Abstract
Background
After cardiac arrest/resuscitation (CA/R), animals often had massive functional restrictions including spastic paralysis of hind legs, disturbed balance and reflex abnormalities. Patients who have survived CA also develop movement restrictions/disorders. A successful therapy requires detailed knowledge of the intrinsic damage pattern and the respective mechanisms. Beside neurodegenerations in the cerebellum and cortex, neuronal loss in the spinal cord could be a further origin of such movement artifacts.
Methods
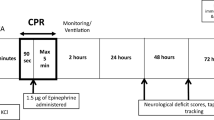
Thus, we aimed to evaluate the CA/R-induced degeneration pattern of the lumbar medulla spinalis by immunocytochemical expression of SMI 311 (marker of neuronal perikarya and dendrites), IBA1 (microglia marker), GFAP (marker of astroglia), calbindin D28k (marker of the cellular neuroprotective calcium-buffering system), MnSOD (neuroprotective antioxidant), the transcription factor PPARγ and the mitochondrial marker protein PDH after survival times of 7 and 21 days. The CA/R specimens were compared with those from sham-operated and completely naïve rats.
Results & Conclusion
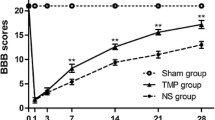
The main ACA/R-mediated results were: (1) degeneration of lumbar spinal cord motor neurons, characterized by neuronal pyknotization and peri-neuronal tissue artifacts; (2) attendant activation of microglia in the short-term group; (3) attendant activation of astroglia in the long-term group; (4) degenerative pattern in the intermediate gray matter; (5) activation of the endogenous anti-oxidative defense systems calbindin D28k and MnSOD; (6) activation of the transcription factor PPARγ, especially in glial cells of the gray matter penumbra; and (7) activation of mitochondria. Moreover, marginal signs of anesthesia-induced cell stress were already evident in sham animals when compared with completely naïve spinal cords. A correlation between the NDS and the motor neuronal loss could not be verified. Thus, the NDS appears to be unsuitable as prognostic tool.






Similar content being viewed by others
Abbreviations
- ACA/R:
-
Asphyxial cardiac arrest/resuscitation
- CTCF:
-
Corrected total cell fluorescence
- DAPI:
-
6-Diamidino-2-phenylindole
- ECG:
-
Electrocardiogram
- FCS:
-
Fetal calf serum
- GFAP:
-
Glial fibrillary acidic protein
- IBA1:
-
Ionized calcium binding adaptor molecule 1
- ID:
-
Integrated density
- IPPV:
-
Intermittent positive pressure ventilation
- LD:
-
Linear density
- MAP:
-
Mean arterial pressure
- MAP2:
-
Microtubule-associated protein 2
- MnSOD:
-
Manganese-dependent superoxide dismutase (mitochondrial SOD 2)
- PBS:
-
Phosphate-buffered saline
- PDH:
-
Pyruvate dehydrogenase
- PFA:
-
Phosphate-buffered paraformaldehyde
- PPARγ:
-
Peroxisome proliferator-activated receptor gamma
- ROSC:
-
Return of spontaneous circulation
- ST:
-
Survival time
References
Keilhoff G, Nguyen Thi TM, Esser T, Ebmeyer U. Relative resilience of cerebellar purkinje cells in a cardiac arrest/resuscitation rat model. Neurocrit Care. 2019;32:775–89.
Keilhoff G, Esser T, Titze M, Ebmeyer U, Schild L. High-potential defense mechanisms of neocortex in a rat model of transient asphyxia induced cardiac arrest. Brain Res. 2017;1674:42–54.
Keilhoff G, Esser T, Titze M, Ebmeyer U, Schild L. Gynostemma pentaphyllum is neuroprotective in a rat model of cardiopulmonary resuscitation. Exp Ther Med. 2017;14(6):6034–46.
Zulch KJ. Traumatic disturbances of the motoric and sensory system and their therapy. Deutsche Zeitschrift fur Nervenheilkunde. 1951;166(5):400–30.
