Front Cell Dev Biol. 2021;9: 689962.
Carmeliet P. Angiogenesis in life, disease and medicine. Nature. 2005;438(7070):932–6.
De Spiegelaere W, Casteleyn C, Van den Broeck W, et al. Intussusceptive angiogenesis: a biologically relevant form of angiogenesis [published correction appears in J Vasc Res. 2012;49(5):416]. J Vasc Res. 2012;49(5):390–404.
Karthik S, Djukic T, Kim JD, et al. Synergistic interaction of sprouting and intussusceptive angiogenesis during zebrafish caudal vein plexus development [published correction appears in Sci Rep. 2019 Mar 6;9(1):4152]. Sci Rep. 2018;8(1):9840–9840.
Handsley MM, Edwards DR. Metalloproteinases and their inhibitors in tumor angiogenesis. Int J Cancer. 2005;115(6):849–60.
Ronca R, Benkheil M, Mitola S, Struyf S, Liekens S. Tumor angiogenesis revisited: regulators and clinical implications. Med Res Rev. 2017;37(6):1231–74.
Lugano R, Ramachandran M, Dimberg A. Tumor angiogenesis: causes, consequences, challenges and opportunities. Cell Mol Life Sci. 2020;77(9):1745–70.
Montesano R, Vassalli JD, Baird A, Guillemin R, Orci L. Basic fibroblast growth factor induces angiogenesis in vitro. Proc Natl Acad Sci USA. 1986;83(19):7297–301.
Hashimoto T, Shibasaki F. Hypoxia-inducible factor as an angiogenic master switch. Front Pediatr. 2015;3:33–33.
Gopinathan G, Milagre C, Pearce OM, et al. Interleukin-6 stimulates defective angiogenesis. Cancer Res. 2015;75(15):3098–107.
Kopec M, Abramczyk H. The role of pro- and antiangiogenic factors in angiogenesis process by Raman spectroscopy. Spectrochim Acta A. 2022;268: 120667.
Cook KM, Figg WD. Angiogenesis inhibitors: current strategies and future prospects. CA Cancer J Clin. 2010;60(4):222–43.
Ide AG. Vascularization of the Brown-Pearce rabbit epithelioma transplant as seen in the transparent ear chamber. Am J Roentgenol. 1939;42:891–891.
Ribatti D, Vacca A, Dammacco F. The role of the vascular phase in solid tumor growth: a historical review. Neoplasia. 1999;1(4):293–302.
Li T, Kang G, Wang T, Huang H. Tumor angiogenesis and anti-angiogenic gene therapy for cancer. Oncol Lett. 2018;16(1):687–702.
Brouty-Boyé D, Zetter BR. Inhibition of cell motility by interferon. Science. 1980;208(4443):516–8.
Ezekowitz RA, Mulliken JB, Folkman J. Interferon alfa-2a therapy for life-threatening hemangiomas of infancy [published correction appears in N Engl J Med 1994 Jan 27;330(4):300] [published correction appears in N Engl J Med 1994 Jan 27;330(4):300]. N Engl J Med. 1992;326(22):1456–63.
Kaban LB, Mulliken JB, Ezekowitz RA, Ebb D, Smith PS, Folkman J. Antiangiogenic therapy of a recurrent giant cell tumor of the mandible with interferon alfa-2a. Pediatrics. 1999;103(6 Pt 1):1145–9.
Kaban LB, Troulis MJ, Ebb D, August M, Hornicek FJ, Dodson TB. Antiangiogenic therapy with interferon alpha for giant cell lesions of the jaws. J Oral Maxillofac Surg. 2002;60(10):1103–13.
Ginns LC, Roberts DH, Mark EJ, Brusch JL, Marler JJ. Pulmonary capillary hemangiomatosis with atypical endotheliomatosis: successful antiangiogenic therapy with doxycycline. Chest. 2003;124(5):2017–22.
National Library of Medicine-National Center for Biotechnology. Information-Interferon. National Library of Medicine-National Center for Biotechnology; 2023. https://www.ncbi.nlm.nih.gov/books/NBK555932/. Accessed 2 Feb 2023.
