Abstract
Background
Brain tissue hypoxia is an independent risk factor for unfavorable outcomes in traumatic brain injury (TBI); however, systemic hyperoxemia encountered in the prevention and/or response to brain tissue hypoxia may also impact risk of mortality. We aimed to identify temporal patterns of partial pressure of oxygen in brain tissue (PbtO2), partial pressure of arterial oxygen (PaO2), and PbtO2/PaO2 ratio associated with mortality in children with severe TBI.
Methods
Data were extracted from the electronic medical record of a quaternary care children’s hospital with a level I trauma center for patients ≤ 18 years old with severe TBI and the presence of PbtO2 and/or intracranial pressure monitors. Temporal analyses were performed for the first 5 days of hospitalization by using locally estimated scatterplot smoothing for less than 1,000 observations and generalized additive models with integrated smoothness estimation for more than 1,000 observations.
Results
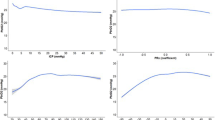
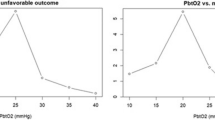
A total of 138 intracranial pressure–monitored patients with TBI (median 5.0 [1.9–12.8] years; 65% boys; admission Glasgow Coma Scale score 4 [3–7]; mortality 18%), 71 with PbtO2 monitors and 67 without PbtO2 monitors were included. Distinct patterns in PbtO2, PaO2, and PbtO2/PaO2 were evident between survivors and nonsurvivors over the first 5 days of hospitalization. Time-series analyses showed lower PbtO2 values on day 1 and days 3–5 and lower PbtO2/PaO2 ratios on days 1, 2, and 5 among patients who died. Analysis of receiver operating characteristics curves using Youden’s index identified a PbtO2 of 30 mm Hg and a PbtO2/PaO2 ratio of 0.12 as the cut points for discriminating between survivors and nonsurvivors. Univariate logistic regression identified PbtO2 < 30 mm Hg, hyperoxemia (PaO2 ≥ 300 mm Hg), and PbtO2/PaO2 ratio < 0.12 to be independently associated with mortality.
Conclusions
Lower PbtO2, higher PaO2, and lower PbtO2/PaO2 ratio, consistent with impaired oxygen diffusion into brain tissue, were associated with mortality in this cohort of children with severe TBI. These results corroborate our prior work that suggests targeting a higher PbtO2 threshold than recommended in current guidelines and highlight the potential use of the PbtO2/PaO2 ratio in the management of severe pediatric TBI.









Similar content being viewed by others
References
Kochanek PM, Clark RSB, Ruppel RA, et al. Biochemical, cellular, and molecular mechanisms in the evolution of secondary damage after severe traumatic brain injury in infants and children: lessons learned from the bedside. Pediatr Crit Care Med. 2000;1(1):4–19.
Lazaridis C, Rusin CG, Robertson CS. Secondary brain injury: predicting and preventing insults. Neuropharmacology. 2019;145:145–52.
Nangunoori R, Maloney-Wilensky E, Stiefel M, et al. Brain tissue oxygen-based therapy and outcome after severe traumatic brain injury: a systematic literature review. Neurocrit Care. 2012;17(1):131–8.
Lazaridis C. Cerebral oxidative metabolism failure in traumatic brain injury: “Brain shock.” J Crit Care. 2017;37:230–3.
Kochanek PM, Tasker RC, Bell MJ, et al. Management of Pediatric Severe Traumatic Brain Injury: 2019 Consensus and Guidelines-Based Algorithm for First and Second Tier Therapies. Pediatr Crit Care Med 2019.
Chang JJJ, Youn TS, Benson D, et al. Physiologic and functional outcome correlates of brain tissue hypoxia in traumatic brain injury. Crit Care Med. 2009;37(1):283–90.
Hirschi R, Hawryluk GWJ, Nielson JL, et al. Analysis of high-frequency PbtO2 measures in traumatic brain injury: Insights into the treatment threshold. J Neurosurg 2019.
Oddo M, Levine JM, MacKenzie L, et al. Brain hypoxia is associated with short-term outcome after severe traumatic brain injury independently of intracranial hypertension and low cerebral perfusion pressure. Neurosurgery. 2011;69(5):1037–45.
Narotam PK, Morrison JF, Nathoo N. Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy–clinical article. J Neurosurg. 2009;111(4):672–82.
