Abstract
Background
Anxiety and depression are common among patients with acute illness and their families. In oncology, psychosocial services addressing these symptoms are increasingly part of regular practice. Less is known about psychiatric distress among patients with acute neurological injury (ANI) and their family caregivers. To highlight this inequity in psychosocial intervention across medical services, we compared anxiety and depressive symptomatology shortly following diagnosis among patients facing incurable cancer or ANI and their family caregivers.
Methods
Recruited from the same hospital, participants were patients within 8 weeks of receiving a diagnosis of incurable cancer (N = 350) and their family caregivers (N = 275; total patient/caregiver dyads = 275) and patients hospitalized in the Neuroscience ICU in the past 2 weeks (N = 81) and their family caregivers (N = 95; total dyads = 75). Participants reported anxiety and depressive symptoms using the Hospital Anxiety and Depression Scale. Symptomatology was compared across illnesses using independent samples t-tests and multiple regressions controlling for differences in sample demographics.
Results
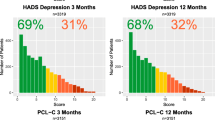
Patients with ANI (M = 6.90) reported greater anxiety symptoms than those with cancer (M = 5.31, p < .001), while caregivers for patients with ANI (M = 5.45) reported greater depressive symptoms than caregivers for patients with cancer (M = 3.81, p < .001). Results remained when controlling for demographic differences between samples.
Conclusion
This is the first cross-comparison of psychiatric distress in patients and family caregivers affected by two distinct, life-threatening illnesses early in the illness trajectory. Findings support the priority of addressing psychiatric distress among patients with ANI and their family caregivers, as has been emphasized in the psychosocial oncology field.
Similar content being viewed by others
References
Stark D, Kiely M, Smith A, Velikova G, House A, Selby P. Anxiety disorders in cancer patients: their nature, associations, and relation to quality of life. J Clin Oncol. 2002;20(14):3137–48.
Delgado-Guay M, Parsons HA, Li Z, Palmer JL, Bruera E. Symptom distress in advanced cancer patients with anxiety and depression in the palliative care setting. Support Care Cancer. 2009;17(5):573–9.
Cumming TB, Blomstrand C, Skoog I, Linden T. The high prevalence of anxiety disorders after stroke. Am J Geriatr Psychiatry. 2016;24(2):154–60.
Turner-Stokes L, Hassan N. Depression after stroke: a review of the evidence base to inform the development of an integrated care pathway. Part 1: diagnosis, frequency and impact. Clin Rehabil. 2002;16(3):231–47.
Campbell Burton CA, Murray J, Holmes J, Astin F, Greenwood D, Knapp P. Frequency of anxiety after stroke: a systematic review and meta-analysis of observational studies. Int J Stroke. 2013;8(7):545–59.
Pinquart M, Duberstein PR. Depression and cancer mortality: a meta-analysis. Psychol Med. 2010;40(11):1797–810.
Ayerbe L, Ayis S, Wolfe CDA, Rudd AG. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br J Psychiatry. 2013;202(1):14–21.
Bartoli F, Lillia N, Lax A, et al. Depression after stroke and risk of mortality: a systematic review and meta-analysis. Stroke Res Treat. 2013;2013:862978.
Greer JA, Pirl WF, Park ER, Lynch TJ, Temel JS. Behavioral and psychological predictors of chemotherapy adherence in patients with advanced non-small cell lung cancer. J Psychosom Res. 2008;65(6):549–52.
Lam WWT, Shing YT, Bonanno GA, Mancini AD, Fielding R. Distress trajectories at the first year diagnosis of breast cancer in relation to 6 years survivorship. Psychooncology. 2012;21(1):90–9.
Traeger L, Greer JA, Fernandez-Robles C, Temel JS, Pirl WF. Evidence-based treatment of anxiety in patients with cancer. J Clin Oncol. 2012;30(11):1197–205.
Li M, Fitzgerald P, Rodin G. Evidence-based treatment of depression in patients with cancer. J Clin Oncol. 2012;30(11):1187–96.
Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. Hidden morbidity in cancer: spouse caregivers. J Clin Oncol. 2007;25(30):4829–34.