National Cancer Institute. Angiogenesis inhibitors. National Cancer Institute; 2023. https://www.cancer.gov/. Accessed 4 Feb 2023.
Zirlik K, Duyster J. Anti-angiogenics: current situation and future perspectives. Oncol Res Treat. 2018;41(4):166–71.
Collett MS, Erikson RL. Protein kinase activity associated with the avian sarcoma virus src gene product. Proc Natl Acad Sci USA. 1978;75(4):2021–4.
Bhullar KS, Lagarón NO, McGowan EM, et al. Kinase-targeted cancer therapies: progress, challenges and future directions. Mol Cancer. 2018;17(1):48–48.
Karaman MW, Herrgard S, Treiber DK, et al. A quantitative analysis of kinase inhibitor selectivity. Nat Biotechnol. 2008;26(1):127–32.
Vaughn C, Zhang L, Schiff D. Reversible posterior leukoencephalopathy syndrome in cancer. Curr Oncol Rep. 2008;10(1):86–91.
Raina S, Mahesh D, Rajendra G, Chauhan NS. Reversible posterior leukoencephalopathy syndrome. J Neurosci Rural Pract. 2012;3(2):222–4.
Myint ZW, Sen JM, Watts NL, et al. Reversible posterior leukoencephalopathy syndrome during regorafenib treatment: a case report and literature review of reversible posterior leukoencephalopathy syndrome associated with multikinase inhibitors. Clin Colorectal Cancer. 2014;13(2):127–30.
Martín G, Bellido L, Cruz JJ. Reversible posterior leukoencephalopathy syndrome induced by sunitinib. J Clin Oncol. 2007;25(23):3559–3559.
Chen A, Agarwal N. Reversible posterior leucoencephalopathy syndrome associated with sunitinib. Int Med J. 2009;39(5):341–2.
Padhy BM, Shanmugam SP, Gupta YK, Goyal A. Reversible posterior leucoencephalopathy syndrome in an elderly male on sunitinib therapy. Br J Clin Pharmacol. 2011;71(5):777–9.
Hadj JO, Braven RD, Tillier C, Schrijver HM, Verheul HM, Van Der Vliet HJ. Reversible posterior leukoencephalopathy syndrome during sunitinib therapy for metastatic renal cell carcinoma. Oncol Lett. 2012;3(6):1293–6.
Rini BI, Escudier B, Tomczak P, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial [published correction appears in Lancet. 2012 Nov 24;380(9856):1818]. Lancet. 2011;378(9807):1931–9.
Rini BI, Tamaskar I, Shaheen P, et al. Hypothyroidism in patients with metastatic renal cell carcinoma treated with sunitinib. J Natl Cancer Inst. 2007;99(1):81–3.
Tamaskar I, Bukowski R, Elson P, et al. Thyroid function test abnormalities in patients with metastatic renal cell carcinoma treated with sorafenib. Ann Oncol. 2008;19(2):265–8.
Baldazzi V, Tassi R, Lapini A, et al. Sunitinib-induced hyperparathyroidism: a possible mechanism to altered bone homeostasis. Cancer. 2012;118(12):3165–72.
Agrillo A, Nastro Siniscalchi E, Facchini A, Filiaci F, Ungari C. Osteonecrosis of the jaws in patients assuming bisphosphonates and sunitinib: two case reports. Eur Rev Med Pharmacol Sci. 2012;16(7):952–7.
Lodish MB. Clinical review: kinase inhibitors: adverse effects related to the endocrine system. J Clin Endocrinol Metab. 2013;98(4):1333–42.
Orphanos GS, Ioannidis GN, Ardavanis AG. Cardiotoxicity induced by tyrosine kinase inhibitors. Acta Oncol. 2009;48(7):964–70.
Shah DR, Shah RR, Morganroth J. Tyrosine kinase inhibitors: their on-target toxicities as potential indicators of efficacy. Drug Saf. 2013;36(6):413–26.
Krämer I, Lipp HP. Bevacizumab, a humanized anti-angiogenic monoclonal antibody for the treatment of colorectal cancer. J Clin Pharm Ther. 2007;32(1):1–14.
