Abstract
Background
After esophagectomy for esophageal carcinoma, 2–13% of patients develop brain metastases (BM) which are associated with a poor prognosis. Further investigation into treatment and prognosis is beneficial given the limited available literature and varying outcomes.
Methods
Case files of all 339 patients who underwent minimally invasive esophagectomy (MIE) in a single high-volume center between January 2015 and December 2020 were retrospectively reviewed. Patients with BM and isolated brain metastases (iBM) were identified and a survival analysis was performed.
Results
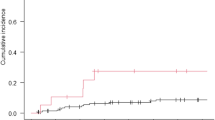
Fifteen out of 339 patients (4,4%) undergoing MIE developed BM of which 9 (60,0%) had iBM. Most patients were diagnosed with squamous cell carcinoma (55,6%), localized in the middle third of the esophagus (66,7%), and had a pathologic complete response (66,7%) after initial treatment. Treatment of iBM consisted of gamma knife (GK) radiosurgery (44,4%), surgical resection (22,2%), GK and surgical resection (11,1%), and best supportive care (22,2%). Median time to diagnose iBM was 8,4 months (range 0,2–37,5) and survival after detection of iBM was 14,3 months (95% CI 0,0–45.9). The 2-year survival rate after detection of iBM was 44,4%.
Conclusions
iBM after esophagectomy for esophageal carcinoma is rare, but when encountered can and should be treated with a curative intent in selected cases in close collaboration with large neurosurgical centers. A large-scale study should be conducted to confirm our findings.

Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. https://doi.org/10.3322/caac.21492.
van Putten M, de Vos-Geelen J, Nieuwenhuijzen GAP, Siersema PD, Lemmens V, Rosman C, van der Sangen MJC, Verhoeven RHA. Long-term survival improvement in oesophageal cancer in the Netherlands. Eur J Cancer. 2018;94:138–47. https://doi.org/10.1016/j.ejca.2018.02.025.
Borggreve AS, Kingma BF, Domrachev SA, Koshkin MA, Ruurda JP, van Hillegersberg R, Takeda FR, Goense L. Surgical treatment of esophageal cancer in the era of multimodality management. Ann N Y Acad Sci. 2018;1434:192–209. https://doi.org/10.1111/nyas.13677.
Oppedijk V, van der Gaast A, van Lanschot JJ, van Hagen P, van Os R, van Rij CM, van der Sangen MJ, et al. Patterns of recurrence after surgery alone versus preoperative chemoradiotherapy and surgery in the cross trials. J Clin Oncol. 2014;32:385–91. https://doi.org/10.1200/jco.2013.51.2186.
Meguid RA, Hooker CM, Taylor JT, Kleinberg LR, Cattaneo SM 2nd, Sussman MS, Yang SC, et al. Recurrence after neoadjuvant chemoradiation and surgery for esophageal cancer: does the pattern of recurrence differ for patients with complete response and those with partial or no response? J Thorac Cardiovasc Surg. 2009;138:1309–17. https://doi.org/10.1016/j.jtcvs.2009.07.069.
Smith RS, Miller RC. Incidence of brain metastasis in patients with esophageal carcinoma. World J Gastroenterol. 2011;17:2407–10. https://doi.org/10.3748/wjg.v17.i19.2407.
Song Z, Lin B, Shao L, Zhang Y. Brain metastases from esophageal cancer: clinical review of 26 cases. World Neurosurg. 2014;81:131–5. https://doi.org/10.1016/j.wneu.2013.02.058.
Harada K, Hwang H, Wang X, Abdelhakeem A, Iwatsuki M, Murphy MAB, Maru DM, et al. Brain metastases in patients with upper gastrointestinal cancer is associated with proximally located adenocarcinoma and lymph node metastases. Gastric Cancer. 2020;23:904–12. https://doi.org/10.1007/s10120-020-01075-3.
Ogawa K, Toita T, Sueyama H, Fuwa N, Kakinohana Y, Kamata M, Adachi G, et al. Brain metastases from esophageal carcinoma: natural history, prognostic factors, and outcome. Cancer. 2002;94:759–64. https://doi.org/10.1002/cncr.10271.