Kochanek PM, Tasker RC, Carney N, et al. Guidelines for the management of pediatric severe traumatic brain injury, third edition: update of the brain trauma foundation guidelines. 2019.
Radolovich DK, Czosnyka M, Timofeev I, et al. Reactivity of brain tissue oxygen to change in cerebral perfusion pressure in head injured patients. Neurocrit Care. 2009;10(3):274–9.
Hawryluk GWJ, Aguilera S, Buki A, et al. A management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2019;45(12):1783–94.
Oddo M, Milby A, Chen I, et al. Hemoglobin concentration and cerebral metabolism in patients with aneurysmal subarachnoid hemorrhage. Stroke. 2009;40(4):1275–81.
Oddo M, Nduom E, Frangos S, et al. Acute lung injury is an independent risk factor for brain hypoxia after severe traumatic brain injury. Neurosurgery. 2010;67(2):338–44.
Robba C, Asgari S, Gupta A, et al. Lung injury is a predictor of cerebral hypoxia and mortality in traumatic brain injury. Front Neurol. 2020;11(August):1–10.
Okonkwo DO, Shutter LA, Moore C, et al. Brain tissue oxygen monitoring and management in severe traumatic brain injury (BOOST-II): a phase II randomized trial. Crit Care Med 2017;45(11).
Figaji AA, Zwane E, Kogels M, et al. The effect of blood transfusion on brain oxygenation in children with severe traumatic brain injury. Pediatr Crit Care Med. 2010;11(3):325–31.
Janz DR, Hollenbeck RD, Pollock JS, McPherson JA, Rice TW. Hyperoxia is associated with increased mortality in patients treated with mild therapeutic hypothermia after sudden cardiac arrest. Crit Care Med. 2012;40(12):3135–9.
Guerra-Wallace MM, Casey FL, Bell MJ, Fink EL, Hickey RW. Hyperoxia and hypoxia in children resuscitated from cardiac arrest. Pediatr Crit Care Med. 2013;14(3):143–8.
Numa A, Aneja H, Awad J, et al. Admission hyperoxia is a risk factor for mortality in pediatric intensive care. Pediatr Crit Care Med. 2018;19(8):699–704.
Ramgopal S, Dezfulian C, Hickey RW, et al. Association of severe hyperoxemia events and mortality among patients admitted to a pediatric intensive care unit. JAMA Netw open. 2019;2(8): e199812.
Pelletier JH, Ramgopal S, Au AK, Clark RSB, Horvat CM. Maximum Pao 2 in the first 72 hours of intensive care is associated with risk-adjusted mortality in pediatric patients undergoing mechanical ventilation. Crit Care Explor. 2020;2(9): e0186.
Demiselle J, Calzia E, Hartmann C, et al. Target arterial PO2 according to the underlying pathology: a mini-review of the available data in mechanically ventilated patients. Ann Intensive Care. 2021;11(1):1–9. https://doi.org/10.1186/s13613-021-00872-y.
Figaji AA, Zwane E, Graham Fieggen A, Argent AC, Le Roux PD, Peter JC. The effect of increased inspired fraction of oxygen on brain tissue oxygen tension in children with severe traumatic brain injury. Neurocrit Care. 2010;12(3):430–7.
Davis DP, Meade W, Sise MJ, et al. Both hypoxemia and extreme hyperoxemia may be detrimental in patients with severe traumatic brain injury. J Neurotrauma. 2009;26(12):2217–23.
Beynon C, Kiening KL, Orakcioglu B, Unterberg AW, Sakowitz OW. Brain tissue oxygen monitoring and hyperoxic treatment in patients with traumatic brain injury. J Neurotrauma. 2012;29(12):2109–23.
Dellazizzo L, Demers SP, Charbonney E, et al. Minimal PaO2 threshold after traumatic brain injury and clinical utility of a novel brain oxygenation ratio. In: J Neurosurg. 2019.
Alali AS, Temkin N, Vavilala MS, et al. Matching early arterial oxygenation to long-term outcome in severe traumatic brain injury: Target values. J Neurosurg. 2020;132(2):537–44.
Asher SR, Curry P, Sharma D, et al. Survival advantage and PaO2 threshold in severe traumatic brain injury. J Neurosurg Anesthesiol. 2013;25(2):168–73.
Ketharanathan N, De Jonge RCJ, Klouwen I, et al. Hyperoxia in pediatric severe traumatic brain injury (TBI): a comparison of patient classification by cutoff versus cumulative (area-under-the-curve) analysis. Brain Inj. 2020;34(7):958–64.