Cunningham O, Scott M, Zhou ZS, Finlay WJJ. Polyreactivity and polyspecificity in therapeutic antibody development: risk factors for failure in preclinical and clinical development campaigns. MAbs. 2021;13(1):1999195.
Méndez-Valdés G, Gómez-Hevia F, Lillo-Moya J, et al. Endostatin and cancer therapy: a novel potential alternative to anti-VEGF monoclonal antibodies. Biomedicines. 2023;11(3):718–718.
Sandeep, Shinde SH, Pande AH. Polyspecificity—an emerging trend in the development of clinical antibodies. Mol Immunol. 2023;155:175–183
Wakelee HA, Dahlberg SE, Keller SM, et al. Adjuvant chemotherapy with or without bevacizumab in patients with resected non-small-cell lung cancer (E1505): an open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2017;18(12):1610–23.
Peter S, Hausmann N, Schuster A, Boehm HF. Reversible posterior leukoencephalopathy syndrome and intravenous bevacizumab. Clin Exp Ophthalmol. 2008;36(1):94–6.
Chang Y, Mbeo G, Littman SJ. Reversible posterior leukoencephalopathy syndrome associated with concurrent bevacizumab, gemcitabine, and oxaliplatin for cholangiocarcinoma. J Gastrointest Cancer. 2012;43(3):505–7.
Wang W, Zhao LR, Lin XQ, Feng F. Reversible posterior leukoencephalopathy syndrome induced by bevacizumab plus chemotherapy in colorectal cancer. World J Gastroenterol. 2014;20(21):6691–7.
Eryılmaz MK, Mutlu H, Salim DK, Musri FY, Coşkun HŞ. Fatal posterior reversible leukoencephalopathy syndrome associated coma induced by bevacizumab in metastatic colorectal cancer and review of literature. J Oncol Pharm Pract. 2016;22(6):806–10.
Hernandez I, Bott SW, Patel AS, et al. Pricing of monoclonal antibody therapies: higher if used for cancer? Am J Manag Care. 2018;24(2):109–12.
Kropff MH, Lang N, Bisping G, et al. Hyperfractionated cyclophosphamide in combination with pulsed dexamethasone and thalidomide (HyperCDT) in primary refractory or relapsed multiple myeloma. Br J Haematol. 2003;122(4):607–16.
Miller MT, Strömland KK. What can we learn from the thalidomide experience: an ophthalmologic perspective. Curr Opin Ophthalmol. 2011;22(5):356–64.
Johnson DC, Corthals SL, Walker BA, et al. Genetic factors underlying the risk of thalidomide-related neuropathy in patients with multiple myeloma. J Clin Oncol. 2011;29(7):797–804.
Thoreau F, Chudasama V. Enabling the next steps in cancer immunotherapy: from antibody-based bispecifics to multispecifics, with an evolving role for bioconjugation chemistry. RSC Chem Biol. 2021;3(2):140–69.
Boehm T, Folkman J, Browder T, O’Reilly MS. Antiangiogenic therapy of experimental cancer does not induce acquired drug resistance. Nature. 1997;390(6658):404–7.
Walia A, Yang JF, Huang YH, Rosenblatt MI, Chang JH, Azar DT. Endostatin’s emerging roles in angiogenesis, lymphangiogenesis, disease, and clinical applications. Biochim Biophys Acta. 2015;1850(12):2422–38.
Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med. 1971;285(21):1182–6.
O’Reilly MS, Holmgren L, Chen C, Folkman J. Angiostatin induces and sustains dormancy of human primary tumors in mice. Nat Med. 1996;2(6):689–92.
O’Reilly MS, Holmgren L, Shing Y, et al. Angiostatin: a circulating endothelial cell inhibitor that suppresses angiogenesis and tumor growth. Cold Spring Harb Symp Quant Biol. 1994;59:471–82.
Ribatti D. The history of angiogenesis inhibitors. Leukemia. 2007;21(8):1606–9.
O’Reilly MS, Boehm T, Shing Y, et al. Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell. 1997;88(2):277–85.
Kisker O, Becker CM, Prox D, et al. Continuous administration of endostatin by intraperitoneally implanted osmotic pump improves the efficacy and potency of therapy in a mouse xenograft tumor model. Cancer Res. 2001;61(20):7669–74.
