Abstract
Arterial gas embolism following pulmonary barotrauma occurs in 13–24% of cases of diving deaths. The study aimed to evaluate the usefulness of a histomorphometric digital analysis in the detection of air space over-distension due to pulmonary barotrauma. The study was performed on lung parenchyma specimens of 12 divers: six had died due to arterial gas embolism following pulmonary barotrauma (mean age at death of 54 years, range of 41–61 years), and six had drowned in saltwater without a diagnosis of pulmonary barotrauma (mean age at death of 54 years, range of 41–66 years) (positive controls). For negative controls, six cases of non-SCUBA divers (mean age of death of 42 years, range of 23–55 years) who died of intracerebral haemorrhage were evaluated. No significant differences were observed in the characteristics of the air spaces between control groups (positive and negative). However, differences were observed in the area occupied by air spaces and the percentage of air space area when we compared the case group to the controls (p < 0.01); and there was a slight difference in the maximum and minimum diameters of air space (p < 0.05). The mean area occupied by air spaces and the mean percentage of air space were the most useful for discriminating pulmonary barotrauma from other causes of death (100% sensitivity and 91.7% specificity). Based on our study, inclusion of an increased pattern of air spaces as a possible diagnostic criterion for pulmonary barotrauma would be useful in discerning the cause of diving death.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Self-contained underwater breathing apparatus (SCUBA) diving is one of the most popular and practised underwater activities [1, 2], and although it is overall a safe activity [3, 4], diving accidents can be potentially serious and even fatal [1, 5]. Decompression illness (DCI) is caused by intravascular or extravascular bubbles that are formed as a result of a reduction in environmental pressure [6]. The term covers both decompression sickness (DCS) and arterial gas embolism (AGE) [7], and while DCS is caused by evolution of bubbles from dissolved inert gas, AGE is caused by introduction of air into the systemic circulation by pulmonary barotrauma (PBt) [8,9,10]. Currently, different terms have been used to refer to a PBt. These include pulmonary overexpansion injury, pulmonary over-inflation syndrome, extra-alveolar air syndrome and intrathoracic hypopressive syndrome [9, 11,12,13]. However, each of these diagnoses has different clinical manifestations such as subcutaneous emphysema, pneumomediastinum, pneumothorax, pneumoperitoneum or AGE, including the death of the diver within minutes [8, 9, 14,15,16].
Although drowning is the main cause of death, arterial gas embolism following pulmonary barotrauma (PBt/AGE) during exposure to reduced environmental pressure (PBt of ascent) has been described in 13–24% of cases [17, 18], and this is well documented in diving medical texts [2, 9, 19,20,21]. According to Boyle’s law, when a SCUBA diver ascends to the surface too quickly without exhaling appropriately, the gas retained in their lungs increases the intrapulmonary pressure while external pressure decreases rapidly [12, 14, 15, 22, 23]. In an emergency situation, panic worsens the diver’s breathing and sometimes can close the glottis completely. Laryngospasm, bronchoconstriction (if water is inspired) or asthmatic bronchospasm has also been described as potential causes that might prevent air exhalation [12]. In addition, other findings such as mucous plugs or foreign bodies may make airflow difficult, even expert divers. This breathing gas remains inside the lungs at a pressure higher than the environmental pressure, converting the thoracic cavity into a pressure container [14]. This increase in intrapulmonary lung tension results in a pulmonary histopathological pattern characterized by over-distension of the air spaces (AS) distal to the terminal bronchiole and this leads to bronchoalveolar emphysema with rupture of the alveolar air sacs. Therefore, gas is then introduced into the blood vessels which are no longer intact [8, 9, 13, 24]. Currently, it is agreed that alveolar tears could provide the avenue for entrance of air into the stroma of the lung. This air develops an interstitial emphysema within a perivascular sheath [8, 13, 25] defined as cystic spaces inside the lung interstitial tissues [26], and allows air to escape into the pulmonary venous system, thereby accessing the left side of the heart [8, 13, 17, 18]. If air bubbles reach the cerebral arterial circulation, they can interrupt blood flow to the brain, and cause AGE with ischemic injuries such as brain anoxia or even death [27].
