Abstract
Background
Acute cerebral complications (ACC) of veno-arterial extracorporeal membrane oxygenation (VA-ECMO) are associated with poor long-term neurologic outcome. We described the role of rSO2 monitoring in detecting ACC and desaturations and their relationship with poor outcome when employing VA-ECMO.
Methods
Retrospective analysis of patients monitored by cerebral frontal near-infrared spectroscopy (NIRS) (CAS Medical Systems Inc., Branford, CT, USA) during VA-ECMO (November 2008–December 2015). ACC was defined as the presence of stroke and/or brain death, while cerebral desaturation as cortical oxygen tissue saturation (rSO2) < 60%.
Results
Fifty-six of 159 VA-ECMO patients (age 55 [36–60] years) were included; 18 (32%) developed ACC and 36 died (64%). Cerebral desaturation occurred in 43 (74%) patients, who had a higher mortality than those without cerebral desaturation (74 vs. 31%). A high sequential organ failure assessment (SOFA) score on the first day of ECMO (OR 1.40 [95% CIs 1.06–1.84]) and the minimum ECMO blood flow during the first 4 days of therapy (OR 3.05 [1.01–9.17]) were independently associated with the occurrence of cerebral desaturation. Cerebral desaturation occurred more frequently in patients with ACC than others (94 vs. 68%); patients with ACC also had a lower minimal rSO2 over time (49 vs. 54%) and more frequently had high right-left rSO2 differences (33 vs. 8%), which were both independent predictors of ACC. The occurrence of cerebral desaturation (OR 7.93 [1.62–38.74]) and high lactate concentrations during the first 4 days of ECMO support (OR 1.22 [1.03–1.46]) was independently associated with hospital mortality.
Conclusions
Monitoring of rSO2 could be considered as an interesting tool to monitor the brain of patients on VA-ECMO.
Similar content being viewed by others
Introduction
In the last decade, the number of patients treated with extracorporeal membrane oxygenation (ECMO) for cardiopulmonary failure has increased significantly, in both adult and pediatric populations [1]. Despite playing a lifesaving role in emergency settings, use of ECMO can be associated with a number of major complications [2, 3]. Among these, neurological complications, including ischemic/hemorrhagic stroke or seizures, are associated with longer hospital stay and increased mortality [4, 5]. In addition, the “differential hypoxia” syndrome, defined as lower arterial oxygen pressure (PaO2) in the upper body than in the lower body, can lead to important neurological complications in patients undergoing peripheral veno-arterial ECMO (VA-ECMO). This syndrome usually occurs when, in the presence of respiratory failure, cardiac function improves and the blood coming from the native left ventricle mixes with the retrograde blood flow coming from the arterial cannula of the ECMO machine. In this situation, the upper part of the body, including the brain, receives poorly oxygenated blood [6].
As patients undergoing VA-ECMO support usually require sedation, a clinical neurological examination is not always feasible or reliable. For this reason, neurological monitoring is crucial to detect and potentially limit neurological complications. Among the tools that can be employed to monitor the brain in such patients, cerebral near-infrared spectroscopy (NIRS) may have an important role. This noninvasive monitoring technique can provide a continuous value of forehead regional oxygen tissue saturation (rSO2), which represents the balance between cerebral oxygen delivery and cerebral oxygen consumption. Monitoring of rSO2 can also give information on changes in relationship to baseline values over time and on the response of cerebral oxygenation to therapeutic interventions; it may also help detect a sudden bilateral or unilateral (right or left) drop in rSO2, which is associated with cerebrovascular events [7]. NIRS has largely been used in patients undergoing cardiopulmonary bypass during cardiac surgery, where NIRS-guided optimization of oxygen delivery has been associated with a reduction in stroke incidence and in the occurrence of organ dysfunction [8, 9].