Li K, Shi M, Qin S. Current status and study progress of recombinant human endostatin in cancer treatment. Oncol Ther. 2018;6(1):21–43.
Sasaki T, Fukai N, Mann K, Göhring W, Olsen BR, Timpl R. Structure, function and tissue forms of the C-terminal globular domain of collagen XVIII containing the angiogenesis inhibitor endostatin. EMBO J. 1998;17(15):4249–56.
Sasaki T, Larsson H, Tisi D, Claesson-Welsh L, Hohenester E, Timpl R. Endostatins derived from collagens XV and XVIII differ in structural and binding properties, tissue distribution and anti-angiogenic activity. J Mol Biol. 2000;301(5):1179–90.
Zatterstrom UK, Felbor U, Fukai N, Olsen BR. Collagen XVIII/endostatin structure and functional role in angiogenesis. Cell Struct Funct. 2000;25(2):97–101.
Sasaki T, Hohenester E, Timpl R. Structure and function of collagen-derived endostatin inhibitors of angiogenesis. IUBMB Life. 2002;53(2):77–84.
John H, Forssmann WG. Determination of the disulfide bond pattern of the endogenous and recombinant angiogenesis inhibitor endostatin by mass spectrometry. Rapid Commun Mass Spectrom. 2001;15(14):1222–8.
Han Q, Fu Y, Zhou H, He Y, Luo Y. Contributions of Zn(II)-binding to the structural stability of endostatin. FEBS Lett. 2007;581(16):3027–32.
Felbor U, Dreier L, Bryant RA, Ploegh HL, Olsen BR, Mothes W. Secreted cathepsin L generates endostatin from collagen XVIII. EMBO J. 2000;19(6):1187–94.
Jagodic M, Vrhovec I, Borstnar S, Cufer T. Prognostic and predictive value of cathepsins D and L in operable breast cancer patients. Neoplasma. 2005;52(1):1–9.
Sullivan S, Tosetto M, Kevans D, et al. Localization of nuclear cathepsin L and its association with disease progression and poor outcome in colorectal cancer. Int J Cancer. 2009;125(1):54–61.
Miyamoto K, Iwadate M, Yanagisawa Y, et al. Cathepsin L is highly expressed in gastrointestinal stromal tumors. Int J Oncol. 2011;39(5):1109–15.
Ruan J, Zheng H, Fu W, Zhao P, Su N, Luo R. Increased expression of cathepsin L: a novel independent prognostic marker of worse outcome in hepatocellular carcinoma patients. PLoS ONE. 2014;9(11): 112136.
Wen W, Moses MA, Wiederschain D, Arbiser JL, Folkman J. The generation of endostatin is mediated by elastase. Cancer Res. 1999;59(24):6052–6.
Ferreras M, Felbor U, Lenhard T, Olsen BR, Delaissé J. Generation and degradation of human endostatin proteins by various proteinases. FEBS Lett. 2000;486(3):247–51.
Poluzzi C, Iozzo RV, Schaefer L. Endostatin and endorepellin: a common route of action for similar angiostatic cancer avengers. Adv Drug Deliv Rev. 2016;97:156–73.
Pedram A, Razandi M, Levin ER. Extracellular signal-regulated protein kinase/Jun kinase cross-talk underlies vascular endothelial cell growth factor-induced endothelial cell proliferation. J Biol Chem. 1998;273(41):26722–8.
Kim YM, Hwang S, Kim YM, et al. Endostatin blocks vascular endothelial growth factor-mediated signaling via direct interaction with KDR/Flk-1. J Biol Chem. 2002;277(31):27872–9.
Kowanetz M, Ferrara N. Vascular endothelial growth factor signaling pathways: therapeutic perspective. Clin Cancer Res. 2006;12(17):5018–22.
Han KY, Azar DT, Sabri A, et al. Characterization of the interaction between endostatin short peptide and VEGF receptor 3. Protein Pept Lett. 2012;19(9):969–74.
Wickström SA, Alitalo K, Keski-Oja J. Endostatin associates with integrin alpha5beta1 and caveolin-1, and activates Src via a tyrosyl phosphatase-dependent pathway in human endothelial cells. Cancer Res. 2002;62(19):5580–9.