In order to establish a PBt/AGE post-mortem diagnosis, it is essential to know the deceased person’s dive profile, to use specific autopsy techniques and/or image diagnoses, to obtain various toxicological and histopathological studies and to know their medical record [2, 22,23,24, 28,29,30,31,32,33,34]. This diagnosis is met when the following four major criteria are met [17, 18]: history of rapid ascent followed by loss of consciousness; air in the left side of the heart and circle of Willis; low probability of post-mortem decompression artefact (PMDA) or decomposition; and mediastinal or subcutaneous emphysema limited to the perithoracic area and/or pneumothorax.
Studies describing some of the tissue lesions characteristic of PBt are scarce and based on the use of classical histological techniques [12, 17, 18, 22,23,24, 28, 34]. Other studies have used experimental models that induce PBt in animals, commonly rabbits, in hyperbaric chambers [35]. Recently, a histomorphometric analysis of pulmonary tissue has been proposed as a technique for providing objective data on alveolar distension in cases of asphyxia in humans [36, 37]. However, to date, there are no studies using quantitative techniques to investigate the presence of air in the lungs in cases of PBt.
Based on the PBt physiopathology, the aim of this study was demonstrate and quantify the presence of abnormal AS in pulmonary tissues by histomorphometric digital analysis in order to verify whether they can be used for the differential diagnosis in SCUBA diving fatalities.
Materials and methods
The study was developed in collaboration with the Institute of Legal Medicine and Forensic Sciences of Catalonia (ILMFSC), the Department of Medical Sciences of the University of Girona, and the Special Group for Underwater Activities of the Spanish Civil Guard. It was authorized on September 20, 2018 by the Teaching and Research Commission of ILMFSC and the Research Ethical Committee of Bellvitge University Hospital, Barcelona (Registry number PR328/18).
Data sources
Our sources of information included data obtained from police technical reports and the forensic pathology service. All victims were diving for recreational purpose and were dependent on gas supply: eleven divers used cylinders containing compressed air as their sole gas supply, and only one diver used an additional supply of Trimix (a mixture of nitrogen, oxygen and helium) in separate cylinders. A detailed summary of the main subject, technical characteristics and sequence of events of all cases is shown in Tables 1 and 2, respectively.
Lung ample from SCUBA diving fatalities
This study includes twelve cases of diving deaths recorded on the Mediterranean Sea (Girona coast, Northeast of Spain) between January 2009 and January 2020. Post-mortem, the bodies were immediately refrigerated at 5–6 °C. All the lung samples were obtained from autopsies conducted at the Forensic Pathology Service of ILMFSC, with a post-mortem interval (PMI) of less than 30 h, and by forensic pathologists with experience in diving fatalities.
We studied lung parenchyma samples from a histological point of view corresponding to six divers (mean age at death of 54 years, range of 41–61 years) where PBt/AGE was diagnosed as the cause of death according to the protocols and specific recommendations for this type of death [2, 17, 18, 22, 23, 29]. In order to compare these results with the histological pattern that can be found in other types of SCUBA diving-related fatalities and as positive controls, we selected six divers (mean age of death of 54 years, range of 41–66 years) whose death was due to drowning in saltwater and without a diagnosis PBt/AGE. The negative control group included six cases of non-SCUBA divers (mean age at death of 42 years, range of 23–55 years) whose cause of death was intracerebral haemorrhage in which a low probability of lung distension was expected.
Exclusion criteria for this study were included age over 65 years; PMI longer than 30 h; use of high-pressure oxygen in cardiopulmonary resuscitation (CPR) advanced manoeuvers; admission to the intensive care unit of a medical centre; and pneumological diseases showing chronic pulmonary emphysema according to medical records and standard histological results. These exclusion criteria were established in accordance with different studies published describing the presence of air secondary to age (senile lung emphysema), decomposition, CPR advanced manoeuvers and pre-existing pathologies [24, 33, 38].