However, the use of NIRS as a tool for neuromonitoring in adult patients undergoing VA-ECMO has only been described by Wong et al. [10] in a small cohort study. The aim of the present study was, therefore, to describe the role of rSO2 monitoring in detecting acute cerebral complications (ACC), differential hypoxia and its relationship with poor outcome in patients receiving VA-ECMO.
Methods
Study Population
This was a retrospective study performed in a 35-bed Department of Intensive Care. The local Ethical Committee (Comité d’Ethique Hospitalo-Facultaire Erasme-ULB) approved the study (Protocol 2017/263), but waived the need for informed consent because of the retrospective design. All patients receiving VA-ECMO who were included in our institutional register of ECMO patients (November 2008–December 2015) and who had concomitant cerebral NIRS monitoring were included.
Data Collection and Definition
We collected data on demographics, indications for and duration of VA-ECMO support, sequential organ failure assessment (SOFA) score on the day of ECMO initiation, duration of cerebral NIRS monitoring, occurrence of ACC, differential hypoxia and seizures, and hospital mortality. Some basic patients’ characteristics were also collected for patients undergoing VA-ECMO over the study period without rSO2 monitoring. We also collected results of arterial and venous blood gas analyses, mechanical ventilation settings and ECMO parameters, on a daily basis for at least 4 days. If the patient had also undergone concomitant EEG monitoring (continuous or intermittent), we collected EEG background patterns (i.e., mild/moderate or severe encephalopathy, presence of flat/burst suppression) and the presence of epileptiform activity (i.e., seizures, periodic discharges [PEDs], or generalized periodic discharges [GPEDs]), according to the neurologist’s report, as previously described [11]; only the worst finding was recorded. ACC was defined as the presence of ischemic or hemorrhagic lesions on cerebral tomography (CT) scans and/or brain death. Differential hypoxia was defined as poorly oxygenated blood (i.e., PaO2 < 55 mmHg measured in the right radial artery), ejected into the ascending aorta from the left ventricle in the presence of lung injury, which competes with retrograde flow from the peripheral ECMO circuit, potentially causing myocardial and cerebral ischemia [6].
Neurological outcome was assessed 3 months after VA-ECMO insertion using the Glasgow Outcome Scale (GOS; 1 = death or severe injury without recovery of consciousness; 2 = persistent vegetative state; 3 = severe injury with permanent need for help with daily living; 4 = moderate disability with no need for assistance in everyday life; 5 = limited disability with minor neurological and psychological deficits) [12]. The GOS evaluation was assessed during follow-up visits or by telephone interview with the general practitioner. Favorable neurological outcome was considered as a GOS 4–5; unfavorable outcome as GOS 1–3.
VA-ECMO Management
The veno-arterial ECMO was implanted surgically or percutaneously using femoro-femoral heparin-coated cannulation (18-22Fr arterial cannula and 25Fr venous cannula; Edwards Lifesciences, Irvine, CA, USA). Transesophageal echocardiography was performed to confirm the correct position of the venous cannula in the inferior vena cava at its entry to the right atrium. A centrifugal blood pump (Revolution blood pump, Sorin, Milano, Italy) was initially set at a blood flow of 3–4 L/min (based on the body surface area). ECMO priming consisted of 700 mL of a balanced crystalloid solution (PlasmalyteR, Baxter Healthcare Corporation, Deerfield, IL, USA). At the end of the implantation, the leg was perfused with an anterograde single lumen 8Fr catheter (Arrow Inc., Reading, PA, USA) to prevent limb ischemia. When VA-ECMO was placed because of refractory cardiac arrest (i.e., extracorporeal cardiopulmonary resuscitation [ECPR]), the heat exchanger on the ECMO circuit was used to maintain body temperature at 34 °C for 24 h. The patient was then slowly rewarmed (less than 0.5 °C/h). In non-cardiac arrest patients, normothermia (body temperature around 37 °C) was maintained. After ECMO implantation, the ICU physician inserted an echo-guided radial or brachial arterial catheter (Vygon, Ecouen, France) in the right arm. FiO2 and gas flow of the ECMO oxygenator (EOS, Sorin, Milano, Italy) were adapted to maintain PaO2 between 70 and 150 mmHg and PaCO2 between 35 and 45 mmHg, with prior adaptation of the ventilator for protective ventilation associated with the lowest FiO2 using the right arm arterial catheter. When these targets were not achieved (e.g., severe respiratory failure or differential hypoxia), increasing ECMO blood flows, reducing inotropes, and giving diuretics were the first-line therapeutic interventions. In case of persistent severe hypoxemia, a reentry venous cannula was placed in the jugular vein and a veno–veno-arterial configuration (VVA) achieved. Systemic anticoagulation was achieved by intravenous administration of unfractionated heparin. Optimal mean arterial pressure (usually > 70 mmHg) was achieved by adjusting ECMO blood flow (to a maximum of 5.5 L/min) or by giving norepinephrine.
