Abstract
Background
In this study, we aimed to investigate the risk factors and impact of poststroke pneumonia (PSP) on mortality and functional outcome in patients with acute ischemic stroke (AIS) after endovascular thrombectomy (EVT).
Methods
This was a post hoc analysis of a prospective randomized trial (Direct intraarterial thrombectomy in order to revascularize AIS patients with large-vessel occlusion efficiently in Chinese tertiary hospitals: a multicenter randomized clinical trial). Patients with AIS who completed EVT were evaluated for the occurrence of PSP during the hospitalization period and their modified Rankin Scale (mRS) scores at 90 days after AIS. Logistic regression analysis was conducted to investigate the independent predictors of PSP. Propensity score matching was conducted for the PSP and non-PSP groups by using the covariates resulting from the logistic regression analysis. The associations between PSP and outcomes were analyzed. The outcomes included 90-day poor functional outcome (mRS scores > 2), 90-day mortality, and early 2-week mortality.
Results
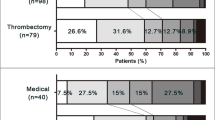
A total of 639 patients were enrolled, of whom 29.58% (189) developed PSP. Logistic regression analysis revealed that history of chronic heart failure (unadjusted odds ratio [OR] 2.011, 95% confidence interval [CI] 1.026–3.941; P = 0.042), prethrombectomy reperfusion on initial digital subtraction angiography (OR 0.394, 95% CI 0.161–0.964; P = 0.041), creatinine levels at admission (OR 1.008, 95% CI 1.000–1.016; P = 0.049), and National Institutes of Health Stroke Scale at 24 h (OR 1.023, 95% CI 1.007–1.039; P = 0.004) were independent risk factors for PSP. With propensity scoring matching, poor functional outcome (mRS > 2) was more common in patients with PSP than in patients without PSP (81.03% vs. 71.83%, P = 0.043) at 90 days after EVT. The early 2-week mortality of patients with PSP was lower (5.74% vs. 12.07%, P = 0.038). But there was no statistically significant difference in 90-day mortality between the PSP group and non-PSP group (22.41% vs. 14.94%, P = 0.074). The survivorship curve also shows no statistical significance (P = 0.088) between the two groups.
Conclusions
Nearly one third of patients with AIS and EVT developed PSP. Heart failure, higher creatinine levels, prethrombectomy reperfusion, and National Institutes of Health Stroke Scale at 24 h were associated with PSP in these patients. PSP was associated with poor 90-day functional outcomes in patients with AIS treated with EVT.



Similar content being viewed by others
References
Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–31.
Badve MS, Zhou Z, van de Beek D, et al. Frequency of post-stroke pneumonia: systematic review and meta-analysis of observational studies. Int J Stroke. 2019;14:125–36.
Cugy E, Sibon I. Stroke-associated pneumonia risk score: validity in a French stroke unit. J Stroke Cerebrovasc Dis. 2017;26:225–9.
Wei M, Huang Q, Yu F, et al. Stroke-associated infection in patients with co-morbid diabetes mellitus is associated with in-hospital mortality. Front Aging Neurosci. 2022;14:1024496.
Yang P, Zhang Y, Zhang L, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med. 2020;382(21):1981–93.
Shi Y, Huang Y, Zhang TT, Cao B, Wang H, Zhuo C, Ye F, Su X, Fan H, Xu JF, Zhang J, Lai GX, She DY, Zhang XY, He B, He LX, Liu YN, Qu JM. Chinese guidelines for the diagnosis and treatment of hospital-acquired pneumonia and ventilator-associated pneumonia in adults (2018 Edition). J Thorac Dis. 2019;11(6):2581–616.
Schaller-Paule MA, Foerch C, Bohmann FO, et al. Predicting poststroke pneumonia in patients with anterior large vessel occlusion: a prospective. Popul Based Stroke Registry Anal Front Neurol. 2022;13: 824450.
De Jonge JC, Takx RAP, Kauw F, et al. Signs of pulmonary infection on admission chest computed tomography are associated with pneumonia or death in patients with acute stroke. Stroke. 2020;51(6):1690–5.
Kishore AK, Jeans AR, Garau J, et al. Antibiotic treatment for pneumonia complicating stroke: recommendations from the pneumonia in stroke consensus (PISCES) group. Eur Stroke J. 2019;4(4):318–28.
Zhang P, Chen L, Jiang Y, Yuan H, Zhu X, Zhang M, Wu T, Deng B, Yang P, Zhang Y, Liu J. Risk factors for and outcomes of poststroke pneumonia in patients with acute ischemic stroke treated with mechanical thrombectomy. Front Neurol. 2023;14:1023475.
Siedler G, Sommer K, Macha K, et al. Heart failure in ischemic stroke: relevance for acute care and outcome. Stroke. 2019;50(11):3051–6.
Tsivgoulis G, Katsanos AH, Schellinger PD, et al. Successful reperfusion with intravenous thrombolysis preceding mechanical thrombectomy in large-vessel occlusions. Stroke. 2018;49(1):232–5.