Routine histology
During the autopsies, randomly chosen samples from different lobes of the lung in non-hypostatic central and peripheral areas were taken and placed in 10% formalin. The paraffin-embedded lung samples were cut into 5-µm sections and stained with haematoxylin and eosin (HE) for routine histological examination by our Forensic Pathology Service.
Image analysis
After routine histological analysis, we reassessed these samples by direct optical microscopy Leica DMRXA and selected seventy-two slides. Six microscope fields were randomly selected (10 × magnification) for each slide, and a total of 432 fields are photographed with a Point Grey Flea3 CMOS USB3.0 digital camera with 12MPx coupled with optical microscopy.
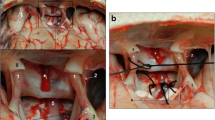
Digital photographs were analysed using open-source image analysis software (FIJI ImageJ2, National Institutes of Health). This software can easily and carefully detect AS in each field by specific Image J Macro (for segmentation and posterior measurement, an adaptive threshold was applied, based on levels of red, on the parenchymal component of each image, with automatic posterior binarization). We defined an AS as an air collection, located in an intra-alveolar or extra-alveolar space and with a minimum area of 100 µm2 (Fig. 1). All AS present in each sample were identified, including those that were incomplete at the edges of the field. Conversely, the presence of oedema, blood vessels or intra-alveolar cells was automatically excluded and not identified, but in some cases, the AS had to be manually selected in order to exclude artefacts (Fig. 2).
Image corresponding to lung tissue (HE, 10 ×) (A) and its digital analysis by the specific Image J Macro used (B, C). The image shows segmentation process where air spaces (AS) are accurately defined (yellow line) (B). It shows the binarization process of the previous image where AS are identified as black areas (C)
Image corresponding to lung tissue (HE, 10 ×) (A) and its digital analysis by the specific Image J Macro used (B, C, D). In this case, we show a wrong segmentation defined by the yellow line (B), its manual adjustment in order to well define the air spaces (C) and the binarization process of the correct segmentation (D)
The following parameters were measured for each field: count of AS (CAS); total area occupied by AS (AAS); percentage (%) of the field occupied by the AS compared to the rest of the parenchyma (PAS); and maximum diameter (MaxDAS) and minimum diameter (MinDAS) of each air collection. Finally, these parameters were automatically calculated and exported to a MS Excel table.
Statistical analysis
Normality and equality of variance were observed using the Shapiro–Wilk and Levene tests. ANOVA test and post hoc analysis were performed to compare means between groups. Receiver operating characteristic (ROC) curve analysis was performed to establish a cut-off value to evaluate the sensitivity and specificity of different parameters. SPSS software (v25.0, IBM, Armonk, NY) was used for the statistical analysis.
Results
A brief summary of histological results from all cases is shown in Table 3.
Morphometric analysis
The ANOVA test and post hoc analysis results are summarized in Table 4. No significant differences were observed in AS characteristics between the saltwater drownings group and the intracerebral haemorrhage group. Differences were observed in the mean area of AS (AAS), mean area ratio for count of AS (AAS/CAS) and in percentage of AS (PAS) for each field compared to the rest of the parenchyma (p < 0.01) between the PBt/AGE and the drownings groups (Fig. 3). There was a slight difference in AS maximum and minimum diameters (maximum DAS and minimum DAS) (p < 0.05) between the PBt/AGE and drownings groups.
ROC curve analysis was performed between PBt/AGE and the other two groups (Table 5 and Fig. 4). The mean AAS and mean PAS were best (AUC of 0.944) for discriminating PBt/AGE from the others with a 100% sensitivity and 91.7% specificity for every cut-off value.
Discussion
PBt/AGE is one of the most serious diving accidents that can occur during SCUBA diving ascent if the breath is held and retained inside the lungs while environmental pressure is reduced. Some authorities describe or refer to this as parenchymal haemorrhage, segmental or lobe rupture and even lung bursts [9, 14, 39]. In our series of autopsies, only one case of alveolar haemorrhage was identified. This can possibly be explained by the Macklin effect [40,41,42,43] as the breathing gas excess looks for a natural pathway exit while maintaining certain anatomical integrity due to the fact that the air accesses extra-pulmonary areas located in the subcutaneous tissues, pleural cavity, mediastinum, peritoneum and even the retroperitoneum via the perivascular sheaths of the lung.