NIRS Monitoring
The cerebral NIRS monitoring used in the present study was a Foresight-Elite (CAS Medical Systems Inc, Branford, CT, USA) that has been extensively described elsewhere [13, 14]. Briefly, the NIRS monitoring was connected to the patients as soon as possible after ECMO initiation according to the decision of the attending physician and availability of the device. Two sensors were placed on the patient’s forehead, emitting and receiving light in the near-infrared spectrum (700–900-nm wavelength). This device uses five wavelengths of infrared light (680, 730, 770, 805, and 870 nm). It is based on the principle of spatially resolved spectroscopy: an array of closely spaced detectors measures light attenuation by hemoglobin, as a function of source–detector separation. It provides an absolute value of rSO2, which reflects the balance between cerebral oxygen supply and cerebral oxygen demand, according to a specific algorithm developed by the producer. The normal value in healthy volunteers is > 60% [15].
The decision to initiate rSO2 monitoring was related to the decision of the attending physicians (in particular post-anoxic injury, deep sedation preventing any neurological examination or severe extracranial bleeding) and the availability of the device (i.e., two devices were available at the moment of the study and were generally used to monitor patients resuscitated from cardiac arrest without ECMO, patients with subarachnoid hemorrhage or with sepsis). In this study, rSO2 values were collected every 2 s and stored on the device memory. At the end of the monitoring period, data were recorded on a USB key and analyzed off-line using specific software (ForeSight Data Analysis V2.0) provided by the company. A median value for the two cerebral hemispheres was obtained and used for final rSO2 analysis. We collected the baseline value (i.e., median rSO2 over the first minute of monitoring), the lowest rSO2 values over the entire monitoring period and the percentage of time spent under the threshold of 60% (T < 60%). In addition, we recorded episodes of “cerebral desaturation,” which was defined as a T < 60% for more than 5% of the entire monitoring period, and the maximum differential between right and left rSO2 (ΔrSO2). For ΔrSO2, we also reported whether patients had a ΔrSO2 > 10% for more than 2 consecutive minutes. Attending physicians were aware of rSO2 values, so that in case of cerebral desaturation, they first excluded the presence of differential hypoxia and then proceeded to improve brain perfusion by increasing blood pressure and/or cardiac output, increasing PaCO2 if < 40 mmHg, increasing ECMO blood flow, giving red blood cell (RBC) transfusions, or decreasing cerebral consumption (i.e., increasing sedative or analgesic drugs, reducing body temperature, treating seizures).
Statistical Analysis
Continuous variables are expressed as means ± standard deviation (SD) or median (25th to 75th percentiles) and discrete variables as counts (percentage). The Kolmogorov–Smirnov test was used, and histograms and normal-quartile plots were examined to verify the normality of distribution of continuous variables. Demographics and clinical differences between groups (survivors and non-survivors, and patients with or without cerebral desaturation) were assessed using the χ2 test, Fisher’s exact test, Student’s t test, or Mann–Whitney U test, as appropriate.
