Abstract
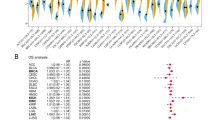
ATF3 is an essential transcription activator in regulating cancer-related genetic expression. To identify the role of ATF3 in ovarian tumor, we investigated the correlation between ATF3 expression and the clinicopathological properties using multiple database. The cBioPortal and GEPIA database displayed the clinical information of ovarian patients harboring or without harboring ATF3 mutation. Furthermore, we assessed the relationship between survival and ATF3 expression level using Kaplan–Meier plotter, which reveals that the ovarian patients with higher expression of ATF3 suffered the worse overall survival and progression-free survival. The differentially expressed genes were analyzed using gene ontology, protein–protein interaction network, and gene set enrichment analysis to identify the hub gene and critical pathways, significantly affecting the tumorigenesis of ovarian tumor. Finally, we assessed the correlation between ATF3 and immune cell infiltration using Tumor Immunoassay Resource (TIMER) database. The results demonstrated that higher expression has a positive correlation with macrophage infiltration, expression for M1- and M2-type macrophages. Our study suggests that ATF3 can regulate the cell cycle and heme-related oxidative phosphorylation process, and it may be a critical factor to regulate the macrophage cell to be infiltrated into ovarian cancer. ATF3 can be used as a biomarker for diagnosis and therapy of ovarian tumor.










Similar content being viewed by others
References
Jayson GC, Kohn EC, Kitchener HC, Ledermann JA. Ovarian cancer. The Lancet. 2014;384(9951):1376–88.
Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD, Gaudet MM, Jemal A, Siegel RL. Ovarian cancer statistics, 2018. CA Cancer J Clin. 2018;68(4):284–96.
Coffman LG, Burgos-Ojeda D, Wu R, Cho K, Bai S, Buckanovich RJ. New models of hematogenous ovarian cancer metastasis demonstrate preferential spread to the ovary and a requirement for the ovary for abdominal dissemination. Transl Res. 2016;175:92-102. e2.
Patch A-M, Christie EL, Etemadmoghadam D, Garsed DW, George J, Fereday S, Nones K, Cowin P, Alsop K, Bailey PJ. Whole–genome characterization of chemoresistant ovarian cancer. Nature. 2015;521(7553):489–94.
Network CGAR. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474(7353):609.
Madariaga A, Lheureux S, Oza AM. Tailoring ovarian cancer treatment: implications of BRCA1/2 mutations. Cancers. 2019;11(3):416.
Naora H, Montell DJ. Ovarian cancer metastasis: integrating insights from disparate model organisms. Nat Rev Cancer. 2005;5(5):355–66.
Yin M, Li X, Tan S, Zhou HJ, Ji W, Bellone S, Xu X, Zhang H, Santin AD, Lou G. Tumor-associated macrophages drive spheroid formation during early transcoelomic metastasis of ovarian cancer. J Clin Investig. 2016;126(11):4157–73.
Browning L, Patel MR, Horvath EB, Tawara K, Jorcyk CL. IL-6 and ovarian cancer: inflammatory cytokines in promotion of metastasis. Cancer Manag Res. 2018;10:6685.
Zhang R, Shi H, Ren F, Feng W, Cao Y, Li G, Liu Z, Ji P, Zhang M. MicroRNA-338-3p suppresses ovarian cancer cells growth and metastasis: implication of Wnt/catenin beta and MEK/ERK signaling pathways. J Exp Clin Cancer Res. 2019;38(1):1–13.
Duncan RM, Reyes L, Moats K, Robinson RM, Murphy SA, Kaur B, Stessman HA, Dolloff NG. ATF3 coordinates antitumor synergy between epigenetic drugs and protein disulfide isomerase inhibitors. Can Res. 2020;80(16):3279–91.
Chang YS, Jalgaonkar SP, Middleton JD, Hai T. Stress-inducible gene Atf3 in the noncancer host cells contributes to chemotherapy-exacerbated breast cancer metastasis. Proc Natl Acad Sci. 2017;114(34):E7159-68.
Yan C, Boyd DD. ATF3 regulates the stability of p53: a link to cancer. Cell Cycle (Georgetown, Tex). 2006;5(9):926–9.
Lim R, Barker G, Liong S, Nguyen-Ngo C, Tong S, Kaitu’u-Lino Tu, Lappas M. ATF3 is a negative regulator of inflammation in human fetal membranes. Placenta. 2016;47:63–72.
Zhang Z-B, Ruan C-C, Chen D-R, Zhang K, Yan C, Gao P-J. Activating transcription factor 3 SUMOylation is involved in angiotensin II-induced endothelial cell inflammation and dysfunction. J Mol Cell Cardiol. 2016;92:149–57.
Chan CM, Macdonald CD, Litherland GJ, Wilkinson DJ, Skelton A, Europe-Finner GN, Rowan AD. Cytokine-induced MMP13 expression in human chondrocytes is dependent on activating transcription factor 3 (ATF3) regulation. J Biol Chem. 2017;292(5):1625–36.
Lee S, Kim G-L, Kim NY, Kim S-J, Ghosh P, Rhee D-K. ATF3 stimulates IL-17A by regulating intracellular Ca2+/ROS-dependent IL-1β activation during Streptococcus pneumoniae infection. Front Immunol. 1954;2018:9.
Sood V, Sharma KB, Gupta V, Saha D, Dhapola P, Sharma M, Sen U, Kitajima S, Chowdhury S, Kalia M. ATF3 negatively regulates cellular antiviral signaling and autophagy in the absence of type I interferons. Sci Rep. 2017;7(1):1–17.
