Abstract
Background
To explore the effect of end of life and other palliative decision making scenarios on the mental health of family members of patients in the neuro-intensive care unit.
Methods
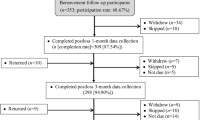
Decision makers of patients in the neuro-ICU at a large, urban, academic medical center meeting palliative care triggers were identified from November 10, 2014, to August 27, 2015. Interviews were conducted at 1 and 6 months post-enrollment. At 1 month, the Inventory of Complicated Grief-Revised (ICG-R), Impact of Events Scale-Revised (IES-R), and the Family Satisfaction-ICU (FS-ICU) were performed along with basic demographic questionnaires. At 6 months, only the ICG-R and IES-R were repeated.
Results
At 1 month, 9 (35%) subjects had significant symptoms in at least one of the three domains of traumatic response. Two (7.7%) subjects met full criteria for PTSD (IES-R ≥ 1.5). At 6 months, 5 (22%) subjects met criteria for PTSD and 5 (22%) for Complicated Grief (ICG-R ≥ 36). Fifteen (50%) had at least one domain of PTSD symptoms identified in follow-up. Time spent at bedside and lower household income were associated with PTSD at 1 and 6 months, respectively. In all, clinically significant psychological outcomes were identified in 9 (30%) of subjects.
Conclusions
Clinically significant grief and stress reactions were identified in 30% of decision makers for severely ill neuro-ICU patients. Though factors including time at bedside during hospitalization and total household income may have some predictive value for these disorders, further evaluation is required to help identify family members at risk of psychopathology following neuro-ICU admissions.

Similar content being viewed by others
References
Aslakson R, Cheng J, Vollenweider D, et al. Evidence-based palliative care in the intensive care unit: a systematic review of interventions. J Palliat Med. 2014;17(2):219–35.
Hua MS, Li G, Blinderman CD, et al. Estimates of the need for palliative care consultation across United States intensive care units using a trigger-based model. Am J Respir Crit Care Med. 2014;189(4):428–36.
Khandelwal N, Kross EK, Engelberg RA, et al. Estimating the effect of palliative care interventions and advance care planning on ICU utilization: a systematic review. Crit Care Med. 2015;43(5):1102–11.
Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356(5):469–78.
Carson SS, Cox CE, Wallenstein S, et al. Effect of palliative care—led meetings for families of patients with chronic critical illness: a randomized clinical trial. JAMA. 2016;316(1):51–62.
Frontera JA, Curtis JR, Nelson JE, et al. Integrating palliative care into the care of neurocritically ill patients: a report from the improving palliative care in the ICU project advisory board and the center to advance palliative care. Crit Care Med. 2015;43(9):1964–77.
Bernat JL. Ethical issues in the perioperative management of neurologic patients. Neurol Clin. 2004;22(2):457–71.
Burkle CM, Schipper AM, Wijdicks EF. Brain death and the courts. Neurology. 2011;76(9):837–41.
Anderson WG, Arnold RM, Angus DC, et al. Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med. 2008;23(11):1871–6.
Probst DR, Gustin JL, Goodman LF, et al. ICU versus Non-ICU hospital death: family member complicated grief, posttraumatic stress, and depressive symptoms. J Palliat Med. 2016;19(4):387–93.
Sundararajan K, Martin M, Rajagopala S, et al. Posttraumatic stress disorder in close relatives of intensive care unit patients’ evaluation (PRICE) study. Aust Crit Care. 2014;27:183.
Hwang DY, Yagoda D, Perrey HM, et al. Anxiety and depression symptoms among families of adult intensive care unit survivors immediately following brief length of stay. J Crit Care. 2014;29(2):278–82.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: American Psychiatric Association; 2000.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington: American Psychiatric Association; 2013.
Shear MK, Simon N, Wall M, et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety. 2011;28(2):103–17.
Weiss DS, Marmar CR. The impact of event scale—revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford Press; 1997. p. 399–411.
Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale-Revised. Behav Res Ther. 2003;41(12):1489–96.
Adkins JW, Weathers FW, Mcdevitt-murphy M, et al. Psychometric properties of seven self-report measures of posttraumatic stress disorder in college students with mixed civilian trauma exposure. J Anxiety Disord. 2008;22(8):1393–402.
Prigerson HG, Maciejewski PK, Reynolds CF, et al. Inventory of Complicated Grief: a scale to measure maladaptive symptoms of loss. Psychiatry Res. 1995;59(1–2):65–79.
O’connor M, Lasgaard M, Shevlin M, et al. A confirmatory factor analysis of combined models of the Harvard Trauma Questionnaire and the Inventory of Complicated Grief-Revised: are we measuring complicated grief or posttraumatic stress? J Anxiety Disord. 2010;24(7):672–9.
Golden AM, Dalgleish T. Is prolonged grief distinct from bereavement-related posttraumatic stress? Psychiatry Res. 2010;178(2):336–41.
Wall RJ, Engelberg RA, Downey L, et al. Refinement, scoring, and validation of the Family Satisfaction in the Intensive Care Unit (FS-ICU) survey. Crit Care Med. 2007;35(1):271–9.
Sarason IG, Sarason BR, Shearin EN, et al. A brief measure of social support: practical and theoretical implications. J Soc Pers Relationsh. 1987;4:497–510.
Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–14. doi:10.1016/0277-9536(91)90150-B.
Kersting A, Brähler E, Glaesmer H, Wagner B. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131(1–3):339–43.
Van Beusekom I, Bakhshi-raiez F, De Keizer NF, Dongelmans DA, Van der Schaaf M. Reported burden on informal caregivers of ICU survivors: a literature review. Crit Care. 2016;20:16.
Salins N, Deodhar J, Muckaden MA. Intensive Care Unit death and factors influencing family satisfaction of Intensive Care Unit care. Indian J Crit Care Med. 2016;20(2):97–103.
Kentish-barnes N, Seegers V, Legriel S, et al. CAESAR: a new tool to assess relatives’ experience of dying and death in the ICU. Intensive Care Med. 2016;42(6):995–1002.
Truog RD, Cist AF, Brackett SE, et al. Recommendations for end-of-life care in the intensive care unit: the Ethics Committee of the Society of Critical Care Medicine. Crit Care Med. 2001;29(12):2332–48.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have disclosed that they do not have any conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Trevick, S.A., Lord, A.S. Post-traumatic Stress Disorder and Complicated Grief are Common in Caregivers of Neuro-ICU Patients. Neurocrit Care 26, 436–443 (2017). https://doi.org/10.1007/s12028-016-0372-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0372-5