Thomas S, Overdevest JB, Nitz MD, et al. Src and caveolin-1 reciprocally regulate metastasis via a common downstream signaling pathway in bladder cancer. Cancer Res. 2011;71(3):832–41.
Nah J, Yoo SM, Jung S, et al. Phosphorylated CAV1 activates autophagy through an interaction with BECN1 under oxidative stress. Cell Death Dis. 2017;8(5):2822.
Sasaki T, Larsson H, Kreuger J, et al. Structural basis and potential role of heparin/heparan sulfate binding to the angiogenesis inhibitor endostatin. EMBO J. 1999;18(22):6240–8.
Karumanchi SA, Jha V, Ramchandran R, et al. Cell surface glypicans are low-affinity endostatin receptors. Mol Cell. 2001;7(4):811–22.
Reis RC, Schuppan D, Barreto AC, et al. Endostatin competes with bFGF for binding to heparin-like glycosaminoglycans. Biochem Biophys Res Commun. 2005;333(3):976–83.
Shi H, Huang Y, Zhou H, et al. Nucleolin is a receptor that mediates antiangiogenic and antitumor activity of endostatin. Blood. 2007;110(8):2899–906.
Faye C, Chautard E, Olsen BR, Ricard-Blum S. The first draft of the endostatin interaction network. J Biol Chem. 2009;284(33):22041–7.
Faye C, Inforzato A, Bignon M, et al. Transglutaminase-2: a new endostatin partner in the extracellular matrix of endothelial cells. Biochem J. 2010;427(3):467–75.
Goyanes AM, Moldobaeva A, Marimoutou M, et al. Functional impact of human genetic variants of COL18A1/endostatin on pulmonary endothelium. Am J Respir Cell Mol Biol. 2020;62(4):524–34.
Song N, Ding Y, Zhuo W, et al. The nuclear translocation of endostatin is mediated by its receptor nucleolin in endothelial cells. Angiogenesis. 2012;15(4):697–711.
Good DJ, Polverini PJ, Rastinejad F, et al. A tumor suppressor-dependent inhibitor of angiogenesis is immunologically and functionally indistinguishable from a fragment of thrombospondin. Proc Natl Acad Sci USA. 1990;87(17):6624–8.
Bagavandoss P, Wilks JW. Specific inhibition of endothelial cell proliferation by thrombospondin. Biochem Biophys Res Commun. 1990;170(2):867–72.
Taraboletti G, Roberts D, Liotta LA, Giavazzi R. Platelet thrombospondin modulates endothelial cell adhesion, motility, and growth: a potential angiogenesis regulatory factor. J Cell Biol. 1990;111(2):765–72.
Lawler PR, Lawler J. Molecular basis for the regulation of angiogenesis by thrombospondin-1 and -2. Cold Spring Harb Perspect Med. 2012;2(5):6627.
Dardik R, Inbal A. Complex formation between tissue transglutaminase II (tTG) and vascular endothelial growth factor receptor 2 (VEGFR-2): proposed mechanism for modulation of endothelial cell response to VEGF. Exp Cell Res. 2006;312(16):2973–82.
Shu H, Dong Y, Xu Z, et al. The efficacy and safety of continuous intravenous endostar treatment combined with concurrent chemoradiotherapy in patients with locally advanced cervical squamous cell carcinoma: a randomized controlled trial. Front Oncol. 2021;11: 723193.
Cunningham C, Bolcaen J, Bisio A, Genis A, Strijdom H, Vandevoorde C. Recombinant endostatin as a potential radiosensitizer in the treatment of non-small cell lung cancer. Pharmaceuticals (Basel). 2023;16(2):219–219.
Eder JP Jr, Supko JG, Clark JW, et al. Phase I clinical trial of recombinant human endostatin administered as a short intravenous infusion repeated daily. J Clin Oncol. 2002;20(18):3772–84.
Herbst RS, Hess KR, Tran HT, et al. Phase I study of recombinant human endostatin in patients with advanced solid tumors. J Clin Oncol. 2002;20(18):3792–803.