Beach SR, Schulz R, Williamson GM, Miller LS, Weiner MF, Lance CE. Risk factors for potentially harmful informal caregiver behavior. J Am Geriatr Soc. 2005;53(2):255–61.
Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol Bull. 2003;129(6):946–72.
Ji J, Zöller B, Sundquist K, Sundquist J. Increased risks of coronary heart disease and stroke among spousal caregivers of cancer patients. Circulation. 2012;125(14):1742–7.
Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282(23):2215–9.
Duncan PW, Zorowitz R, Bates B, et al. Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke J Cereb Circ. 2005;36(9):e100–43.
Kent EE, Rowland JH, Northouse L, et al. Caring for caregivers and patients: research and clinical priorities for informal cancer caregiving. Cancer. 2016;122(13):1987–95.
Institute of Medicine (US) Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington (DC): National Academies Press (US); 2008 [cited 2016 June 22]. http://www.ncbi.nlm.nih.gov/books/NBK4015/.
Jacobsen PB, Wagner LI. A new quality standard: the integration of psychosocial care into routine cancer care. J Clin Oncol. 2012;30(11):1154–9.
American College of Surgeons. Commission on Cancer. Cancer program standards 2012: ensuring patient-centered care. American College of Surgeons; 2011.
Loscalzo M, Clark K, Pal S, Pirl WF. Role of biopsychosocial screening in cancer care. Cancer J Sudbury Mass. 2013;19(5):414–20.
Mitchell AJ. Screening for cancer-related distress: when is implementation successful and when is it unsuccessful? Acta Oncol Stockh Swed. 2013;52(2):216–24.
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–42.
Shaffer KM, Riklin E, Jacobs JM, Rosand J, Vranceanu A-M. Psychosocial resiliency is associated with lower emotional distress among dyads of patients and their informal caregivers in the neuroscience intensive care unit. J Crit Care. 2016;36:154–9.
Shaffer KM, Riklin E, Jacobs JM, Rosand J, Vranceanu A-M. Mindfulness and coping are inversely related to psychiatric symptoms in patients and informal caregivers in the neuroscience ICU: implications for clinical care. Crit Care Med. 2016;44(11):2028–36.
Hwang DY, Yagoda D, Perrey HM, et al. Anxiety and depression symptoms among families of adult intensive care unit survivors immediately following brief length of stay. J Crit Care. 2014;29(2):278–82.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70.
Cohen J. A power primer. Psychol Bull. 1992;112(1):155–9.
Statistical package for the social sciences. Armonk. NY: IBM Corporation; 2011.
Holland JC. History of psycho-oncology: overcoming attitudinal and conceptual barriers. Psychosom Med. 2002;64(2):206–21.
Northouse LL, Mood DW, Schafenacker A, et al. Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psychooncology. 2013;22(3):555–63.
Aben I, Verhey F, Lousberg R, Lodder J, Honig A. Validity of the beck depression inventory, hospital anxiety and depression scale, SCL-90, and hamilton depression rating scale as screening instruments for depression in stroke patients. Psychosomatics. 2002;43(5):386–93.
Vodermaier A, Millman RD. Accuracy of the Hospital Anxiety and Depression Scale as a screening tool in cancer patients: a systematic review and meta-analysis. Support Care Cancer. 2011;19(12):1899–908.
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77.
Acknowledgements
This work was performed at the Massachusetts General Hospital, Boston, MA. We thank Tara Tehan, Mary Guanci, Eric Riklin, and the nursing staff within the Neuroscience ICU for their help with recruitment for patients with Acute Neurological Injury. We thank the Cancer Outcomes Research team for their contributions to the Early Palliative Care study.
Funding
Dr. Vranceanu received support from the National Institute of Neurological Disorders and Stroke Clinical Trials Methodology Course (5R25NS088248-02). Dr. Temel received support from the National Institute of Nursing Research (R01 NR012735) and National Cancer Institute (K24 CA181253).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Shaffer, K.M., Jacobs, J.M., Coleman, J.N. et al. Anxiety and Depressive Symptoms Among Two Seriously Medically Ill Populations and Their Family Caregivers: A Comparison and Clinical Implications. Neurocrit Care 27, 180–186 (2017). https://doi.org/10.1007/s12028-016-0358-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0358-3