Shen L, Jhund PS, Anand IS, et al. Incidence and outcomes of pneumonia in patients with heart failure. J Am Coll Cardiol. 2021;77(16):1961–73.
Li SJ, Hu HQ, Wang XL, Cao BZ. Correlation between post-stroke pneumonia and outcome in patients with acute brain infarction. Zhonghua Yi Xue Za Zhi. 2016;96(35):2796–801.
Ueki K, Matsuo R, Kuwashiro T, et al. Decreased estimated glomerular filtration rate and proteinuria and long-term outcomes after ischemic stroke: A longitudinal observational cohort study. Stroke. 2023;54(5):1268–77.
Su G, Trevisan M, Ishigami J, et al. Short- and long-term outcomes after incident pneumonia in adults with chronic kidney disease: a time-dependent analysis from the Stockholm Creatinine Measurement project. Nephrol Dial Transplant. 2020;35(11):1894–900.
Ishigami J, Grams ME, Chang AR, et al. CKD and risk for hospitalization with infection: the atherosclerosis risk in communities (ARIC) study. Am J Kidney Dis. 2017;69:752–61.
Teh WH, Smith CJ, Barlas RS, et al. Impact of stroke-associated pneumonia on mortality, length of hospitalization, and functional outcome. Acta Neurol Scand. 2018;138(4):293–300.
Rocco A, Fam G, Sykora M, Diedler J, Nagel S, Ringleb P. Poststroke infections are an independent risk factor for poor functional outcome after three-months in thrombolysed stroke patients. Int J Stroke. 2013;8(8):639–44.
Ingeman A, Andersen G, Hundborg HH, Svendsen ML, Johnsen SP. In-hospital medical complications, length of stay, and mortality among stroke unit patients. Stroke. 2011;42(11):3214–8.
Koennecke HC, Belz W, Berfelde D, Endres M, Fitzek S, Hamilton F, Kreitsch P, Mackert BM, Nabavi DG, Nolte CH, Pöhls W, Schmehl I, Schmitz B, von Brevern M, Walter G, Heuschmann PU; Berlin Stroke Register Investigators. Factors influencing in-hospital mortality and morbidity in patients treated on a stroke unit. Neurology. 2011;77(10):965–72.
Chen Y, Zhou S, Yang S, Mofatteh M, Hu Y, Wei H, Lai Y, Zeng Z, Yang Y, Yu J, Chen J, Sun X, Wei W, Nguyen TN, Baizabal-Carvallo JF, Liao X. Developing and predicting of early mortality after endovascular thrombectomy in patients with acute ischemic stroke. Front Neurosci. 2022;16:1034472.
Li H, Huang J, Ye S, Chen H, Yuan L, Liao G, Du W, Li C, Fang L, Liu S, Yang P, Zhang Y, Xing P, Zhang X, Ye X, Peng Y, Cao J, Zhang L, Yang Z, Liu J; DIRECT-MT investigators. Predictors of mortality in acute ischemic stroke treated with endovascular thrombectomy despite successful reperfusion: subgroup analysis of a multicentre randomised clinical trial. BMJ Open. 2022;12(3):e053765.
Nutakki A, Chomba M, Chishimba L, et al. Predictors of in-hospital and 90-day post-discharge stroke mortality in Lusaka. Zambia J Neurol Sci. 2022;437: 120249.
Patel UK, Kodumuri N, Dave M, et al. Stroke-associated pneumonia: a retrospective study of risk factors and outcomes. Neurologist. 2020;25(3):39–48.
Zhu Y, Gao J, Lv Q, et al. Risk factors and outcomes of stroke-associated pneumonia in patients with stroke and acute large artery occlusion treated with endovascular thrombectomy. J Stroke Cerebrovasc Dis. 2020;29(11): 105223.
Funding
This work was funded by a grant (GN-2017R0001) from the Stroke Prevention Project of the National Health Commission of the People’s Republic of China and by the Wu Jieping Medical Foundation.
Author information
Authors and Affiliations
Contributions
PZ conducted research design and writing. Lei Chen was responsible for the data collection. XFY was responsible for statistical analysis. Writing direction was given by TW and BQD. YH revised the article. PFY and YWZ conducted the Direct intraarterial thrombectomy in order to revascularize AIS patients with large-vessel occlusion efficiently in Chinese tertiary hospitals: a multicenter randomized clinical trial. JML was the organizer of the Direct intraarterial thrombectomy in order to revascularize AIS patients with large-vessel occlusion efficiently in Chinese tertiary hospitals: a multicenter randomized clinical trial. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Ethical Approval/Informed Consent
The study was approved by the institutional review board and local ethical committee of the 41 academic tertiary care centers concerned. The main ethical approval number is CHEC2018-003 by Shanghai Changhai Hospital Ethics Committee.
Conflict of interest
The authors of this article declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, P., Chen, L., Ye, Xf. et al. Outcome and Risk of Poststroke Pneumonia in Patients with Acute Ischemic Stroke After Endovascular Thrombectomy: A Post Hoc Analysis of the DIRECT-MT Trial. Neurocrit Care (2024). https://doi.org/10.1007/s12028-024-01947-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-024-01947-x