Weeden M, Bailey M, Gabbe B, Pilcher D, Bellomo R, Udy A. Functional outcomes in patients admitted to the intensive care unit with traumatic brain injury and exposed to hyperoxia: a retrospective multicentre cohort study. Neurocrit Care 2020.
Naylor JF, Borgman MA, April MD, Hill GJ, Schauer SG. Normobaric hyperoxia in wartime pediatric trauma casualties. Am J Emerg Med. 2020;38(4):709–14.
Ó Briain D, Nickson C, Pilcher D V., Udy AA. Early hyperoxia in patients with traumatic brain injury admitted to intensive care in Australia and New Zealand: a retrospective multicenter cohort study. Neurocrit Care 2018;29(3):443–51.
Adelson P, Bratton S, Carney N, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Pediatr Crit Care Med 2003;4(3 Suppl).
Kochanek P, Carney N, Adelson P, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents–second edition. Pediatr Crit Care Med. 2012;13(Suppl 1):S1-2.
Von Elm E, Egger M, Altman DG, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Br Med J. 2007;335(7624):806–8.
Dings J, Meixensberger J, Jäger A, Roosen K. Clinical experience with 118 brain tissue oxygen partial pressure catheter probes. Neurosurgery 1998.
Van Den Brink WA, Van Santbrink H, Steyerberg EW, et al. Brain oxygen tension in severe head injury. Neurosurgery 2000.
Ramgopal S, Dezfulian C, Hickey RW, et al. Association of severe hyperoxemia events and mortality among patients admitted to a pediatric intensive care unit. JAMA Netw Open 2019;2(8).
Raman S, Prince NJ, Hoskote A, Ray S, Peters MJ. Admission PaO2 and mortality in critically ill children: a cohort study and systematic review. Pediatr Crit Care Med. 2016;17(10):e444–50.
Pelletier JH, Ramgopal S, Horvat CM. Hyperoxemia is associated with mortality in critically ill children. Front Med. 2021;8: 675293.
Ferguson LP, Durward A, Tibby SM. Relationship between arterial partial oxygen pressure after resuscitation from cardiac arrest and mortality in children. Circulation. 2012;126(3):335–42.
del Castillo J, López-Herce J, Matamoros M, et al. Hyperoxia, hypocapnia and hypercapnia as outcome factors after cardiac arrest in children. Resuscitation. 2012;83(12):1456–61.
Guerra-Wallace MM, Casey FL, Bell MJ, Fink EL, Hickey RW. Hyperoxia and hypoxia in children resuscitated from cardiac arrest. Pediatr Crit Care Med 2013;14(3).
Lilien TA, Groeneveld NS, Van Etten-Jamaludin F, et al. Association of arterial hyperoxia with outcomes in critically ill children: a systematic review and meta-analysis. JAMA Netw Open. 2022;5(1):e2142105–e2142105.
W S Cleveland EGWMS. Local regression models. In: Compstat. Boca Raton, Fla: Chapman & Hall/CRC; 1992 p. Statistical Models in S. https://doi.org/10.1007/978-3-642-50096-1_48
The LOESS Procedure. SAS/STAT User’s Guide. Cary, NC: 2015.
Wood SN. Generalized Additive Models: An Introduction with R. Second. Chapman and Hall/CRC; 2017. Available from: https://www.routledge.com/Generalized-Additive-Models-An-Introduction-with-R-Second-Edition/Wood/p/book/9781498728331
Perkins NJ, Schisterman EF. The Youden index and the optimal cut-point corrected for measurement error. Biometr J. 2005;47(4):428–41.
Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biometr J. 2005;47(4):458–72.
Rosario BL, Horvat CM, Wisniewski SR, et al. Presenting characteristics associated with outcome in children with severe traumatic brain injury: A secondary analysis from a randomized, controlled trial of therapeutic hypothermia. Pediatr Crit Care Med. 2018;19(10):957–64.
Kirkman MA, Smith M. Brain oxygenation monitoring. Anesthesiol Clin. 2016;34(3):537–56.
Stiefel MF, Spiotta A, Gracias VH, et al. Reduced mortality rate in patients with severe traumatic brain injury treated with brain tissue oxygen monitoring. J Neurosurg. 2005;103(5):805–11.