Thomas JP, Arzoomanian RZ, Alberti D, et al. Phase I pharmacokinetic and pharmacodynamic study of recombinant human endostatin in patients with advanced solid tumors. J Clin Oncol. 2003;21(2):223–31.
Hansma AH, Broxterman HJ, van der Horst I, et al. Recombinant human endostatin administered as a 28-day continuous intravenous infusion, followed by daily subcutaneous injections: a phase I and pharmacokinetic study in patients with advanced cancer. Ann Oncol. 2005;16(10):1695–701.
Kulke MH, Bergsland EK, Ryan DP, et al. Phase II study of recombinant human endostatin in patients with advanced neuroendocrine tumors. J Clin Oncol. 2006;24(22):3555–61.
Whitworth A. Endostatin: are we waiting for Godot? J Natl Cancer Inst. 2006;98(11):731–3.
Fu Y, Tang H, Huang Y, Song N, Luo Y. Unraveling the mysteries of endostatin. IUBMB Life. 2009;61(6):613–26.
Folkman J. Endostatin finds a new partner: nucleolin. Blood J Am Soc Hematol. 2007;110(8):2786–7.
Hurwitz H. Integrating the anti-VEGF-A humanized monoclonal antibody bevacizumab with chemotherapy in advanced colorectal cancer. Clin Colorectal Cancer. 2004;4(Suppl 2):S62–8.
Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350(23):2335–42.
Gasparini G, Longo R, Fanelli M, Teicher BA. Combination of antiangiogenic therapy with other anticancer therapies: results, challenges, and open questions. J Clin Oncol. 2005;23(6):1295–311.
Boehm T, O’reilly MS, Keough K, Shiloach J, Shapiro R, Folkman J. Zinc-binding of endostatin is essential for its antiangiogenic activity. Biochem Biophys Res Commun. 1998;252(1):190–4.
Yang L, Wang JW, Sun Y, et al. Randomized phase II trial on escalated doses of Rh-endostatin (YH-16) for advanced non-small cell lung cancer. Chin J Oncol. 2006;28(2):138–41.
Wang J, Sun Y, Liu Y, et al. Results of randomized, multicenter, double-blind phase III trial of rh-endostatin (YH-16) in treatment of advanced non-small cell lung cancer patients. Zhongguo Fei Ai Za Zhi. 2005;8(4):283–90.
Zhong Q, Tao Y, Chen H, et al. The changing landscape of anti-lung cancer drug clinical trials in mainland China from 2005 to 2020. Lancet Reg Health West Pac. 2021;11:100151–100151.
Jiang XD, Ding MH, Qiao Y, Liu Y, Liu L. Study on lung cancer cells expressing VEGFR2 and the impact on the effect of RHES combined with radiotherapy in the treatment of brain metastases. Clin Lung Cancer. 2014;15(2):e23–9.
Zhang R, Wang ZY, Li YH, et al. Usefulness of dynamic contrast-enhanced magnetic resonance imaging for predicting treatment response to vinorelbine–cisplatin with or without recombinant human endostatin in bone metastasis of non-small cell lung cancer. Am J Cancer Res. 2016;6(12):2890–900.
Xu HX, Huang XE, Qian ZY, Xu X, Li Y, Li CG. Clinical observation of Endostar® combined with chemotherapy in advanced colorectal cancer patients. Asian Pac J Cancer Prev. 2011;12(11):3087–90.
Pan Y, Jiao G. Short-term therapeutic effect of Endostar combined with chemotherapy for advanced colorectal cancer: a meta-analysis. Nan Fang Yi Ke Da Xue Xue Bao. 2014;34(2):270–4.
Huang W, Liu J, Wu F, et al. The efficacy and safety of endostar combined with taxane-based regimens for HER-2-negative metastatic breast cancer patients. Oncotarget. 2016;7(21):31501–7.
Harbeck N, Penault-Llorca F, Cortes J, et al. Breast cancer. Nat Rev Dis Primers. 2019;5(1):66–66.
Tolleson WH. Human melanocyte biology, toxicology, and pathology. J Environ Sci Health C. 2005;23(2):105–61.
Lee B, Mukhi N, Liu D. Current management and novel agents for malignant melanoma. J Hematol Oncol. 2012;5:3.