Our results also show that none of the analysed histological parameters allowed us to distinguish between saltwater drownings and controls. Although some pathological changes have been described in drowning as emphysematous-like alveolar patterns or “emphysema aquosum” [12, 44, 45], other authors believe that there are no specific histological changes [23, 46]. Recent studies suggest that acute pulmonary emphysema is not a typical sign of death by saltwater drowning [37]. Conversely, in the PBt/AGE group, our results show an emphysematous pattern that is different from the other analysed groups and congruent with bronchoalveolar emphysema. Morphologically, we observed that AS occupy a larger area of distribution, even overlapping each other, and with an over-distension that is both intra- and extra-alveolar. These results demonstrate the presence of a significantly larger AS in the pulmonary parenchyma of divers that died within a context of a PBt/AGE. We believe that this might be related to the intrapulmonary high-pressure air retention. These results differ from the histology we found in cases of death by drowning and the control group.
Autopsy evidence from cases of fatal PBt/AGE needs to be interpreted with caution [24] because the macro- or microscopic findings may not be definitively attributed to gas formation as a result of the reduction in environment pressure [46]. Admittedly, the presence of intravascular air is not uncommon in autopsies of SCUBA diving deaths, and it is not specific to PBt/AGE [2, 17, 18]; it can also be due to explosive DCS, post-mortem decompression artefact (PMDA), decomposition and/or resuscitation. It is important to distinguish AGE from DCS, although they can occasionally occur simultaneously [11]. In all SCUBA divers studied herein, we were able to remove DCS as a diagnosis because these divers did not stay under water long enough or go deep enough to develop this dysbaric disorder. Therefore, we believe that PMDA, as documented in the police report, is improbable. In addition, performing autopsies with a PMI of less than 30 h avoided the artefacts of putrefaction or decomposition in our study. Even so, some authorities differentiate between in vivo gas embolism and putrefaction by using gas composition analysis [47], which is a good alternative to avoid the artefact of putrefaction as long as the necessary technical resources are available. Similarly, although resuscitation efforts secondary-to-CPR manoeuvers may rarely simulate larger volumes usually seen with PBt [2, 17, 18], well-controlled animal experiments suggest that in fatal SCUBA diving accidents, subcutaneous emphysema should not be mistaken as diagnostic criteria for barotrauma, because it may be an artefact caused by the resuscitation manoeuvers [30].
Together with a history of rapid ascent as registered in the dive profile, the presence of air in the systemic circulation is one of the key criteria for diagnosing PBt/AGE [17, 18, 29]. Although some studies have described technical modifications that demonstrate this in various organs at autopsy [33], the use of post-mortem imaging techniques should be used when available. Unfortunately, these radiological and macroscopic techniques may not be conclusive to show air existence because most autopsies are performed by pathologists who are not familiar with diving-related injuries. All of this justifies the need to use supplementary analyses to help confirm the radiological and macroscopic findings and differentiate PBt/AGE from other pathologies characteristic of diving, particularly drowning. This is especially important for the medical examiner or coroner’s office, as most diving-related deaths will undergo autopsies at these facilities and not at a large university hospital pathology department.
In addition, a careful histological examination is required for distinguishing these from positive pressure ventilation; pre-existing disease such as chronic pulmonary emphysema; and death due to cardiac oedema, acute asthma or intoxications [48, 49]. In particular, and although in all our cases toxicological analyses were negative, one should remember that inhalational drug abuse (cocaine) and inhalation of certain gases can also cause PBt [50, 51] and, thus, results in a misinterpretation of histopathological findings.