Narotam PK, Burjonrappa SC, Raynor SC, Rao M, Taylon C. Cerebral oxygenation in major pediatric trauma: its relevance to trauma severity and outcome. J Pediatr Surg. 2006;41(3):505–13.
Figaji AA, Zwane E, Thompson C, et al. Brain tissue oxygen tension monitoring in pediatric severe traumatic brain injury : PPPart 1: Relationship with outcome. Child’s Nerv Syst. 2009;25(10):1325–33.
Lang EW, Mulvey JM, Mudaliar Y, Dorsch NWC. Direct cerebral oxygenation monitoring—a systematic review of recent publications. Neurosurg Rev. 2007;30(2):99–107.
Maloney-Wilensky E, Gracias V, Itkin A, et al. Brain tissue oxygen and outcome after severe traumatic brain injury: a systematic review. Crit Care Med. 2009;37(6):2057–63.
Stippler M, Ortiz V, Adelson PD, et al. Brain tissue oxygen monitoring after severe traumatic brain injury in children: relationship to outcome and association with other clinical parameters. J Neurosurg Pediatr. 2012;10(5):383–91.
Patchana T, Wiginton J, Brazdzionis J, et al. Increased brain tissue oxygen monitoring threshold to improve hospital course in traumatic brain injury patients. Cureus 2020.
Valadka AB, Hlatky R, Furuya Y, Robertson CS. Brain tissue PO2: Correlation with cerebral blood flow. In: Acta Neurochirurgica, Supplement. Acta Neurochir Suppl; 2002, p. 299–301.
Hlatky R, Valadka AB, Gopinath SP, Robertson CS. Brain tissue oxygen tension response to induced hyperoxia reduced in hypoperfused brain. J Neurosurg 2008.
Rosenthal G, Hemphill JC, Sorani M, et al. Brain tissue oxygen tension is more indicative of oxygen diffusion than oxygen delivery and metabolism in patients with traumatic brain injury. Crit Care Med. 2008;36(6):1917–24.
Jha RM, Elmer J, Zusman BE, et al. Intracranial pressure trajectories: A novel approach to informing severe traumatic brain injury phenotypes. Crit Care Med 2018.
Verweij BH, Muizelaar JP, Vinas FC, Peterson PL, Xiong Y, Lee CP. Impaired cerebral mitochondrial function after traumatic brain injury in humans. J Neurosurg 2000.
Ragan DK, McKinstry R, Benzinger T, Leonard JR, Pineda JA. Alterations in cerebral oxygen metabolism after traumatic brain injury in children. J Cereb Blood Flow Metab 2013;
Rockswold SB, Rockswold GL, Zaun DA, et al. A prospective, randomized clinical trial to compare the effect of hyperbaric to normobaric hyperoxia on cerebral metabolism, intracranial pressure, and oxygen toxicity in severe traumatic brain injury: clinical article. J Neurosurg. 2010;112(5):1080–94.
Diringer MN. Hyperoxia: good or bad for the injured brain? Curr Opin Crit Care. 2008;14(2):167–71.
Menzel M, Doppenberg EMR, Zauner A, et al. Cerebral oxygenation in patients after severe head injury: Monitoring and effects of arterial hyperoxia on cerebral blood flow, metabolism, and intracranial pressure. J Neurosurg Anesthesiol 1999.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstem AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9.
Funding
This effort was supported, in part, by grants 5T32HD040686-20 (JR, JHP), 5T32HD040686-17 (JA), 5K23NS104133 (AKA), and 1K23HD099331-01A1 (CMH). No sponsors were involved in the study design, collection, analysis or interpretation of data, the writing of the report, nor the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Drs. JR and JA conceptualized the study design and drafted the initial article. Dr. JR performed database extraction, data curation, and statistical coding for the analyses presented. Dr. JHP performed statistical coding and substantially revised the work. Drs. AKA, MJB, DWS, PMK, RSBC, and CMH reviewed the initial draft of the article, contributed additional analyses, and substantially revised the work. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
No author has any potential, perceived, or real conflict of interest.
Ethical Approval/Informed Consent
We confirm adherence to best practices including ethical guidelines for data collection and report that all aspects of this study were approved by the University of Pittsburgh Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rakkar, J., Azar, J., Pelletier, J.H. et al. Temporal Patterns in Brain Tissue and Systemic Oxygenation Associated with Mortality After Severe Traumatic Brain Injury in Children. Neurocrit Care 38, 71–84 (2023). https://doi.org/10.1007/s12028-022-01602-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01602-3