Dambska M, Dydyk L, Szretter T, Wozniewicz J, Myers RE. Topography of lesions in newborn and infant brains following cardiac arrest and resuscitation. Damage to brain and hemispheres. Biol Neonate. 1976;29(3–4):194–206.
Towfighi J, Vannucci RC. Neuropathology of normothermic circulatory arrest in newborn dogs. Acta Neuropathol. 1997;93(5):485–93.
Kochanek PM, Tasker RC. Pediatric neurointensive care: 2008 update for the Rogers’ Textbook of Pediatric Intensive Care. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2009;10(4):517–23.
Wang B, Armstrong JS, Reyes M, Kulikowicz E, Lee JH, Spicer D, et al. White matter apoptosis is increased by delayed hypothermia and rewarming in a neonatal piglet model of hypoxic ischemic encephalopathy. Neuroscience. 2016;316:296–310.
Santos PT, O’Brien CE, Chen MW, Hopkins CD, Adams S, Kulikowicz E, et al. Proteasome biology is compromised in white matter after asphyxic cardiac arrest in neonatal piglets. J Am Heart Assoc. 2018;7(20):e009415.
Inamasu J, Nakatsukasa M, Hirose Y. Computed tomography evaluation of the brain and upper cervical spine in patients with traumatic cardiac arrest who achieved return of spontaneous circulation. Neurol Med Chir. 2013;53(9):585–9.
Klinke R, Pape HC, Silbernagl S. Physiologie. Stuttgart: Thieme; 2005.
Trepel M. Neuroanatomie. München: Urban & Fischer; 2004.
Schutz B. Imbalanced excitatory to inhibitory synaptic input precedes motor neuron degeneration in an animal model of amyotrophic lateral sclerosis. Neurobiol Dis. 2005;20(1):131–40.
O’Donnell R, Molon-Noblot S, Laroque P, Rigby M, Smith D. The ultrastructural localisation of the N-methyl-D-aspartate NR2B receptor subunit in rat lumbar spinal cord. Neurosci Lett. 2004;371(1):24–9.
Belov Kirdajova D, Kriska J, Tureckova J, Anderova M. Ischemia-triggered glutamate excitotoxicity from the perspective of glial cells. Front Cell Neurosci. 2020;14:51.
Martin LJ, Al-Abdulla NA, Brambrink AM, Kirsch JR, Sieber FE, Portera-Cailliau C. Neurodegeneration in excitotoxicity, global cerebral ischemia, and target deprivation: a perspective on the contributions of apoptosis and necrosis. Brain Res Bull. 1998;46(4):281–309.
Lau A, Tymianski M. Glutamate receptors, neurotoxicity and neurodegeneration. Pflugers Arch. 2010;460(2):525–42.
Duggal N, Lach B. Selective vulnerability of the lumbosacral spinal cord after cardiac arrest and hypotension. Stroke. 2002;33(1):116–21.
Keilhoff G, Titze M, Rathert H, Lucas B, Esser T, Ebmeyer U. Normoxic post-ROSC ventilation delays hippocampal CA1 neurodegeneration in a rat cardiac arrest model, but does not prevent it. Exp Brain Res. 2020;238(4):807–24.
Katz L, Ebmeyer U, Safar P, Radovsky A, Neumar R. Outcome model of asphyxial cardiac arrest in rats. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab. 1995;15(6):1032–9.
Widmer R, Engels M, Voss P, Grune T. Postanoxic damage of microglial cells is mediated by xanthine oxidase and cyclooxygenase. Free Radic Res. 2007;41(2):145–52.
Venkatesan A, Frucht S. Movement disorders after resuscitation from cardiac arrest. Neurol Clin. 2006;24(1):123–32.
Khot S, Tirschwell DL. Long-term neurological complications after hypoxic-ischemic encephalopathy. Semin Neurol. 2006;26(4):422–31.
Scheibe F, Neumann WJ, Lange C, Scheel M, Furth C, Kohnlein M, et al. Movement disorders after hypoxic brain injury following cardiac arrest in adults. Eur J Neurol. 2020. https://doi.org/10.1111/ene.14326.