We performed three multivariable logistic regression analyses to identify variables independently associated with cerebral desaturation, ACC and hospital mortality; colinearity between variables was excluded prior to modeling. Only variables associated with cerebral desaturation, ACC, and hospital mortality, respectively, on a univariate basis were introduced in the multivariable models. Odds ratios (OR) with 95% confidence intervals (CI) were computed. The receiver operating characteristic curve was constructed for each multivariable model to obtain the area under the curve (AUC) and relative 95% interval of confidence of the models.
A p value < 0.05 was considered as statistically significant. Data were analyzed using IBM® SPSS® Statistics software, version 22.0 for Windows, and R software, version 3.1.0 (CRAN project).
Results
Study Population
During the study period, 159 patients were treated with VA-ECMO. Of those, 103 did not receive NIRS monitoring (median age 52 [41–60] years, 58% cardiogenic shock and 24% ECPR; hospital mortality 55%) leaving 56 eligible for the final analysis: 29 (52%) with cardiogenic shock, 22 (39%) with ECPR, and 5 (15%) with graft dysfunction after lung or heart transplantation. The duration of ECMO therapy was 6 [3–9] days. Patient characteristics are summarized in Table 1.
Eighteen patients (32%) developed ACC; of those, 8 had an ischemic (n = 7, 1 in the posterior circulation) or hemorrhagic (n = 1) stroke, 8 were diagnosed with brain death after ECPR, and 2 developed both ischemic stroke and brain death. Two patients had seizures (both after ECPR). Thirty-six patients (64%) died in hospital.
NIRS Variables
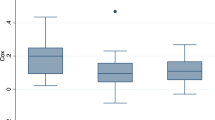
NIRS monitoring was placed after a median of 1 [1, 2] day after ECMO initiation and was continued for 3 [2–4] days. The baseline rSO2 was 63 [61–66]% and was similar among the different indications for VA-ECMO (Table 1). Cerebral desaturation occurred in 43 (74%) patients; rSO2 was < 60, 55, or 50% for 19, 4, and 0%, respectively, of the total duration of NIRS monitoring (Table 1). The highest ΔrSO2 was 6 [5–8]%, and the lowest rSO2 was 53 [49–55]%. Some examples of rSO2 values over time in individual patients are shown in Fig. 1.
Time course of rSO2 values in four different patients; a changes in rSO2 values according to changes in arterial carbon dioxide levels (PaCO2). b Persistent left–right rSO2 difference over time despite modification in blood pressure and ECMO blood flow. c Persistent rSO2 values above the minimal threshold of 60%. d Persistent rSO2 values below the minimal threshold of 60% despite several therapeutic interventions; the patient developed brain death on day 3 after an anoxic brain injury
Outcomes
Cerebral Desaturation
Patients with cerebral desaturation had a higher SOFA score on the day of ECMO initiation, a higher mean minimum ECMO flow, lower hemoglobin levels and a lower ScvO2 despite more RBC transfusions than those without cerebral desaturation (Table 2). Baseline rSO2 was lower in patients who developed cerebral desaturation than in those who did not, although the maximal ΔrsO2 was similar in the two groups. All episodes of ACC occurred in patients with cerebral desaturation. Seven of the patients with cerebral desaturation developed differential hypoxia; in 3 of them, VA-ECMO was finally converted into VVA-ECMO because other interventions did not correct this abnormality. Hospital mortality was significantly higher in patients with cerebral desaturation than in those without (32/43 [74%] vs. 4/13 [31%]).