Falkson CI, Ibrahim J, Kirkwood JM, Coates AS, Atkins MB, Blum RH. Phase III trial of dacarbazine versus dacarbazine with interferon alpha-2b versus dacarbazine with tamoxifen versus dacarbazine with interferon alpha-2b and tamoxifen in patients with metastatic malignant melanoma: an Eastern Cooperative Oncology Group study. J Clin Oncol. 1998;16(5):1743–51.
Middleton MR, Grob JJ, Aaronson N, et al. Randomized phase III study of temozolomide versus dacarbazine in the treatment of patients with advanced metastatic malignant melanoma [published correction appears in J Clin Oncol 2000 Jun; 18(11):2351]. J Clin Oncol. 2000;18(1):158–66.
Avril MF, Aamdal S, Grob JJ, et al. Fotemustine compared with dacarbazine in patients with disseminated malignant melanoma: a phase III study. J Clin Oncol. 2004;22(6):1118–25.
Cui C, Mao L, Chi Z, et al. A phase II, randomized, double-blind, placebo-controlled multicenter trial of Endostar in patients with metastatic melanoma. Mol Ther. 2013;21(7):1456–63.
Misaghi A, Goldin A, Awad M, Kulidjian AA. Osteosarcoma: a comprehensive review. SICOT J. 2018;4:12–12.
American Cancer Society. Osteosarcoma. American Cancer Society; 2023. https://www.cancer.org/cancer/osteosarcoma.html. Accessed 3 March 2023.
Xu M, Xu CX, Bi WZ, et al. Effects of endostar combined multidrug chemotherapy in osteosarcoma. Bone. 2013;57(1):111–5.
Chen Z, Guo W, Cao J, et al. Endostar in combination with modified FOLFOX6 as an initial therapy in advanced colorectal cancer patients: a phase I clinical trial. Cancer Chemother Pharmacol. 2015;75(3):547–57.
Hanna NN, Seetharam S, Mauceri HJ, et al. Antitumor interaction of short-course endostatin and ionizing radiation. Cancer J. 2000;6(5):287–93.
Dkhissi F, Lu H, Soria C, et al. Endostatin exhibits a direct antitumor effect in addition to its antiangiogenic activity in colon cancer cells. Hum Gene Ther. 2003;14(10):997–1008.
Bruns CJ, Harbison MT, Davis DW, et al. Epidermal growth factor receptor blockade with C225 plus gemcitabine results in regression of human pancreatic carcinoma growing orthotopically in nude mice by antiangiogenic mechanisms. Clin Cancer Res. 2000;6(5):1936–48.
Raut CP, Takamori RK, Davis DW, Sweeney-Gotsch B, O’Reilly MS, McConkey DJ. Direct effects of recombinant human endostatin on tumor cell IL-8 production are associated with increased endothelial cell apoptosis in an orthotopic model of human pancreatic cancer [published correction appears in Cancer Biol Ther. 2009 May;8(10):984]. Cancer Biol Ther. 2004;3(7):679–87.
Arslan AE, Simsek E, Fidan KA, Fiskin K. Endostatin enhances radioresponse in breast cancer cells via alteration of substance P levels. Oncol Lett. 2011;2(5):879–86.
Aydemir EA, Şimşek E, Korcum AF, Fişkin K. Endostatin and irradiation modifies the activity of ADAM10 and neprilysin in breast cancer cells. Mol Med Rep. 2016;14(3):2343–51.
Wang B, Wang X, Wayne C, et al. Production of a therapeutic protein by fusing it with two fragments of the carboxyl-terminal peptide of human chorionic gonadotropin β-subunit in Pichia pastoris. Biotechnol Lett. 2016;38(5):801–7.
Limaverde-Sousa G, Sternberg C, Ferreira CG. Antiangiogenesis beyond VEGF inhibition: a journey from antiangiogenic single-target to broad-spectrum agents. Cancer Treat Rev. 2014;40(4):548–57.
Tang L, Persky AM, Hochhaus G, Meibohm B. Pharmacokinetic aspects of biotechnology products. J Pharm Sci. 2004;93(9):2184–204.