Legriel S, Le Stang MB, Merceron S, Cronier P, Troche G. Ongoing abdominal status myoclonus in postanoxic coma. Neurocrit Care. 2012;16(1):136–8.
Caronna JJ, Finklestein S. Neurological syndromes after cardiac arrest. Stroke. 1978;9(5):517–20.
Gilles FH, Nag D. Vulnerability of human spinal cord in transient cardiac arrest. Neurology. 1971;21(8):833–9.
Sliwa JA, Maclean IC. Ischemic myelopathy: a review of spinal vasculature and related clinical syndromes. Arch Phys Med Rehabil. 1992;73(4):365–72.
Sladky JT, Rorke LB. Perinatal hypoxic/ischemic spinal cord injury. Pediatr Pathol. 1986;6(1):87–101.
Kuwamura M, Yoshida T, Yamate J, Kotani T, Sakuma S. Hereditary cerebellar vermis defect in the Lewis rat. Brain Res Dev Brain Res. 1994;83(2):294–8.
Liachenko S, Tang P, Hamilton RL, Xu Y. A reproducible model of circulatory arrest and remote resuscitation in rats for NMR investigation. Stroke. 1998;29(6):1229–38 (discussion 38–9).
Ahn JH, Lee TK, Kim B, Lee JC, Tae HJ, Cho JH, et al. Therapeutic hypothermia improves hind limb motor outcome and attenuates oxidative stress and neuronal damage in the lumbar spinal cord following cardiac arrest. Antioxidants. 2020;9(1):38.
Manto M, Bower JM, Conforto AB, Delgado-Garcia JM, da Guarda SN, Gerwig M, et al. Consensus paper: roles of the cerebellum in motor control–the diversity of ideas on cerebellar involvement in movement. Cerebellum. 2012;11(2):457–87.
Aravamuthan BR, Shoykhet M. Long-term increase in coherence between the basal ganglia and motor cortex after asphyxial cardiac arrest and resuscitation in developing rats. Pediatr Res. 2015;78(4):371–9.
Kudo Y, Ohtaki H, Dohi K, Yin L, Nakamachi T, Endo S, et al. Neuronal damage in rat brain and spinal cord after cardiac arrest and massive hemorrhagic shock. Crit Care Med. 2006;34(11):2820–6.
Moore JC. Neonatal neuropathology. Phys Occup Ther Pediatr. 1986;6(3–4):55–90.
Wu Y, Satkunendrarajah K, Fehlings MG. Riluzole improves outcome following ischemia-reperfusion injury to the spinal cord by preventing delayed paraplegia. Neuroscience. 2014;265:302–12.
Schwaller B. Cytosolic Ca2+ buffers. Cold Spring Harb Perspect Biol. 2010;2(11):a004051.
Palecek J, Lips MB, Keller BU. Calcium dynamics and buffering in motoneurones of the mouse spinal cord. J Physiol. 1999;520(Pt 2):485–502.
Burke RE, Baimbridge KG. Relative loss of the striatal striosome compartment, defined by calbindin-D28k immunostaining, following developmental hypoxic-ischemic injury. Neuroscience. 1993;56(2):305–15.
Timmermans JA, Bindels RJ, Van Os CH. Stimulation of plasma membrane Ca2+ pump by calbindin-D28k and calmodulin is additive in EGTA-free solutions. J Nutr. 1995;125(7 Suppl):1981S–6S.
Rosenfeld J, Cook S, James R. Expression of superoxide dismutase following axotomy. Exp Neurol. 1997;147(1):37–47.
Melov S, Schneider JA, Day BJ, Hinerfeld D, Coskun P, Mirra SS, et al. A novel neurological phenotype in mice lacking mitochondrial manganese superoxide dismutase. Nat Genet. 1998;18(2):159–63.
Reaume AG, Elliott JL, Hoffman EK, Kowall NW, Ferrante RJ, Siwek DF, et al. Motor neurons in Cu/Zn superoxide dismutase-deficient mice develop normally but exhibit enhanced cell death after axonal injury. Nat Genet. 1996;13(1):43–7.
