Abstract
Background
Guidelines recommend maintaining cerebral perfusion pressure (CPP) between 60 and 70 mmHg in patients with severe traumatic brain injury (TBI), but acknowledge that optimal CPP may vary depending on cerebral blood flow autoregulation. Previous retrospective studies suggest that targeting CPP where the pressure reactivity index (PRx) is optimized (CPPopt) may be associated with improved recovery.
Methods
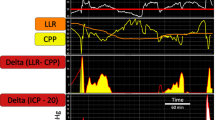
We performed a retrospective cohort study involving TBI patients who underwent PRx monitoring to assess issues of feasibility relevant to future interventional studies: (1) the proportion of time that CPPopt could be detected; (2) inter-observer variability in CPPopt determination; and (3) agreement between manual and automated CPPopt estimates. CPPopt was determined for consecutive 6-h epochs during the first week following TBI. Sixty PRx-CPP tracings were randomly selected and independently reviewed by six critical care professionals. We also assessed whether greater deviation between actual CPP and CPPopt (ΔCPP) was associated with poor outcomes using multivariable models.
Results
In 71 patients, CPPopt could be manually determined in 985 of 1173 (84%) epochs. Inter-observer agreement for detectability was moderate (kappa 0.46, 0.23–0.68). In cases where there was consensus that it could be determined, agreement for the specific CPPopt value was excellent (weighted kappa 0.96, 0.91–1.00). Automated CPPopt was within 5 mmHg of manually determined CPPopt in 93% of epochs. Lower PRx was predictive of better recovery, but there was no association between ΔCPP and outcome. Percentage time spent below CPPopt increased over time among patients with poor outcomes (p = 0.03). This effect was magnified in patients with impaired autoregulation (defined as PRx > 0.2; p = 0.003).
Conclusion
Prospective interventional clinical trials with regular determination of CPPopt and corresponding adjustment of CPP goals are feasible, but measures to maximize consistency in CPPopt determination are necessary. Although we could not confirm a clear association between ΔCPP and outcome, time spent below CPPopt may be particularly harmful, especially when autoregulation is impaired.






Similar content being viewed by others
Availability of Data and Material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CBF:
-
Cerebral blood flow
- CPP:
-
Cerebral perfusion pressure
- CPPopt :
-
“Optimal” cerebral perfusion pressure
- DC:
-
Decompressive craniectomy
- eGOS:
-
Extended Glasgow Outcome Scale
- ICP:
-
Intracranial pressure
- MAP:
-
Mean arterial pressure
- PRx:
-
Pressure reactivity
- TBI:
-
Traumatic brain injury
References
Chesnut RM, Marshall LF, Klauber MR, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34:216–22.
Manley G, Knudson MM, Morabito D, et al. Hypotension, hypoxia, and head injury: frequency, duration, and consequences. Arch Surg. 2001;136:1118–23.
McHugh GH, Engel DC, Butcher I, et al. Prognostic value of secondary insults in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24:287–93.
Changaris DG, McGraw CP, Richardson JD, et al. Correlation of cerebral perfusion pressure and Glasgow Outcome Scale to outcome. J Trauma. 1987;27:1007–13.
Juul N, Morris GF, Marshall SB, Marshall LF. Intracranial hypertension and cerebral perfusion pressure: influence on neurological deterioration and outcome in severe head injury. J Neurosurg. 2000;92:1–6.
Clifton GL, Miller ER, Choi SC, Levein HS. Fluid thresholds and outcome from severe brain injury. Crit Care Med. 2002;30:739–45.
Elf K, Nilsson P, Ronne-Engstrom E, et al. Cerebral perfusion pressure between 50 and 60 mmHg may be beneficial in head-injured patients: a computerized secondary insult monitoring study. Neurosurgery. 2005;56:962–71.
Johnson U, Nilsson P, Ronne-Engstrom E, et al. Favorable outcome in traumatic brain injury patients with impaired cerebral perfusion pressure autoregulation when treated at low cerebral perfusion pressure levels. Neurosurgery. 2011;68:714–21.
Balestreri M, Czosnyka M, Hutchinson P, et al. Impact of intracranial pressure and cerebral perfusion pressure on severe disability and mortality after head injury. Neurocrit Care. 2006;4:8–13.
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury, 4th edition. http://www.braintrauma.org. Accessed Nov 23, 2016.
Czosnyka M, Smielewski P, Kirkpatrick P, et al. Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery. 1997;41:11–7.
Steiner LA, Coles JP, Johnston AJ, et al. Assessment of cerebrovascular autoregulation in head-injured patients: a validation study. Stroke. 2003;34:2404–9.
Brady KM, Lee JK, Kibler KK, et al. Continuous measurement of autoregulation by spontaneous fluctuations in cerebral perfusion pressure: comparison of 3 methods. Stroke. 2008;39:2531–7.
Steiner LA, Czosnyka M, Piechnik SK, et al. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med. 2002;30:733–8.
Sanchez-Porras R, Santos E, Czosnyka M, et al. ‘Long’ pressure reactivity index (L-PRx) as a measure of autoregulation correlates with outcome in traumatic brain injury patients. Acta Neurochir. 2012;154:1575–81.
Johnson U, Lewen A, Ronne-Engstrom E, et al. Should the neurointensive care management of traumatic brain injury patients be individualized according to autoregulation status and injury subtype? Neurocrit Care. 2014;21:259–65.