Conclusions
Our findings suggest a direct association between PBt and over-distension of AS in pulmonary tissues that can be shown with histomorphometric digital analysis. This study found that an increased histopathological pattern of AS, congruent which an bronchoalveolar emphysema, is a possible major diagnostic criterion for PBt/AGE, including a detailed dive profile, and the radiological and/or macroscopic findings described by Lawrence and Cooke [17, 18]. All of this will provide insights for investigation of fatal SCUBA diving incidents.
Limitations and perspectives
The heterogeneous distribution pattern of AS described in emphysematous lungs makes it difficult to find strong evidence for a pathognomonic diagnosis. Therefore, a multidisciplinary investigation including the deceased person’s dive profile, specific autopsy techniques and/or post-mortem radiographic imaging must be performed. The histological findings described herein should be with future additional cases and one must consider that pulmonary barotrauma in SCUBA diving fatalities is, in general, uncommon.
Key points
-
1.
Despite drowning being the most common cause of death, a differential diagnosis is mandatory.
-
2.
A qualified investigation of diving fatalities requires a careful histological examination.
-
3.
Alveolar tears provide a pathway for the entrance of air into the stroma resulting in interstitial emphysema.
-
4.
Histomorphometric analysis allows one to diagnose pulmonary barotrauma with over-distension of the air spaces.
References
Ihama Y, Miyazaki T, Fuke C, Mukai T, Ohno Y, Sato Y. Scuba-diving related deaths in Okinawa, Japan, from 1982 to 2007. Leg Med (Tokyo). 2008;10:119–24.
Edmonds C, Caruso J. Recent modifications to the investigation of diving related deaths. Forensic Sci Med Pathol. 2014;10:83–90.
Desola J. Sudden death of non-cardiological origin during exercise. The dysbarism model. Med Clin (Barc). 2017;148:566–8.
Shreeves K, Buzzacott P, Hornsby A, Caney M. Violations of safe diving practices among 122 diver fatalities. Int Marit Health. 2018;69:94–8.
Smith N. Scuba diving: how high the risk? J Insur Med. 1995;27:15–24.
Francis TJR, Smith DJ, Eds. Describing decompression illness. 42nd Workshop of the Undersea and Hyperbaric Medical Society. Bethesda, MD: Undersea and Hyperbaric Medical Society. 1991.
Vann RD, Butler FK, Mitchell SJ, Moon RE. Decompression illness. Lancet. 2011;377:153–64.
Francis J. Pulmonary barotrauma: a new look at mechanisms. SPUMS J. 1997;27:205–18.
Caruso JL. The pathology of drowning and pulmonary overexpansion injury. Acad Forensic Pathol. 2013;3(4):435–45.
Mitchell SJ. DCS or DCI? The difference and why it matters. Diving Hyperb Med. 2019;49(3):152–3.
Desola J, Sala J. The combination of decompression-sickness plus intrathoracic hyperpressive syndrome plus and near drowning (“The diving tragedy”) – reflections and concerns. In: Desola J, editor. Proceeding of the 15th International Congress on Hyperbaric Medicine. Barcelona, Sub-Help, cop. 2005;181–7.
Shkrum MJ, Ramsay DA. Forensic pathology of trauma: common problems for the pathologist. Totowa, NJ: Humana Press Inc. 1st ed. 5.14, Bodies recovered from water: diving-related deaths. 2007;278–93.
U.S. Navy Diving Manual. Rev 7. Washington, DC: Naval Sea Systems Command. 3.8, Pulmonary overinflation syndromes. 2018;32–40.
Desola J. Accidentes de buceo (2). Barotraumatismo respiratorio: Síndrome de sobrepresión pulmonar. Med Clin (Barc). 1990;95:183–90.
Ehm OF. Pulmonary barotrauma: reflections on its causes. European J Underwater Hyperbaric Med. 2001;2(1):4–7.
Bunni J, Bryson PJ, Higgs SM. Abdominal compartment syndrome caused by tension pneumoperitoneum in a scuba diver. Ann R Coll Surg Engl. 2012;94:237–9.