Acute Cerebral Complication
Patients who developed ACC had lower PaO2 values during ECMO therapy and more frequently had EEG abnormalities, such as severe encephalopathy, GPDEs/PEDs, or flat/burst suppression background, than those who did not develop ACC (Table 2). Patients who developed ACC more frequently had cerebral desaturation than those who did not (17/18, 94 vs. 26/38, 68%—p < 0.01), despite a similar baseline rSO2. Among the 10 patients who had a stroke, 7/10 had a ΔrSO2 ≥ 10% (one of the 3 with ΔrSO2 < 10% had a posterior circulation stroke—Figs. 2 and 3). Patients who developed ACC also had a lower “lowest rSO2” and a longer period below different rSO2 thresholds than the other patients. Hospital mortality and poor neurological outcome were more frequent in patients who developed ACC.
Hospital Mortality
Hospital non-survivors had a higher SOFA score on the day of ECMO initiation, and a lower pH, lower hemoglobin levels and higher lactate concentrations during the first 4 days of ECMO therapy than did survivors (Table 2). Non-survivors had a lower baseline rSO2 and a lower “lowest” rSO2 value; they also more frequently developed cerebral desaturation and spent a longer time below different thresholds of rSO2 than survivors. Non-survivors also more frequently had flat/burst suppression background on EEG analysis.
Multivariable Analyses
In the multivariable analyses, high SOFA score on the day of ECMO initiation and the minimum ECMO blood flow during the first 4 days of therapy were independently associated with the occurrence of cerebral desaturation (Table 3). Lower rSO2 values and at least one episode of ΔrSO2 > 10% were independently associated with the development of ACC (Table 3). The optimum cutoff for the lowest rSO2 value to predict ACC was 52% (with a sensitivity of 71% and a specificity of 72%—Fig. 4). Higher lactate concentration during the first 4 days of ECMO support and the occurrence of cerebral desaturation were independently associated with hospital mortality (Table 3).
Discussion
This is the first study in which the role of rSO2 in adult patients undergoing VA-ECMO has been investigated; in this selected patient population, 32% of the patients developed ACC and the overall ICU mortality was 64%. ACC was more frequent in patients with the lowest rSO2 values or a large right–left rSO2 difference during NIRS monitoring. Cerebral desaturation occurred frequently in these patients, in particular in those with the highest severity score at the moment of ECMO implantation or in those who required a higher ECMO blood flow. Finally, hospital mortality in these patients was independently associated with high lactate levels and the occurrence of cerebral desaturation.
The incidence of neurological complications during VA-ECMO treatment ranges from 7 to 50% in the literature depending on the definition of “neurologic injury” used in the different studies, including brain hypoperfusion, ischemic and/or hemorrhagic stroke, post-anoxic brain injury, and impaired cerebral autoregulation [16,17,18]. The incidence of ACC in the present study is consistent with the data reported in the literature, although our patients were a selected population who also underwent NIRS monitoring. The decision to use NIRS monitoring was perhaps biased toward those patients with expected brain injury (e.g., during ECPR) or who already had some neurological abnormalities. A prospective study including all VA-ECMO patients may provide more accurate data on the role of NIRS monitoring in the early diagnosis of neurological complications.
As VA-ECMO patients usually require sedation, clinical neurological examination is not always reliable and neurological monitoring is of paramount importance to detect and potentially limit neurological complications. Cerebral NIRS monitoring has been extensively used to estimate cerebral oxygenation during heart, aortic, and carotid surgery, during which use of protocols based on NIRS-derived parameters has been shown to reduce neurological complications, in particular cerebral ischemia [7,8,9, 19]. NIRS monitoring has also been described during ECMO in neonates and children, especially because clinical assessment is not easily feasible in this setting [20, 21]. In contrast, the relevance of NIRS monitoring in adult ECMO patients has not yet been validated. To our knowledge, there is only one study in which the role of rSO2 was investigated in ECMO. Wong et al. [10] studied 20 adult ECMO patients treated with veno-venous and veno-arterial procedures: Cerebral saturation was defined as a reduction in rSO2 to less than 40% or by more than 25% from the baseline values; as the device used in the study by Wong and colleagues does not provide a reliable cutoff rSO2 to define “normal” values, because of the fewer wavelengths and less precision than the device we used [22], it is difficult to compare these data with our findings. Nevertheless, cerebral desaturation occurred in all ECMO patients and interventions which were undertaken to resolve these abnormalities, succeeded in 16/20 patients (80%). Of the four patients who did not respond to these interventions, two with persistent bilaterally low rSO2 values had diffuse anoxic brain injury and the two others with persistent unilaterally low rSO2 values had large unilateral ischemic strokes. Interestingly, rSO2 monitoring is the most feasible and safe tool to monitor cerebral oxygenation in VA-ECMO patients, where the use of invasive monitoring (i.e., parenchymal oxygen pressure, PtiO2) has never been described before and could be associated with an increased risk of intracerebral complications, because these patients are frequently thrombopenic and require systemic anticoagulation to prevent circuit clotting.