Dias C, Silva MJ, Pereira E, et al. Optimal cerebral perfusion pressure management at bedside: a single-center pilot study. Neurocrit Care. 2015;23:92–102.
Depretiere B, Guiza F, Van den Berghe G, et al. Pressure autoregulation monitoring and cerebral perfusion pressure target recommendation in patients with severe traumatic brain injury based on minute-by-minute monitoring data. J Neurosurg. 2014;120:1451–7.
Needham E, McFadyen C, Newcombe V, et al. Cerebral perfusion pressure targets individualized to pressure-reactivity index in moderate to severe traumatic brain injury: a systematic review. J Neurotrauma. 2016;33:1–8.
Steijn R, Stewart R, Czosnyka M, et al. Survey in expert clinicians on validity of automated calculation of optimal cerebral perfusion pressure. Minerva Anesthesiol 2017 (Epub ahead of print).
Aries MJH, Czosnyka M, Budohoski KP, et al. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40:2456–63.
Brain Trauma Foundation. Guidelines for the management of severe traumatic brain injury. VIII. Intracranial pressure thresholds. J Neurotrauma. 2007;24:S55–8.
Kramer AH, Deis N, Ruddell S, et al. Decompressive craniectomy in patients with traumatic brain injury: are the usual indications congruent with those evaluated in clinical trials? Neurocrit Care. 2016;25:109.
Liu X, Maurits NM, Aries MJH, et al. Monitoring of optimal cerebral perfusion pressure in traumatic brain injured patients using a multi-window weighting algorithm. J Neurotrauma. 2017;15:3081–8.
Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psych Bull. 1968;70:213–20.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Wilson JT, Pettigrew LE, Teasdale GM. Structure interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma. 1998;15:573–85.
Murray GD, Butcher I, McHugh G, et al. Multivariable prognostic analysis in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24:329–37.
Preiksatis A, Krakauskaite S, Petkus V, et al. Association of severe traumatic brain injury patient outcomes with duration of cerebrovascular autoregulation impairment events. Neurosurgery. 2016;79:75–82.
Robertson CS, Valadka AB, Hannay HJ, et al. Prevention of secondary ischemic insults after severe head injury. Crit Care Med. 1999;27:2086–95.
Okonkwo DO, Shutter LA, Moore C, et al. Brain oxygen optimization in severe traumatic brain injury phase-II: a phase II randomized trial. Crit Care Med. 2017;45:1907–14.
Thiara S, Griesdale DE, Henderson WR, Sekhon MS. Effect of cerebral perfusion pressure on acute respiratory distress syndrome. Can J Neurol Sci 2018; (Epub ahead of print).
Donnelly J, Czosnyka M, Adams H, et al. Individualizing thresholds of cerebral perfusion pressure using estimated limits of autoregulation. Crit Care Med. 2017;45:1464–71.
Lazaridis C, DeSantis SM, Smielewski P, et al. Patient-specific thresholds of intracranial pressure in severe traumatic brain injury. J Neurosurg. 2014;120:893–900.
Sorrentino E, Diedler J, Kasprowicz M, et al. Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocrit Care. 2012;16:258–66.
Zeiler FA, Donnelly J, Smielewski P, et al. Critical thresholds of ICP derived continuous cerebrovascular reactivity indices for outcome prediction in non-craniectomized TBI patients: PRx, PAx and RAC. J Neurotrauma 2017 (Epub ahead of print).
Pesek M, Kibler K, Easley RB, et al. The upper limit of cerebral blood flow autoregulation is decreased with elevations in intracranial pressure. Neurosurgery. 2014;75:163–70.
http://cppopt.org/research-projects-cogitate Accessed Mar 15 2018.
Acknowledgements
The authors acknowledge several critical care professionals who participated in the assessment of inter-observer variability: Tomas Godinez MD, Colin Casault MD, Jason Waechter MD, Laura Robinson RN, and Sandy Manuel RN.
Funding
This study was performed without any dedicated funding. One of the authors (CG) received funding from the Department of Clinical Neurosciences at the University of Calgary for the purchase of ICM+ licenses and equipment. Alberta Health Services provided information technology support.
Author information
Authors and Affiliations
Contributions
AK conceived the study, analyzed and interpreted the data, and wrote the first draft of the manuscript; PC participated in the assessment of inter-observer variability, and assisted with the interpretation of data and writing of the final manuscript; DZ helped with the interpretation of data and writing of the final manuscript; MA assisted with refining the study questions, provided technical assistance with the use of ICM+ software, and assisted with the interpretation of data; CG participated in the assessment of inter-observer variability and assisted with the interpretation of data and writing of the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for Publication
No identifiable information has been presented.
Ethics Approval and Consent to Participate
This study was approved by the Conjoint Health Research Ethics Boards at the University of Calgary. The need for consent was waived.
Rights and permissions
About this article
Cite this article
Kramer, A.H., Couillard, P.L., Zygun, D.A. et al. Continuous Assessment of “Optimal” Cerebral Perfusion Pressure in Traumatic Brain Injury: A Cohort Study of Feasibility, Reliability, and Relation to Outcome. Neurocrit Care 30, 51–61 (2019). https://doi.org/10.1007/s12028-018-0570-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0570-4