Lindenau J, Noack H, Possel H, Asayama K, Wolf G. Cellular distribution of superoxide dismutases in the rat CNS. Glia. 2000;29(1):25–34.
Meyer M, Garay LI, Kruse MS, Lara A, Gargiulo-Monachelli G, Schumacher M, et al. Protective effects of the neurosteroid allopregnanolone in a mouse model of spontaneous motoneuron degeneration. J Steroid Biochem Mol Biol. 2017;174:201–16.
Aleshin S, Reiser G. Role of the peroxisome proliferator-activated receptors (PPAR)-alpha, beta/delta and gamma triad in regulation of reactive oxygen species signaling in brain. Biol Chem. 2013;394(12):1553–70.
Zolezzi JM, Santos MJ, Bastias-Candia S, Pinto C, Godoy JA, Inestrosa NC. PPARs in the central nervous system: roles in neurodegeneration and neuroinflammation. Biol Rev Camb Philos Soc. 2017;92(4):2046–69.
Iglesias J, Morales L, Barreto GE. metabolic and inflammatory adaptation of reactive astrocytes: role of PPARs. Mol Neurobiol. 2017;54(4):2518–38.
Lee EJ, Park JS, Lee YY, Kim DY, Kang JL, Kim HS. Anti-inflammatory and anti-oxidant mechanisms of an MMP-8 inhibitor in lipoteichoic acid-stimulated rat primary astrocytes: involvement of NF-kappaB, Nrf2, and PPAR-gamma signaling pathways. J Neuroinflamm. 2018;15(1):326.
Giampietro L, Gallorini M, De Filippis B, Amoroso R, Cataldi A, di Giacomo V. PPAR-gamma agonist GL516 reduces oxidative stress and apoptosis occurrence in a rat astrocyte cell line. Neurochem Int. 2019;126:239–45.
Kark RA, Rodriguez-Budelli M. Pyruvate dehydrogenase deficiency in spinocerebellar degenerations. Neurology. 1979;29(1):126–31.
Marangos PJ, Turkel CC, Dziewanowska ZE, Fox AW. Dichloroacetate and cerebral ischaemia therapeutics. Expert Opin Investig Drugs. 1999;8(4):373–82.
Miquel E, Cassina A, Martinez-Palma L, Bolatto C, Trias E, Gandelman M, et al. Modulation of astrocytic mitochondrial function by dichloroacetate improves survival and motor performance in inherited amyotrophic lateral sclerosis. PLoS ONE. 2012;7(4):e34776.
Putzu A, Valtorta S, Di Grigoli G, Haenggi M, Belloli S, Malgaroli A, et al. Regional differences in cerebral glucose metabolism after cardiac arrest and resuscitation in rats using [(18)F]FDG positron emission tomography and autoradiography. Neurocrit Care. 2018;28(3):370–8.
Kobrine AI, Evans DE, Rizzoli HV. The effects of ischemia on long-tract neural conduction in the spinal cord. J Neurosurg. 1979;50(5):639–44.
Acknowledgement
The authors wish to thank Leona Bück for the excellent technical assistance.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors have made substantive contributions to the study: GK: conceived the study, was responsible for data analyses, writing the manuscript and preparing the illustration of results. MT & HR: carried out surgery including post resuscitation care and tissue sampling. TMNT: carried out immunohistochemical stainings. UE: established the experimental model and supervised the animal experiments and critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval/informed consent
This study was granted according to the requirements of the German Animal welfare Act on the Use of Experimental Animals and the Animal Care and Use Committees of Saxony-Anhalt (permit number 42502-2-2-947 Uni MD).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Keilhoff, G., Titze, M., Rathert, H. et al. The Spinal Cord Damage in a Rat Asphyxial Cardiac Arrest/Resuscitation Model. Neurocrit Care 34, 844–855 (2021). https://doi.org/10.1007/s12028-020-01094-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01094-z