Lawrence C, Cooke C. Autopsy and the investigation of scuba diving fatalities. Melbourne: The Royal College of Pathologists of Australasia. 2003. Available from: http://www.rcpa.edu.au/Library/College-Policies. Accessed August 2013
Lawrence C, Cooke C. Autopsy and the investigation of scuba diving fatalities. Diving Hyperb Med. 2006;36:2–8.
Denoble PJ, Caruso JL, Dear G de L, Pieper CF, Vann RD. Common causes of open-circuit recreational diving fatalities. Undersea Hyperb Med. 2008;35:393–406.26
Edmonds C, Bennett M, Lippmann J, Mitchell S. Diving and subaquatic medicine: CRC Press. 5th ed. 6, Pulmonary barotrauma. 2016;65–79.
Casadesús JM, Aguirre F, Carrera A, Boadas-Vaello P, Serrando MT, Reina F. Diving-related fatalities: multidisciplinary, experience-based investigation. Forensic Sci Med Pathol. 2019;15:224–32.
Busuttil A, Obafunwa J. A review of the forensic investigation of scuba diving deaths. Sci Justice. 1995;35:87–95.
Saukko P, Knight B. Knight’s forensic pathology: CRC Press. 4th ed. 24, Dysbaric fatalities and barotrauma. 2015;509–13.
Calder IM. Autopsy and experimental observations on factors leading to barotrauma in man. Undersea Biomed Res. 1985;12(1):165–82.
Schaffer KE, McNulty WO, Carey C, Liebow AA. Mechanisms in development of interstitial emphysema and air embolism on decompression from depth. J Appl Physiol. 1958;13(1):15–29.
Barcia SM, Kukreja J, Jones KD. Pulmonary interstitial emphysema in adults: a clinicopathologic study of 53 lungs explants. Am J Surg Pathol. 2014;38(3):339–45.
Neumann TS, Jacoby I, Bove AA. Fatal pulmonary barotrauma due to obstruction of the central circulation with air. J Emeg Med. 1998;16:413–7.
Wheen LC, Williams MP. Post-mortems in recreational scuba diver deaths: The utility of radiology. J Forensic Legal Med. 2009;16:273–6.
Caruso JL. Appendix F: Autopsy protocol for recreational scuba diving fatality. In: Vann RD, Lang MA, editors. Recreational diving fatalities workshop proceedings. Durham: Divers Alert Network. 2011;277–9.
Laurent PE, Coulange M, Bartoli C, et al. Appearance of gas collections after scuba diving death: a computed tomography study in a porcine model. Int J Legal Med. 2013;127:177–84.
Robert G, Teather CV. Encyclopedia of underwater investigations: Best Publishing Company. 2nd ed. 7, Scuba fatality-accident investigation. 2013;190–237.
Edmonds C, Bennett M, Lippmann J, Mitchell S. Diving and subaquatic medicine: CRC Press. 5th ed. 51, Investigations of diving fatalities. 2016;583–600.
Casadesús JM, Aguirre F, Carrera A, Boadas-Vaello P, Serrando MT, Reina F. Diagnosis of arterial gas embolism in SCUBA diving: modification suggestion of autopsy techniques and experience in eight cases. Forensic Sci Med Pathol. 2018;14:18–25.
Aquila I, Pepe F, Manno M, Frati P, Gratteri S, Fineschi V, et al. Scuba diving death: always due to drowning? Two forensic cases and a review of the literature. Med Leg J. 2018;86:49–51.
Siermontowski P, Kozlowski W, Pedrycz A, Krefft K, Kaczerska D. Experimental modeling of pulmonary barotrauma. Undersea Hiperb Med. 2015;42(2):143–9.
Castiglioni C, Baumann P, Fracasso T. Acute pulomary emphysema in death by hanging: a morphometric digital study. Int J Legal Med. 2016;130(5):1281–5.
Barranco R, Castiglioni C, Ventura F, Fracasso T. A comparative digital morphometric study of lung tissue in saltwater and freshwater drowning. Forensic Sci Int. 2019;298:157–60.
Kohlhase C, Maxeiner H. Morphometric investigation of emphysema aquosum in the elderly. Forensic Sci Int. 2003;134(2–3):93–8.
