Abstract
South America is a subcontinent with 393 million inhabitants with widely distinct countries and diverse ethnicities, cultures, political and societal organizations. The epidemiological transition that accompanied the technological and demographic evolution is happening in South America and leading to a rise in the incidence of neurodegenerative and cardiovascular diseases that now coexist with the still high burden of infectious diseases. South America is also quite heterogeneous regarding the existence of systems of care for the various neurological emergencies, with some countries having well-organized systems for some diseases, while others have no plan of action for the care of patients with acute neurological symptoms. In this article, we discuss the existing systems of care in different countries of South America for the treatment of neurological emergencies, mainly stroke, status epilepticus, and traumatic brain injury. We also will address existing gaps between the current systems and recommendations from the literature to improve the management of such emergencies, as well as strategies on how to solve these disparities.


Similar content being viewed by others
References
Central Intelligence Agency. The 2012 World Factbook. https://www.cia.gov/library/publications/download/download-2012/ index.html. Cited 1 November 2018.
Ounpuu S, Anand S, Yusuf S. The impending global epidemic of cardiovascular diseases. Eur Heart J. 2000;21(11):880–3.
Asma S, Mensah GA, Warren CW, Henson R. Tobacco use and the cardiovascular disease epidemic in developing countries: global crises and opportunity in the making. Ethn Dis. 2003;13(2 Suppl. 2):S81–7.
Santosa A, Byass P. Diverse empirical evidence on epidemiological transition in low- and middle-income countries: population-based findings from INDEPTH network data. PLoS ONE. 2016;11(5):e0155753.
Albala C, Vio F, Yanez M. Epidemiological transition in Latin America: a comparison of four countries. Rev Med Chil. 1997;125(6):719–27.
Machado CV, Lima LD. Health policies and systems in Latin America: regional identity and national singularities. Cad Saude Publica. 2017;33(Suppl. 2):e00068617.
Becerra-Posada F, Minayo M, Quental C, de Haan S. National research for health systems in Latin America and the Caribbean: moving towards the right direction? Health Res Policy Syst. 2014;12:13.
Organization PAH. Report on epilepsy in Latin America and the Caribbean; 2013.
Health in the Americas. 2017. https://www.paho.org/salud-en-las-americas-2017/. Cited 17 January 2019.
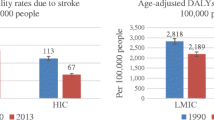
Lavados PM, Hennis AJ, Fernandes JG, et al. Stroke epidemiology, prevention, and management strategies at a regional level: Latin America and the Caribbean. Lancet Neurol. 2007;6(4):362–72.
Avezum A, Costa-Filho FF, Pieri A, Martins SO, Marin-Neto JA. Stroke in Latin America: Burden of disease and opportunities for prevention. Glob Heart. 2015;10(4):323–31.
Martins SCO, Sacks C, Hacke W, et al. Priorities to reduce the burden of stroke in Latin American countries. Lancet Neurol. 2019;18:674–83.
Lavados PM, Sacks C, Prina L, et al. Incidence, 30-day case-fatality rate, and prognosis of stroke in Iquique, Chile: a 2-year community-based prospective study (PISCIS project). Lancet. 2005;365(9478):2206–15.
Minelli C, Fen LF, Minelli DP. Stroke incidence, prognosis, 30-day, and 1-year case fatality rates in Matao, Brazil: a population-based prospective study. Stroke. 2007;38(11):2906–11.
Jaillard AS, Hommel M, Mazetti P. Prevalence of stroke at high altitude (3380 m) in Cuzco, a town of Peru. A population-based study. Stroke. 1995;26(4):562–8.
Silva FA, Zarruk JG, Quintero C, et al. Cerebrovascular disease in Colombia. Rev Colomb Cardiol. 2006;13(2):85–9.
Nicoletti A, Sofia V, Giuffrida S, et al. Prevalence of stroke : a door-to-door survey in rural Bolivia. Stroke. 2000;31(4):882–5.
Cabral NL, Goncalves AR, Longo AL, et al. Incidence of stroke subtypes, prognosis and prevalence of risk factors in Joinville, Brazil: a 2 year community based study. J Neurol Neurosurg Psychiatry. 2009;80(7):755–61.
Bestetti RB, Cardinalli-Neto A. Sudden cardiac death in Chagas’ heart disease in the contemporary era. Int J Cardiol. 2008;131(1):9–17.
Carod Artal FJ, Melo M, Vargas AP. Stroke of cardioembolic origin in Chagas disease. Rev Neurol. 2001;33(4):311–5.
