Abstract
Background
Osmotic therapy is a critical component of medical management for cerebral edema. While up to 90% of neurointensivists report using these treatments, few quantitative clinical measurements guide optimal timing, dose, or administration frequency. Its use is frequently triggered by a qualitative assessment of neurologic deterioration and/or pupil size, and anecdotally appears to improve pupil asymmetry suggestive of uncal herniation. However, subjective pupil assessment has poor reliability, making it difficult to detect or track subtle changes. We hypothesized that osmotic therapy reproducibly improves quantitative pupil metrics.
Methods
We included patients at two centers who had recorded quantitative pupil measurements within 2 h before and after either 20% mannitol or 23.4% hypertonic saline in the neurosciences intensive care unit. The primary outcome was the Neurologic Pupil Index (NPi), a composite metric ranging from 0 to 5 in which > 3 is considered normal. Secondary outcomes included pupil size, percent change, constriction and dilation velocity, and latency. Results were analyzed with Wilcoxon signed-rank tests, Chi-square and multi-level linear regression to control for other edema-reducing interventions.
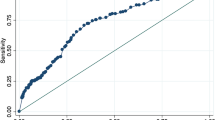
Results
Out of 72 admissions (403 paired pupil observations), NPi significantly differed within 2 h of osmotic therapy when controlling for other commonly used interventions in our whole cohort (β = 0.08, p = 0.0168). The effect was most pronounced (β = 0.57) in patients with abnormal NPi prior to intervention (p = 0.0235).
Conclusions
Pupil reactivity significantly improves after osmotic therapy in a heterogenous critically ill population when controlling for various other interventions. Future work is necessary to determine dose-dependent effects and clinical utility.
Similar content being viewed by others
References
Cadena R, Shoykhet M, Ratcliff JJ. Emergency neurological life support: intracranial hypertension and herniation. Neurocrit Care. 2017;27:82–8.
Hays AN, Lazaridis C, Neyens R, Nicholas J, Gay S, Chalela JA. Osmotherapy: use among neurointensivists. Neurocrit Care. 2011;14:222–8.
Qureshi AI, Geocadin RG, Suarez JI, Ulatowski JA. Long-term outcome after medical reversal of transtentorial herniation in patients with supratentorial mass lesions. Crit Care Med. 2000;28:1556–64.
Koenig MA, Bryan M, Lewin JL 3rd, Mirski MA, Geocadin RG, Stevens RD. Reversal of transtentorial herniation with hypertonic saline. Neurology. 2008;70:1023–9.
Francony G, Fauvage B, Falcon D, Canet C, Dilou H, Lavagne P, et al. Equimolar doses of mannitol and hypertonic saline in the treatment of increased intracranial pressure. Crit Care Med. 2008;36:795–800.
Ropper AH. The opposite pupil in herniation. Neurology. 1990;40:1707–9.
Mcnealy DE, Plum F. Brainstem dysfunction with supratentorial mass lesions. Arch Neurol. 1962;7:10–32.
Ropper AH. Lateral displacement of the brain and level of consciousness in patients with an acute hemispheral mass. N Engl J Med. 1986;314:953–8.
Ropper AH, Cole D, Louis DN. Clinicopathologic correlation in a case of pupillary dilation from cerebral hemorrhage. Arch Neurol. 1991;48:1166–9.
Fisher CM. Brain herniation: a revision of classical concepts. Can J Neurol Sci. 1995;22:83–91.
Olson DM, Stutzman S, Saju C, Wilson M, Zhao W, Aiyagari V. Interrater reliability of pupillary assessments. Neurocrit Care. 2016;24:251–7.
Couret D, Boumaza D, Grisotto C, Triglia T, Pellegrini L, Ocquidant P, et al. Reliability of standard pupillometry practice in neurocritical care: an observational, double-blinded study. Crit Care. 2016;20:99.
Meeker M, Du R, Bacchetti P, Privitera CM, Larson MD, Holland MC, et al. Pupil examination: validity and clinical utility of an automated pupillometer. J Neurosci Nurs. 2005;37:34–40.
R Development Core Team. R: a language and environment for statistical computing. 2016.
Papangelou A, Zink EK, Chang WW, Frattalone A, Gergen D, Gottschalk A, et al. Automated pupillometry and detection of clinical transtentorial brain herniation: a case series. Mil Med. 2018;183:e113–21.
Cruz J, Minoja G, Okuchi K. Major clinical and physiological benefits of early high doses of mannitol for intraparenchymal temporal lobe hemorrhages with abnormal pupillary widening: a randomized trial. Neurosurgery. 2002;51:628–37 (discussion 637-628).