In our study, low rSO2 and large right–left rSO2 differences were independently associated with the occurrence of ACC. These data highlight the importance of NIRS cerebral oxymetry in ECMO patients to identify patients at risk of developing such complications. Nevertheless, this technique has its limitations. As one example, complications occurring outside the frontal areas could not be detected, as shown in our patient with a stroke in the posterior circulation. Second, if a persistent unilateral decrease in rSO2 is detected, the importance of urgent brain imaging and potential neuroradiological interventions to diagnose and treat cerebrovascular complications is unknown [23]. Third, it is important to recognize the cause of a low rSO2. In our study, cerebral desaturation was predicted by the severity of organ dysfunction, as assessed by the SOFA score, and a high minimal ECMO blood flow, which may reflect attempts to provide a better oxygen supply to the brain by increasing the oxygenated blood injected into the patient. This intervention is typical in patients with differential hypoxia, which occurred in 15% of the patients who developed ACC; correction of hypoxia in the upper body is feasible and requires specific ECMO (i.e., increasing blood flow) or “systemic” (e.g., increasing blood oxygen content, reducing patient blood flow, placing outflow injection cannula in the internal jugular/superior vena cava or shift from peripheral to central configuration) interventions [6]. Nevertheless, cerebral desaturation may also reflect global brain hypoperfusion, as observed in diffuse post-anoxic brain injury, which will result in brain death for most patients.
Cerebral desaturation was an independent predictor of hospital mortality, together with higher lactate levels during the first 4 days of ECMO support. Lactate is a widely accepted marker of severity of illness in critically ill patients; in patients suffering from cardiac arrest (40% of our patient population), and high lactate levels have been shown to be independently associated with poor outcomes [24]. In a large population of ECPR patients, Jung et al. showed that baseline serum lactate was the strongest predictor of poor outcome [25]. For the first time, we have identified cerebral desaturation as an independent predictor of mortality in ECMO patients; whether this reflects underlying brain injury or potentially avoidable secondary brain damage due to systemic factors, such as hypotension or hypoxemia, is difficult to conclude from our data. However, the use of the rSO2 threshold to identify this “cerebral desaturation” could be of great value for patients who are sedated on VA-ECMO, as clinicians could try to optimize brain oxygenation using absolute NIRS findings.