Carod-Artal FJ, Vargas AP, Horan TA, Nunes LG. Chagasic cardiomyopathy is independently associated with ischemic stroke in Chagas disease. Stroke. 2005;36(5):965–70.
Oliveira-Filho J, Viana LC, Vieira-de-Melo RM, et al. Chagas disease is an independent risk factor for stroke: baseline characteristics of a Chagas disease cohort. Stroke. 2005;36(9):2015–7.
de Paiva Bezerra R, de Miranda Alves MA, Conforto AB, Rodrigues DLG, Silva GS. Etiological classification of Stroke in patients with Chagas disease using TOAST, causative classification system TOAST, and ASCOD phenotyping. J Stroke Cerebrovasc Dis. 2017;26(12):2864–9.
Camargo EC, Bacheschi LA, Massaro AR. Stroke in Latin America. Neuroimaging Clin N Am. 2005;15(2):283–96.
Fandino-Franky J, Silfvenius H. World-wide disparities in epilepsy care: a Latin American outlook. Epilepsia. 1999;40(Suppl. 8):48–54.
Burneo JG, Tellez-Zenteno J, Wiebe S. Understanding the burden of epilepsy in Latin America: a systematic review of its prevalence and incidence. Epilepsy Res. 2005;66(1–3):63–74.
Levav I, Stephenson C, Theodore W. Epilepsy in Latin America and the Caribbean: a survey on needs and resources. Rev Panam Salud Publica. 1999;6(5):342–5.
Escalaya AL, Tellez-Zenteno JF, Steven DA, Burneo JG. Epilepsy and mortality in Latin America. Seizure. 2015;25:99–103.
Bruno E, Bartoloni A, Zammarchi L, et al. Epilepsy and neurocysticercosis in Latin America: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2013;7(10):e2480.
Garzon E, Fernandes RM, Sakamoto AC. Analysis of clinical characteristics and risk factors for mortality in human status epilepticus. Seizure. 2003;12(6):337–45.
Puvanachandra P, Hyder AA. Traumatic brain injury in Latin America and the Caribbean: a call for research. Salud Publica Mex. 2008;50(Suppl. 1):S3–5.
Barreto SM, Miranda JJ, Figueroa JP, et al. Epidemiology in Latin America and the Caribbean: current situation and challenges. Int J Epidemiol. 2012;41(2):557–71.
Dewan MC, Rattani A, Gupta S, et al. Estimating the global incidence of traumatic brain injury. J Neurosurg. 2018;1:1–18.
Bonow RH, Barber J, Temkin NR, et al. The outcome of severe traumatic brain injury in Latin America. World Neurosurg. 2018;111:e82–90.
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80(1):6–15.
Organization WH. Guidelines for essential trauma care/World Health Organization, International Society of Surgery/Société Internationale de Chirurgie and the International Association for the Surgery of Trauma and Surgical Intensive Care (IATSIC), in Guidelines for essential trauma care/World Health Organization, International Society of Surgery/Société Internationale de Chirurgie and the International Association for the Surgery of Trauma and Surgical Intensive Care (IATSIC); 2004.
Meretoja A, Kaste M. Pre- and in-hospital intersection of stroke care. Ann N Y Acad Sci. 2012;1268:145–51.
Castilla-Guerra L, Serrano-Rodriguez L, Alpanseque-Hoogesteyn L, Fernandez-Moreno MC, Jimenez-Hernandez MD. Pre-hospital care of acute stroke: have we really improved? Rev Neurol. 2013;56(4):255–6.
Silverman EC, Sporer KA, Lemieux JM, et al. Prehospital care for the adult and pediatric seizure patient: current evidence-based recommendations. West J Emerg Med. 2017;18(3):419–36.
Pontes-Neto OM, Silva GS, Feitosa MR, et al. Stroke awareness in Brazil: alarming results in a community-based study. Stroke. 2008;39(2):292–6.
Díaz Cabezas R, Ruano Restrepo MI. Conocimiento de síntomas y factores de riesgo de enfermedad cerebro vascular en una población urbana colombiana. Acta Neurol Colomb. 2011;27(4):195–204.
Castaneda-Guarderas A, Beltran-Ale G, Casma-Bustamante R, Ruiz-Grosso P, Malaga G. Registry of patients with stroke stated in a public hospital of Peru, 2000–2009. Rev Peru Med Exp Salud Publica. 2011;28(4):623–7.
Davalos LF, Malaga G. Stroke in Peru: a forgotten and unattended prevalent disease. Rev Peru Med Exp Salud Publica. 2014;31(2):400–1.