Tsai MJ, Tsai MS, Tsai YM, Lien CT, Hwang JJ, Huang MS. Alveolar hemorrhage after scuba diving: a case report. Kaohsiung J Med Sci. 2010;26(7):389–92.
Macklin CC. Pneumotorax with massive collapse from experimental local over-inflation of the lung substance. Can Med Assoc J. 1937;36(4):414–20.
Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiment. Medicine. 1944;23:281–358.
Seung-Tak O, Wook K, Hae-Myung J, Jeong-Soo K, Kee-Whan K, Seung-Jin Y, Eung-Kuk K. Massive pneumoperitoneum after scuba diving. J Korean Med Sci. 2003;18:281–3.
Marsico S, Del Carpio Bellido LA, Zuccarino F. Spontaneous pneumomediastinum and macklin effect in COVID-19 patients. Arch Bronconeumol. 2021;57(1):67.
Fornes P, Pepin G, Heudes H, Lecomte D. Diagnosis of drowning by combined computer-assisted histomorphometry of lungs with blood strontium determination. J Forensic Sci. 1998;43:772–6.
Delmonte C, Capelozzi VL. Morphologic determinants of asphyxia in lungs: a semiquantitative study in forensic autopsies. Am J Forensic Med Pathol. 2001;22(2):139–49.
Ball CG, Herath JC. Earth, air, water, and fire: histopathology of environmental death. Acad Forensic Pathol. 2018;8(3):641–52.
Varlet V, Dominguez A, Augsburger M, Lossois M, Egger C, Palmiere C, Vilarino R, Grabherr S. Understanding scuba diving fatalities: carbon dioxide concentrations in intra-cardiac gas. Diving Hyperb Med. 2017;47:75–81.
Shrestha DB, Sedhai YR, Budhathoki P, Adhikari A, Pokharel N, Dhakal R, Kafle S, Yadullahi Mir WA, Acharya R, Kashiouris MG, Parker MS. Pulmonary barotrauma in COVID-19: a systematic review and meta-analysis. Ann Med Surg (Lond). 2022;73:103221.
Mauad T, do Nascimento FB, Dolhnikoff M, Picka M, Saldiva PH. Pulmonary interstitial emphysema in fatal asthma: case report and histopathological review. BMC Pulm Med. 2018;18(1):50.
Underner M, Peiffer G, Perriot J, Jaafari N. Complications pulmonaires chez les consommateurs de cocaïne [Pulmonary complications in cocaine users]. Rev Mal Respir. 2020;37(1):45–59.
Smędra A, Łabętowicz P, Wochna K, Berent J. Helium suicide - a suffocation or a barotrauma? J Forensic Leg Med. 2020;76:102065.
Acknowledgements
We gratefully acknowledge the contribution of our colleagues (Aina Torres) and technical staff (Dani Reyes) of the University of Girona for their help in this project. The authors also thank i2e3 Biomedical Research Institute for editing the final version of the manuscript and Agency for Management of University and Research Grants-AGAUR, Generalitat of Catalonia, for your support (grant number 2017 SGR 1279).
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Josep M. Casadesús, Javier Nieto-Moragas, Anna Carrera, Pere Boadas-Vaello, Maria T. Serrando and Fernando Aguirre. The first draft of the manuscript was written by Francisco Reina and Josep M. Casadesús, and all authors commented on previous versions of the manuscript. Review and final edition were made by R. Shane Tubbs, Francisco Reina and Josep M. Casadesús. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was authorized on September 20, 2018, by the Teaching and Research Commission of ILMFSC and the Research Ethical Committee of Bellvitge University Hospital, Barcelona (registry number PR328/18).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Casadesús, J.M., Nieto-Moragas, J., Serrando, M.T. et al. Pulmonary barotrauma in SCUBA diving-related fatalities: a histological and histomorphometric analysis. Forensic Sci Med Pathol 19, 541–550 (2023). https://doi.org/10.1007/s12024-022-00567-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12024-022-00567-1