The study has several limitations. First, the association of cerebral desaturation with poor outcome does not guarantee that a NIRS-guided protocol would improve outcome in VA-ECMO patients. Although clinicians were aware of rSO2 values, we could not retrospectively describe whether different treatment modalities had been successful in ameliorating rSO2 and revert the occurrence of cerebral desaturation. This would have better clarified whether rSO2 in this setting is a diagnostic tool with therapeutic implications or simply a prognostic tool. Moreover, since cerebral desaturation triggered some therapeutic interventions, it is possible that the worse neurological outcomes associated with low rSO2 could be due to these interventions rather than to the cause of desaturation. Importantly, norepinephrine (which is the first-choice vasopressor in our ICU to increase blood pressure) could simply increase rSO2 by increasing cardiac output (i.e., by a β-adrenergic effect or by the shift of the unstressed volume into the central circulation when cardiac output is preload dependent) and thus the extracranial component of the rSO2 measurement, without adding any benefits to cerebral perfusion [26]. Second, admission diagnosis and reasons for ECMO may be associated with different risks of neurological complications and cerebral desaturation; however, it was not possible to conduct a subgroup analysis because of the limited number of patients in this study. Third, NIRS monitoring has additional pitfalls, such as inter-individual rSO2 variability for the same cerebral oxygenation, because of variable venous and arterial blood contents in the frontal areas, or contamination from the extracranial circulation, which can influence the absolute rSO2 value by 7–15% [27]. Fourth, we did not monitor veno-venous ECMO patients, although these patients are also at risk of cerebral complications, in particular brain hypoperfusion following rapid CO2 correction after ECMO implementation [28]. In addition, we did not measure plasma-free hemoglobin (fHb) levels; in ECMO patients, elevated fHb may enable detection of pump dysfunction and clot formation, which are associated with an increased risk of organ dysfunction and systemic complications [29]. Finally, in the absence of a control group, we cannot conclude whether rSO2 monitoring would be effective in helping reduce neurological complications in VA-ECMO patients.
Conclusions
These preliminary data show that use of cerebral NIRS in patients undergoing VA-ECMO could provide some interesting information on brain function. The predictive value of persistent unilateral or bilateral decreases in rSO2 to identify patients with stroke or with poor outcome needs to be further validated.
References
Nasr DM, Rabinstein A. Neurologic complications of extracorporeal membrane oxygenation. J Clin Neurol. 2015;11(4):383–9.
Zangrillo A, Landoni G, Biondi-Zoccai G, et al. A meta-analysis of complications and mortality of extracorporeal membrane oxygenation. Crit Care Resusc. 2013;15(3):172–8.
Cheng R, Hachamovitch R, Kittleson M, et al. Complications of extracorporeal membrane oxygenation for treatment of cardiogenic shock and cardiac arrest: a meta-analysis of 1866 adult patients. Ann Thorac Surg. 2014;97:610–6.
Hervey-Jumper SL, Annich GM, Yancon AR, Garton HJ, Muraszko KM, Maher CO. Neurological complications of extracorporeal membrane oxygenation in children. J Neurosurg Pediatr. 2011;7:338–44.
Mehta A, Ibsen LM. Neurologic complications and neurodevelopmental outcome with extracorporeal life support. World J Crit Care Med. 2013;2:40–7.
Cove ME. Disrupting differential hypoxia in peripheral veno-arterial extracorporeal membrane oxygenation. Crit Care. 2015;19:280.
Fischer GW, Lin HM, Krol M, et al. Non-invasive cerebral oxygenation may predict outcome in patients undergoing aortic arch surgery. J Thorac Cardiovasc Surg. 2011;141:815–21.
Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesia I. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104:51–8.
Goldman S, Suter F, Ferdinand F, Trace C. Optimizing intraoperative cerebral oxygen delivery using non-invasive cerebral oxymetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum. 2004;7:E376–81.
Wong JK, Smith TN, Pitcher HT, Hirose H, Cavarocchi NC. Cerebral and lower limb near-infrared spectroscopy in adults on extracorporeal membrane oxygenation. Artif Organs. 2012;36:659–67.
Lamartine Monteiro M, Taccone FS, Depondt C, et al. The prognostic value of 48-h continuous EEG during therapeutic hypothermia after cardiac arrest. Neurocrit Care. 2016;24(2):153–62.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;7905:480–4.
Suzuki S, Takasaki S, Ozaki T, Kobayashi Y. A tissue oxygenation monitor using NIR spatially resolved spectroscopy. Proc SPIE. 1999;3597:592.
Ghosh A, Elwell C, Smith M. Cerebral near-infrared spectroscopy in adults: a work in progress. Anesth Analg. 2012;115(6):1373–83.