Saavedra AG, Camejo C, Salamano R, Brunet F, Albisu S. Stroke care organization in public health of Montevideo, Uruguay. J Neurol Sci. 2015;357:e377.
Moro CH, Goncalves AR, Longo AL, et al. Trends of the incidence of ischemic stroke thrombolysis over seven years and one-year outcome: a population-based study in Joinville, Brazil. Cerebrovasc Dis Extra. 2013;3(1):156–66.
Sposato LA, Esnaola MM, Zamora R, et al. Quality of ischemic stroke care in emerging countries: the Argentinian National Stroke Registry (ReNACer). Stroke. 2008;39(11):3036–41.
Vancini RL, Benedito-Silva AA, Sousa BS, et al. Knowledge about epilepsy among health professionals: a cross-sectional survey in Sao Paulo, Brazil. BMJ Open. 2012;2(2):e000919.
Dantas FG, Cariri GA, Cariri GA, Ribeiro Filho ARV. Knowledge and attitudes toward epilepsy among primary, secondary and tertiary level teachers. Arq Neuropsiquiat. 2001;59(3):712–6.
Martins SC, Pontes Neto OM, Alves CV, et al. Past, present, and future of stroke in middle-income countries: the Brazilian experience. Int J Stroke. 2013;8(Suppl. A):106–11.
Silva GS, Rocha ECA, Pontes-Neto OM, Martins SO. Stroke care services in Brazil. J Stroke Med. 2018;1(1):51–4.
Caminiti C, Schulz P, Marcomini B, et al. Development of an education campaign to reduce delays in pre-hospital response to stroke. BMC Emerg Med. 2017;17(1):20.
DiBiasio EL, Jayaraman MV, Oliver L, et al. Emergency medical systems education may improve knowledge of pre-hospital stroke triage protocols. J Neurointerv Surg. 2018. https://doi.org/10.1136/neurintsurg-2018-014108.
Lemmel P. Role of pre-hospital and hospital emergency services in the management of stroke. Soins. 2018;63(828):33–5.
Lima FO, Silva GS, Furie KL, et al. Field assessment stroke triage for emergency destination: a simple and accurate prehospital scale to detect large vessel occlusion strokes. Stroke. 2016;47(8):1997–2002.
Hov MR, Lossius HM, Lund CG. Mechanical thrombectomy in stroke—the prehospital phase is crucial. Tidsskr Nor Laegeforen. 2017;137(12–13):860–1.
Ollikainen JP, Janhunen HV, Tynkkynen JA, et al. The Finnish prehospital stroke scale detects thrombectomy and thrombolysis candidates—a propensity score-matched study. J Stroke Cerebrovasc Dis. 2018;27(3):771–7.
Nogueira RG, Silva GS, Lima FO, et al. The FAST-ED app: a smartphone platform for the field triage of patients with stroke. Stroke. 2017;48(5):1278–84.
Chaudhry FS, Schneck MJ, Warady J, et al. Primary stroke center concept: strengths and limitations. Front Neurol. 2012;3:108.
LaBresh KA, Reeves MJ, Frankel MR, Albright D, Schwamm LH. Hospital treatment of patients with ischemic stroke or transient ischemic attack using the “Get With The Guidelines” program. Arch Intern Med. 2008;168(4):411–7.
Leifer D, Bravata DM, Connors JJ III, et al. Metrics for measuring quality of care in comprehensive stroke centers: detailed follow-up to Brain Attack Coalition comprehensive stroke center recommendations: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(3):849–77.
Stroke Unit Trialists’ Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2000;9(2):CD000197.
Sun Y, Paulus D, Eyssen M, Maervoet J, Saka O. A systematic review and meta-analysis of acute stroke unit care: what’s beyond the statistical significance? BMC Med Res Methodol. 2013;13:132.
Kaup AO, Dos Santos BF, Victor ES, et al. Georeferencing deaths from stroke in Sao Paulo: an intra-city stroke belt? Int J Stroke. 2015;10(Suppl. A):69–74.
Kuster GW, Bueno Alves M, Cendoroglo Neto M, Silva GS. Determinants of emergency medical services use in a Brazilian population with acute ischemic stroke. J Stroke Cerebrovasc Dis. 2013;22(3):244–9.
de Carvalho JJ, Alves MB, Viana GA, et al. Stroke epidemiology, patterns of management, and outcomes in Fortaleza, Brazil: a hospital-based multicenter prospective study. Stroke. 2011;42(12):3341–6.
Lavados PM, Hoppe WA. Stroke units in Chile. Rev Med Chil. 2005;133(11):1271–3.