Müller-Stich BP, Probst P, Nienhüser H, Fazeli S, Senft J, Kalkum E, Heger P, et al. Meta-analysis of randomized controlled trials and individual patient data comparing minimally invasive with open oesophagectomy for cancer. Br J Surg. 2021;108:1026–33. https://doi.org/10.1093/bjs/znab278.
Schizas D, Lazaridis II, Moris D, Mastoraki A, Lazaridis LD, Tsilimigras DI, Charalampakis N, Liakakos T. The role of surgical treatment in isolated organ recurrence of esophageal cancer-a systematic review of the literature. World J Surg Oncol. 2018;16:55. https://doi.org/10.1186/s12957-018-1357-y.
Ohkura Y, Shindoh J, Ueno M, Iizuka T, Udagawa H. Clinicopathologic characteristics of oligometastases from esophageal cancer and long-term outcomes of resection. Ann Surg Oncol. 2020;27:651–9. https://doi.org/10.1245/s10434-019-08175-0.
Zhang P, Yao L, Chen M, Feng W. Prognostic factors affecting long-term outcomes in patients with brain metastasis from esophageal carcinoma. Chin J Cancer Res. 2020;32:768–77. https://doi.org/10.21147/j.issn.1000-9604.2020.06.10.
Nobel TB, Dave N, Eljalby M, Xing X, Barbetta A, Hsu M, Tan KS, et al. Incidence and risk factors for isolated esophageal cancer recurrence to the brain. Ann Thorac Surg. 2020;109:329–36. https://doi.org/10.1016/j.athoracsur.2019.09.028.
Rice TW, Khuntia D, Rybicki LA, Adelstein DJ, Vogelbaum MA, Mason DP, Murthy SC, Blackstone EH. Brain metastases from esophageal cancer: a phenomenon of adjuvant therapy? Ann Thorac Surg. 2006;82(2042–9):49.e1-2. https://doi.org/10.1016/j.athoracsur.2006.06.089.
Tachimori Y. Pattern of lymph node metastases of squamous cell esophageal cancer based on the anatomical lymphatic drainage system: efficacy of lymph node dissection according to tumor location. J Thorac. 2017;9:S724-s30. https://doi.org/10.21037/jtd.2017.06.19.
Blum Murphy M, Xiao L, Patel VR, Maru DM, Correa AM, Amlashi FG, Liao Z, et al. Pathological complete response in patients with esophageal cancer after the trimodality approach: the association with baseline variables and survival-the University of Texas Md Anderson Cancer Center experience. Cancer. 2017;123:4106–13. https://doi.org/10.1002/cncr.30953.
Al-Kaabi A, van der Post RS, van der Werf LR, Wijnhoven BPL, Rosman C, Hulshof MCCM, van Laarhoven HWM, et al. Impact of pathological tumor response after CROSS neoadjuvant chemoradiotherapy followed by surgery on long-term outcome of esophageal cancer: a population-based study. Acta Oncol. 2021;60:497–504. https://doi.org/10.1080/0284186X.2020.1870246.
Wadhwa R, Taketa T, Correa AM, Sudo K, Campagna MC, Blum MA, Komaki R, et al. Incidence of brain metastases after trimodality therapy in patients with esophageal or gastroesophageal cancer: implications for screening and surveillance. Oncology. 2013;85:204–7. https://doi.org/10.1159/000354736.
Author information
Authors and Affiliations
Contributions
SS, TK, ISM, JH, and RM contributed to the study design and its concept. TK coordinated the procedures necessary for approval by the institutional review board. SS was responsible for the data collection under the supervision of ISM, JH, and RM. SS performed the analysis and wrote the manuscript. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study protocol was approved by the Institutional Ethical Review Board (L1049.2020) and the requirement for informed consent was waived due to the retrospective and anonymized nature of the data.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stuart, S.K., Kuypers, T.J.L., Martijnse, I.S. et al. Patients with Isolated Brain Metastases from Esophageal Carcinoma After Minimally Invasive Esophagectomy May Not Have a Dismal Prognosis. J Gastrointest Canc 54, 751–755 (2023). https://doi.org/10.1007/s12029-022-00870-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-022-00870-8