Kontermann RE. Half-life extended biotherapeutics [published correction appears in Expert Opin Biol Ther. 2016 Sep;16(9):1179]. Expert Opin Biol Ther. 2016;16(7):903–15.
Iyengar ARS, Gupta S, Jawalekar S, Pande AH. Protein chimerization: a new frontier for engineering protein therapeutics with improved pharmacokinetics. J Pharmacol Exp Ther. 2019;370(3):703–14.
Zaman R, Islam RA, Ibnat N, et al. Current strategies in extending half-lives of therapeutic proteins. J Control Release. 2019;301:176–89.
Tryggvason K, Wartiovaara J. How does the kidney filter plasma? Physiology (Bethesda). 2005;20:96–101.
Strohl WR. Fusion proteins for half-life extension of biologics as a strategy to make biobetters. BioDrugs. 2015;29(4):215–39.
Ryman JT, Meibohm B. Pharmacokinetics of monoclonal antibodies. CPT Pharmacometr Syst Pharmacol. 2017;6(9):576–88.
Meibohm B. Pharmacokinetics and half‐life of protein therapeutics. In: Therapeutic proteins: strategies to modulate their plasma half‐lives. New York: Wiley; 2012, pp. 23–38.
Roopenian DC, Akilesh S. FcRn: the neonatal Fc receptor comes of age. Nat Rev Immunol. 2007;7(9):715–25.
Schmidt SR. Fusion-proteins as biopharmaceuticals—applications and challenges. Curr Opin Drug Discov Dev. 2009;12(2):284–95.
Sockolosky JT, Szoka FC. The neonatal Fc receptor, FcRn, as a target for drug delivery and therapy. Adv Drug Deliv Rev. 2015;91:109–24.
Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84(5):548–58.
Fee CJ, Van Alstine JM. Purification of pegylated proteins. Methods Biochem Anal. 2011;54:339–62.
Li L, Wang Y, Chen J, et al. An engineered arginase FC protein inhibits tumor growth in vitro and in vivo. Evid Based Complement Altern Med. 2013;2013:423129.
Haeckel A, Appler F, Ariza de Schellenberger A, Schellenberger E. XTEN as biological alternative to pegylation allows complete expression of a protease-activatable killin-based cytostatic. PLoS ONE. 2016;11(6):e0157193.
Anakha J, Kawathe PS, Datta S, Jawalekar SS, Banerjee UC, Pande AH. Human arginase 1, a Jack of all trades? 3 Biotech. 2022;12(10):264–264.
Schlapschy M, Theobald I, Mack H, Schottelius M, Wester HJ, Skerra A. Fusion of a recombinant antibody fragment with a homo-amino-acid polymer: effects on biophysical properties and prolonged plasma half-life. Protein Eng Des Sel. 2007;20(6):273–84.
Aghaabdollahian S, Ahangari Cohan R, Norouzian D, et al. Enhancing bioactivity, physicochemical, and pharmacokinetic properties of a nano-sized, anti-VEGFR2 Adnectin, through PASylation technology. Sci Rep. 2019;9(1):2978.
Sockolosky JT, Tiffany MR, Szoka FC. Engineering neonatal Fc receptor-mediated recycling and transcytosis in recombinant proteins by short terminal peptide extensions. Proc Natl Acad Sci USA. 2012;109(40):16095–100.
Kontermann RE. Strategies for extended serum half-life of protein therapeutics. Curr Opin Biotechnol. 2011;22(6):868–76.
Dobariya P, Adhya P, Vaidya B, Khandave PY, Sharma SS, Pande AH. Fused human paraoxonase 1 as a prophylactic agent against organophosphate poisoning. Enzyme Microb Technol. 2023;165: 110209.
US FDA. Food and Drug Administration; 2023. https://www.fda.gov. Accessed 3 March 2023.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
JA and PKD involved in conceptualization, data curation, and original draft preparation. SSS and AHP involved in reviewing and editing of manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anakha, J., Dobariya, P., Sharma, S.S. et al. Recombinant human endostatin as a potential anti-angiogenic agent: therapeutic perspective and current status. Med Oncol 41, 24 (2024). https://doi.org/10.1007/s12032-023-02245-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-023-02245-w