McLeod D, Ikeda K, Cheng C, Shaw A. Validation of the next generation FORE-SIGHT elite tissue oximeter for adult cerebral tissue oxygen saturation. Anesth Analg. 2013;116(SCA Suppl):1–182.
Mateen FJ, Muralidharan R, Shinohara RT, et al. Neurological injury in adults treated with extracorporeal membrane oxygenation. Arch Neurol. 2011;68:1543–9.
Lan C, Tsai PR, Chen YS, Ko WJ. Prognostic factors for adult patients receiving extracorporeal membrane oxygenation as mechanical circulatory support—a 14-year experience at a medical center. Artif Organs. 2010;34:E59–64.
Ko WJ, Lin CY, Chen RJ, et al. Extracorporeal membrane oxygenation support for adult postcardiotomy cardiogenic shock. Ann Thorac Surg. 2002;73:538–45.
Samra SK, Dy EA, Welch K, Dorje P, Zelenock GB, Stanley JC. Evaluation of a cerebral oximeter as a monitor of cerebral ischemia during carotid endarterectomy. Anesthesiology. 2000;93:964–70.
Papdemetriou MD, Tachtsidis I, Leung TS, Elliott MJ, Hoskote A, Elwell CE. Cerebral and peripheral tissue oxygenation in children supported on ECMO for cardio-respiratory failure. Adv Exp Med Biol. 2010;662:447–53.
Rais-Bahrami K, Rivera O, Short BL. Validation of a noninvasive neonatal optical cerebral oximeter in veno-venous ECMO patients with a cephalad catheter. J Perinatol. 2006;26:628–35.
Greenberg S, Murphy G, Shear T, Patel A, Simpson A, Szokol J, Avram MJ, Vender J. Extracranial contamination in the INVOS 5100C versus the FORE-SIGHT ELITE cerebral oximeter: a prospective observational crossover study in volunteers. Can J Anesth. 2016;63:24–30.
Maldonado Y, Singh S, Taylor MA. Cerebral near-infrared spectroscopy in perioperative management of left ventricular assist device and extracorporeal membrane oxygenation patients. Curr Opin Anaesthesiol. 2014;27(1):81–8.
Vincent JL, Quintairos E, Silva A, Couto L Jr, Taccone FS. The value of blood lactate kinetics in critically ill patients: a systematic review. Crit Care. 2016;20(1):257.
Jung C, Janssen K, Kaluza M, et al. Outcome predictors in cardiopulmonary resuscitation facilitated by extracorporeal membrane oxygenation. Clin Res Cardiol. 2016;105(3):196–205.
Toksvang LN, Plovsing RR, Petersen MW, Møller K, Berg RM. Poor agreement between transcranial Doppler and near-infrared spectroscopy-based estimates of cerebral blood flow changes in sepsis. Clin Physiol Funct Imaging. 2014;34:405–9.
Davie SN, Grocott HP. Impact of extracranial contamination on regional cerebral oxygen saturation: a comparison of three cerebral oximetry technologies. Anesthesiology. 2012;116(4):834–40.
Luyt CE, Bréchot N, Demondion P, et al. Brain injury during venovenous extracorporeal membrane oxygenation. Intensive Care Med. 2016;42(5):897–907.
Omar HR, Mirsaeidi M, Socias S, et al. Plasma free hemoglobin is an independent predictor of mortality among patients on extracorporeal membrane oxygenation support. PLoS ONE. 2015;10(4):e0124034.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare to have no conflict of interest for this study.
Rights and permissions
About this article
Cite this article
Pozzebon, S., Blandino Ortiz, A., Franchi, F. et al. Cerebral Near-Infrared Spectroscopy in Adult Patients Undergoing Veno-Arterial Extracorporeal Membrane Oxygenation. Neurocrit Care 29, 94–104 (2018). https://doi.org/10.1007/s12028-018-0512-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0512-1