Hoffmeister L, Lavados PM, Comas M, et al. Performance measures for in-hospital care of acute ischemic stroke in public hospitals in Chile. BMC Neurol. 2013;13:23.
Pontes-Neto OM, Cougo P, Martins SC, et al. Brazilian guidelines for endovascular treatment of patients with acute ischemic stroke. Arq Neuropsiquiatr. 2017;75(1):50–6.
Cabral NL, Conforto A, Magalhaes PSC, et al. Intravenous rtPA versus mechanical thrombectomy in acute ischemic stroke: a historical cohort in Joinville, Brazil. eNeurologicalSci. 2016;5:1–6.
Kuster GW, Dutra LA, Brasil IP, et al. Outcome determinants of stroke in a Brazilian primary stroke center. Stroke Res Treat. 2014;2014:194768.
de Carvalho FA, Schwamm LH, Kuster GW, et al. Get with the guidelines stroke performance indicators in a Brazilian tertiary hospital. Cerebrovasc Dis Extra. 2012;2(1):26–35.
Alves MB, Silva GS, Miranda RA, et al. Patterns of care, variations and temporal trends in stroke care: a Brazilian primary stroke center report. In: Stroke. 2016. Lippincott Williams & Wilkins Two Commerce SQ, 2001 Market ST, Philadelphia, Pa 19103 USA.
Martins SC. Endovascular treatment with stent-retriever and/or thromboaspiration vs. best medical therapy in acute ischemic stroke (RESILIENT); 2014. https://clinicaltrials.gov/ct2/show/NCT02216643. Cited 02 January 2019.
O’Phelan KH, Miller CM. Emergency neurological life support: third edition, updates in the approach to early management of a neurological emergency. Neurocrit Care. 2017;27(Suppl. 1):1–3.
Claassen J, Goldstein JN. Emergency neurological life support: status epilepticus. Neurocrit Care. 2017;27(Suppl. 1):152–8.
Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23.
Hernandez O, Zapata J, Jimenez M, et al. Refractory status epilepticus: experience in a neurological intensive care unit. J Crit Care Med. 2014;2014:9.
Chesnut RM, Temkin N, Carney N, et al. Traumatic brain injury in Latin America: lifespan analysis randomized control trial protocol*. Neurosurgery. 2012;71(6):1055–63.
Chesnut RM, Temkin N, Carney N, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012;367(26):2471–81.
Chesnut RM, Bleck TP, Citerio G, et al. A consensus-based interpretation of the benchmark evidence from South American trials: treatment of intracranial pressure trial. J Neurotrauma. 2015;32(22):1722–4.
Suarez JI, Zaidat OO, Suri MF, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med. 2004;32(11):2311–7.
Suarez JI. Outcome in neurocritical care: advances in monitoring and treatment and effect of a specialized neurocritical care team. Crit Care Med. 2006;34(9 Suppl):S232–8.
De Georgia M, Patel V. Critical care management in acute ischemic stroke. J Neurointerv Surg. 2011;3(1):34–7.
Diringer MN, Bleck TP, Claude Hemphill J III, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference. Neurocrit Care. 2011;15(2):211–40.
Mateen FJ. Neurocritical care in developing countries. Neurocrit Care. 2011;15(3):593–8.
Shrestha GS, Goffi A, Aryal D. Delivering neurocritical care in resource-challenged environments. Curr Opin Crit Care. 2016;22(2):100–5.
Mejia-Mantilla JH, Aristizabal-Mayor JD. Capacidad operativa de las unidades de cuidados intensivos colombianas y latinoamericanas en el manejo de la hemorragia subaracnoidea: un acercamiento preliminar. Acta Colomb Cuid Intensivo. 2017;17(4):241–6.
Moheet AM, Livesay SL, Abdelhak T, et al. Standards for neurologic critical care units: a statement for healthcare professionals from the neurocritical care society. Neurocrit Care. 2018;29(2):145–60.
Pandian JD, Gall SL, Kate MP, et al. Prevention of stroke: a global perspective. Lancet. 2018;392(10154):1269–78.
Acknowledgements
The Galapagos Neurocritical Care Summit was sponsored by the Universidad San Francisco de Quito, Ecuador and endorsed by the Neurocritical Care Society.
Funding
The Galapagos Neurocritical Care Summit was sponsored by the Universidad San Francisco de Quito, Ecuador and endorsed by the Neurocritical Care Society.