Zhang Y, Xu J, Zhang N, Chen M, Wang H, Zhu D. Targeting the tumour immune microenvironment for cancer therapy in human gastrointestinal malignancies. Cancer Lett. 2019;458:123–35.
Almeida FV, Douglass SM, Fane ME, Weeraratna AT. Bad company: microenvironmentally mediated resistance to targeted therapy in melanoma. Pigment Cell Melanoma Res. 2019;32(2):237–47.
Li J, Byrne KT, Yan F, Yamazoe T, Chen Z, Baslan T, Richman LP, Lin JH, Sun YH, Rech AJ. Tumor cell-intrinsic factors underlie heterogeneity of immune cell infiltration and response to immunotherapy. Immunity. 2018;49(1):178-193. e7.
Hao M, Wu T, Chen Q, Lian X, Wu H. Hyperbranched polyglycerols as robust up-conversion nanoparticle coating layer for feasible cell imaging. Polymers. 2020;12(11):2592.
Hu K, Li K, Lv J, Feng J, Chen J, Wu H, Cheng F, Jiang W, Wang J, Pei H, Chiao PJ, Cai Z, Chen Y, Liu M, Pang X. Suppression of the SLC7A11/glutathione axis causes synthetic lethality in KRAS-mutant lung adenocarcinoma. J Clin Invest. 2020;130(4):1752–66.
Burrell RA, McGranahan N, Bartek J, Swanton C. The causes and consequences of genetic heterogeneity in cancer evolution. Nature. 2013;501(7467):338–45.
Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM, Linette GP, Hogg D, Ottensmeier CH, Lebbé C, Peschel C, Quirt I, Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos A, Urba WJ. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–23.
Brüggmann D, Pulch K, Klingelhöfer D, Pearce CL, Groneberg DA. Ovarian cancer: density equalizing mapping of the global research architecture. Int J Health Geogr. 2017;16(1):3.
Lee KA, Hai TY, SivaRaman L, Thimmappaya B, Hurst HC, Jones NC, Green MR. A cellular protein, activating transcription factor, activates transcription of multiple E1A-inducible adenovirus early promoters. Proc Natl Acad Sci USA. 1987;84(23):8355–9.
Yilmaz M, Christofori G. EMT, the cytoskeleton, and cancer cell invasion. Cancer Metastasis Rev. 2009;28(1–2):15–33.
Fife CM, McCarroll JA, Kavallaris M. Movers and shakers: cell cytoskeleton in cancer metastasis. Br J Pharmacol. 2014;171(24):5507–23.
Wu H, Chen Q, Jiao M, Xia X, Lian X, Huang N, Li K, Yin J, Shi B. Evaluation of nanomechanical properties of hyperbranched polyglycerols as prospective cell membrane engineering block. Colloids Surf B Biointerf. 2020;190:110968.
Fiorito V, Chiabrando D, Petrillo S, Bertino F, Tolosano E. The multifaceted role of heme in cancer. Front Oncol. 2019;9:1540.
Strainic MG, Pohlmann E, Valley CC, Sammeta A, Hussain W, Lidke DS, Medof ME. RTK signaling requires C3ar1/C5ar1 and IL-6R joint signaling to repress dominant PTEN, SOCS1/3 and PHLPP restraint. FASEB J. 2020;34(2):2105–25.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Kaur A, Ecker BL, Douglass SM, Kugel CH, Webster MR, Almeida FV, Somasundaram R, Hayden J, Ban E, Ahmadzadeh H, Franco-Barraza J, Shah N, Mellis IA, Keeney F, Kossenkov A, Tang HY, Yin X, Liu Q, Xu X, Fane M, Brafford P, Herlyn M, Speicher DW, Wargo JA, Tetzlaff MT, Haydu LE, Raj A, Shenoy V, Cukierman E, Weeraratna AT. Remodeling of the collagen matrix in aging skin promotes melanoma metastasis and affects immune cell motility. Cancer Discov. 2019;9(1):64–81.
Vilgelm AE, Richmond A. Chemokines modulate immune surveillance in tumorigenesis, metastasis, and response to immunotherapy. Front Immunol. 2019;10:333.
Cheng H, Wang Z, Fu L, Xu T. Macrophage polarization in the development and progression of ovarian cancers: an overview. Front Oncol. 2019;9:421.
Kobayashi M, Nakashima A, Yoshino O, Yoshie M, Ushijima A, Ito M, Ono Y, Shima T, Kawamura K, Ishizuka B, Saito S. Decreased effector regulatory T cells and increased activated CD4(+) T cells in premature ovarian insufficiency. Am J Reprod Immunol. 2019;81(6):e13125.
Lan J, Sun L, Xu F, Liu L, Hu F, Song D, Hou Z, Wu W, Luo X, Wang J, Yuan X, Hu J, Wang G. M2 macrophage-derived exosomes promote cell migration and invasion in colon cancer. Can Res. 2019;79(1):146–58.
Zhao Q, Zhong J, Lu P, Feng X, Han Y, Ling C, Guo W, Zhou W. DOCK4 is a platinum-chemosensitive and prognostic-related biomarker in ovarian cancer. PPAR Res. 2021;2021:6629842.
Acknowledgements
This work is supported by Henan Province Medical Science and Technique Foundation (NO. LHGJ20200035).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All the authors declared no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, X., Liu, P., Sun, X. et al. Analyzing the impact of ATF3 in tumorigenesis and immune cell infiltration of ovarian tumor: a bioinformatics study. Med Oncol 38, 91 (2021). https://doi.org/10.1007/s12032-021-01541-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-021-01541-7