Roberts I, Smith R, Evans S. Doubts over head injury studies. BMJ. 2007;334:392–4.
Diringer MN, Zazulia AR. Osmotic therapy: fact and fiction. Neurocrit Care. 2004;1:219–33.
Alvarez B, Ferrer-Sueta G, Radi R. Slowing of peroxynitrite decomposition in the presence of mannitol and ethanol. Free Radic Biol Med. 1998;24:1331–7.
Wise BL, Chater N. The value of hypertonic mannitol solution in decreasing brain mass and lowering cerebrospinal-fluid pressure. J Neurosurg. 1962;19:1038–43.
Grande PO, Romner B. Osmotherapy in brain edema: a questionable therapy. J Neurosurg Anesthesiol. 2012;24:407–12.
Rudehill A, Gordon E, Ohman G, Lindqvist C, Andersson P. Pharmacokinetics and effects of mannitol on hemodynamics, blood and cerebrospinal fluid electrolytes, and osmolality during intracranial surgery. J Neurosurg Anesthesiol. 1993;5:4–12.
Bentsen G, Breivik H, Lundar T, Stubhaug A. Hypertonic saline (7.2%) in 6% hydroxyethyl starch reduces intracranial pressure and improves hemodynamics in a placebo-controlled study involving stable patients with subarachnoid hemorrhage. Crit Care Med. 2006;34:2912–7.
Brophy GM, Human T, Shutter L. Emergency neurological life support: pharmacotherapy. Neurocrit Care. 2015;23(Suppl 2):S48–68.
Suarez JI, Qureshi AI, Bhardwaj A, Williams MA, Schnitzer MS, Mirski M, et al. Treatment of refractory intracranial hypertension with 23.4% saline. Crit Care Med. 1998;26:1118–22.
Ropper AH. Management of raised intracranial pressure and hyperosmolar therapy. Pract Neurol. 2014;14:152–8.
Paczynski RP. Osmotherapy. Basic concepts and controversies. Crit Care Clin. 1997;13:105–29.
Nau R. Osmotherapy for elevated intracranial pressure: a critical reappraisal. Clin Pharmacokinet. 2000;38:23–40.
Chen JW, Gombart ZJ, Rogers S, Gardiner SK, Cecil S, Bullock RM. Pupillary reactivity as an early indicator of increased intracranial pressure: the introduction of the neurological pupil index. Surg Neurol Int. 2011;2:82.
Kamel H, Navi BB, Nakagawa K, Hemphill JC 3rd, Ko NU. Hypertonic saline versus mannitol for the treatment of elevated intracranial pressure: a meta-analysis of randomized clinical trials. Crit Care Med. 2011;39:554–9.
Brown DA, Wijdicks EF. Decompressive craniectomy in acute brain injury. Handb Clin Neurol. 2017;140:299–318.
Shirozu K, Setoguchi H, Tokuda K, Karashima Y, Ikeda M, Kubo M, et al. The effects of anesthetic agents on pupillary function during general anesthesia using the automated infrared quantitative pupillometer. J Clin Monit Comput. 2017;31:291–6.
Larsen RS, Waters J. Neuromodulatory correlates of pupil dilation. Front Neural Circuits. 2018;12:21.
Ropper AH, Shafran B. Brain edema after stroke. Clinical syndrome and intracranial pressure. Arch Neurol. 1984;41:26–9.
Diggle PJ, Heagerty P, Liang K-Y, Zeger SL. Analysis of longitudinal data. Oxford: Oxford University Press; 2002. p. 31.
Author information
Authors and Affiliations
Contributions
CO was responsible for study design, analysis, interpretation of results, and the writing of the manuscript. MH assisted in statistical analysis of results and entering demographic and clinical data for patients. MB provided pharmacological expertise regarding osmotic therapy and manuscript review. AK was responsible for collecting pupillometry smart guards, entering demographic and clinical data, manuscript review and administrative duties regarding IRB submission process. SZ assisted in study design and collection, manuscript review. SS oversaw study design and provided expertise regarding analysis and interpretation of results.
Corresponding author
Ethics declarations
Source of Support
American Brain Foundation.
Conflict of interest
Dr. Ong reports grants from American Brain Foundation, during the conduct of the study. All other authors have nothing to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ong, C., Hutch, M., Barra, M. et al. Effects of Osmotic Therapy on Pupil Reactivity: Quantification Using Pupillometry in Critically Ill Neurologic Patients. Neurocrit Care 30, 307–315 (2019). https://doi.org/10.1007/s12028-018-0620-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0620-y