Author information
Authors and Affiliations
Consortia
Contributions
GSS and JIS designed, directed this review and drafted the manuscript; NJM, JHM, SOG, JC and PV participated in the conceptual framing of the study and revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Silva reports personal fees from Boehringer Ingelheim, personal fees from BARD, personal fees from Pfizer, Grants from Brazilian Ministry of Health, outside the submitted work. Dr. Maldonado has nothing to disclose. Dr. Mejia-Mantilla has nothing to disclose. Dr. Ortega receives Grants from Siemens, Society of vascular and Interventional Neurology. He is the site PI for 3 endovascular stroke trial at the University of Iowa including TESLA, SEGA and SELECT 2. Dr. Claassen reports Grants from Charles A. Dana Foundation , Grants from James S. McDonnell Foundation, from NIH: The Stroke Hyperglycemia Insulin Network Effort (SHINE) Trial, Grants from NIH: I-SPOT, Grants from NIH: Established Status Epilepticus Treatment Trial (ESETT), Grants from Bard: Intrepid, Grants from NIH: Futility Study of Deferoxamine Mesylate in Intracerebral Hemorrhage (I-DEF), Grants from NIH / NLM: BIGDATA: Causal Inference in Large-Scale Time Series with Rare and Latent Events, Grants from NIH: Rhapsody (ZZ-3K3A-201), other from iCE Neurosystems, outside the submitted work. Dr. Varelas reports Grants from Marinus, outside the submitted work. Dr. Suarez reports non-financial support and other from Neurocritical Care Society (President of the Neurocritical Care Society), non-financial support and other from Stroke Journal (member of the Editorial Board of Stroke), non-financial support and other from BARD (Chair of the DSMB for the INTREPID Study), outside the submitted work.
Ethical Approval/Informed Consent
No ethical approval is required for this type of study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
See “Appendix” for a full listing of investigators.
Appendix
Appendix
The Galapagos Neurocritical Care Summit Investigators (in alphabetical order)
-
Abdelhak Tamer, MD, Spectrum Health, Grand Rapids, MI, USA
-
Bader Mary K, RN, Mission Hospital St Joe Health, Mission Viejo, CA, USA
-
Brophy Gretchen, PharmD, Virginia Commonwealth University, Richmond, VA, USA
-
Calvillo Eusebia, RN, The Johns Hopkins University, Baltimore, MD, USA
-
Claassen Jan, Columbia University, New York, NY, USA
-
De Oliveira Manoel Airton Leonardo, MD, Sao Paulo, Brazil
-
Frontera Jennifer, MD, NYU Langone Health, Brooklyn, NY, USA
-
Georgiadis Alexandros, MD, Baylor College of Medicine, Houston, TX, USA
-
Greene-Chandos Diana, MD, Ohio State University, Columbus, OH, USA
-
Jijaba Manuel, MD, Hospital Eugenio Espejo, Quito, Ecuador
-
Lazaridis Christos, MD, University of Chicago, Chicago, IL, USA
-
Leira Enrique, MD, MS, University of Iowa, Iowa City, IA, USA
-
Lewandowski Chris, MD, Henry Ford Hospital, Detroit, MI, USA
-
Maldonado Nelson J, MD, Universidad San Francisco de Quito, Quito, Ecuador
-
Mejia-Mantilla Jorge, MD, Fundacion Valle del Lili, Cali, Colombia
-
Moretti Jose Ignacio, MD, Clinical Bicentenario, Santiago de Chile, Chile
-
Ontaneda Daniel, MD, The Cleveland Clinic Foundation, Cleveland, OH, USA
-
Ortega-Gutierrez Santiago, MD, University of Iowa, Iowa City, IA, USA
-
Samaniego Edgar, MD, University of Iowa, Iowa City, IA, USA
-
Sampaio Silva Gisele, MD, PhD, Federal University of Sao Paulo, Sao Paulo, Brazil
-
Silver Brian, MD, University of Massachusetts, Worcester, MA, USA
-
Spanaki Marianna, MD, Henry Ford Hospital, Detroit, MI, USA
-
Suarez Jose I, MD, The Johns Hopkins University, Baltimore, MD, USA
-
Torbey Michel, MD, MPH, University of New Mexico, Albuquerque, NM, USA
-
Varelas Panayiotis, MD, PhD, Henry Ford Hospital, Detroit, MI, USA
-
Venkatasubba Rao Chethan P, Baylor College of Medicine, Houston, TX, USA
-
Videtta Walter, MD, Hospital Nacional Posadas, Buenos Aires, Argentina.
Rights and permissions
About this article
Cite this article
Silva, G.S., Maldonado, N.J., Mejia-Mantilla, J.H. et al. Neuroemergencies in South America: How to Fill in the Gaps?. Neurocrit Care 31, 573–582 (2019). https://doi.org/10.1007/s12028-019-00775-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00775-8