Abstract
Objective
Some observational studies have suggested the association between thyroid function and polycystic ovary syndrome (PCOS). However, it remains to be determined whether these associations are causal or not. The aim of this study was to investigate the underlying causal association between different thyroid function status and PCOS.
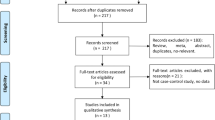
Methods
Bidirectional Mendelian randomization (MR) analysis was conducted to explore the impact of different thyroid function statuses on PCOS. The study included 10,074 individuals with PCOS and 103,164 controls for the primary analysis, with validation analysis repeated in the FinnGen R9 and EstBB PCOS cohorts. Female-specific thyroid function GWAS data were obtained from European population, including Hyperthyroidism (22,383 cases and 54,288 controls) and Hypothyroidism (27,383 cases and 54,288 controls) from the UK Biobank, and TSH (54,288 cases and 72,167 controls) and FT4 (49,269 cases and 72,167 controls) within the reference range from the ThyroidOmics Consortium. Inverse variance weighting (IVW) was chosen as the principal method, and sensitivity analysis was conducted to test for the presence of horizontal pleiotropy or heterogeneity.
Results
The IVW analysis indicated nominal significance between normal TSH levels and PCOS after adjusted for age and BMI [OR (95% CI) = 0.78(0.62,0.97), P = 0.029], suggesting that maintaining normal TSH levels might act as a protective factor against the pathogenesis of PCOS. Besides, in order to increase the statistical power, we pooled PCOS GWAS above together by meta-analysis and found PCOS contributed to the occurrence of hyperthyroidism [OR(95%CI) = 1.37(0.73,2.57), P = 0.012]. However, no causal relationship was found after Bonferroni correction (P-value < 0.0031).
Conclusion
Although the MR analysis didn’t indicate genetic causal association between thyroid function and PCOS after Bonferroni correction. Further efforts are needed to interpret the potential causal relationship between thyroid function and PCOS in different age and BMI subgroup.



Similar content being viewed by others
Data availability
Publicly available data were analyzed in this study, which can be found in: UK Biobank (https://www.nealelab.is/ukbiobank), ThyroidOmicsConsortium (http://www.thyroidomics.com), FinnGenR9 (https://www.finngen.fi/en/access_results) and GWAS Catalog (https://www.ebi.ac.uk/). The original contributions presented in the study are included in the Article/Suppletmentary Material, further inquiries can be directed to the corresponding author.
References
S. De Leo, S.Y. Lee, L.E. Braverman, Hyperthyroidism. Lancet Lond. Engl. 388(10047), 906–918 (2016). https://doi.org/10.1016/S0140-6736(16)00278-6
P. N. Taylor, D. Albrecht, A. Scholz, G. Gutierrez-Buey, J. H. Lazarus, C. M. Dayan, O. E. Okosieme, Global epidemiology of hyperthyroidism and hypothyroidism. Nature reviews. Endocrinology 14(5), 301–316 (2018). https://doi.org/10.1038/nrendo.2018.18
K. Poppe, P. Bisschop, L. Fugazzola, G. Minziori, D. Unuane, A. Weghofer, 2021 European Thyroid Association Guideline on Thyroid Disorders prior to and during Assisted Reproduction. Eur. Thyroid J. 9(6), 281–295 (2021). https://doi.org/10.1159/000512790
J.G. Hollowell, N.W. Staehling, W.D. Flanders et al. Serum TSH, T4, and Thyroid Antibodies in the United States Population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J. Clin. Endocrinol. Metab. 87(2), 489–499 (2002). https://doi.org/10.1210/jcem.87.2.8182
C. Dosiou, Thyroid and Fertility: Recent Advances. Thyroid J. Am. Thyroid Assoc. 30(4), 479–486 (2020). https://doi.org/10.1089/thy.2019.0382
K. Poppe, Management of Endocrine Disease: Thyroid and female infertility: more questions than answers?! Eur. J. Endocrinol. 184(4), R123–R135 (2021). https://doi.org/10.1530/EJE-20-1284
M.A. Bedaiwy, M.Y. Abdel-Rahman, J. Tan et al. Clinical, Hormonal, and Metabolic Parameters in Women with Subclinical Hypothyroidism and Polycystic Ovary Syndrome: A Cross-Sectional Study. J. Womens Health 27(5), 659–664 (2018). https://doi.org/10.1089/jwh.2017.6584
T.I.M. Korevaar, L. Mínguez-Alarcón, C. Messerlian et al. Association of Thyroid Function and Autoimmunity with Ovarian Reserve in Women Seeking Infertility Care. Thyroid J. Am. Thyroid Assoc. 28(10), 1349–1358 (2018). https://doi.org/10.1089/thy.2017.0582
H.M. Sadeghi, I. Adeli, D. Calina et al. Polycystic Ovary Syndrome: A Comprehensive Review of Pathogenesis, Management, and Drug Repurposing. Int J. Mol. Sci. 23(2), 583 (2022). https://doi.org/10.3390/ijms23020583
A.H. Balen, G.S. Conway, G. Kaltsas et al. Andrology: Polycystic ovary syndrome: the spectrum of the disorder in 1741 patients. Hum. Reprod. 10(8), 2107–2111 (1995). https://doi.org/10.1093/oxfordjournals.humrep.a136243
S. Parveen, S. Das, Homeopathic Treatment in Patients with Polycystic Ovarian Syndrome: A Case Series. Homeopath. J. Fac. Homeopath. 110(3), 186–193 (2021). https://doi.org/10.1055/s-0041-1725039
J. Puurunen, T. Piltonen, L. Morin-Papunen, A. Perheentupa, I. Järvelä, A. Ruokonen, J. S. Tapanainen, Unfavorable hormonal, metabolic, and inflammatory alterations persist after menopause in women with PCOS. J. Clin. Endocrinol. Metab. 96(6), 1827–1834 (2011). https://doi.org/10.1210/jc.2011-0039
J. Collée, M. Mawet, L. Tebache, M. Nisolle, G. Brichant, Polycystic ovarian syndrome and infertility: overview and insights of the putative treatmentsGynecological endocrinology: the official journal of the International Society of Gynecological Endocrinology, 37(10), 869–874 (2021). https://doi.org/10.1080/09513590.2021.1958310
H. Teede, A. Deeks, L. Moran, Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC medicine, 8, 41 (2010). https://doi.org/10.1186/1741-7015-8-41
I.M. Gawron, R. Baran, K. Derbisz, R. Jach, Association of Subclinical Hypothyroidism with Present and Absent Anti-Thyroid Antibodies with PCOS Phenotypes and Metabolic Profile. J. Clin. Med. 11(6), 1547 (2022). https://doi.org/10.3390/jcm11061547
A. Arduc, B. Aycicek Dogan, S. Bilmez et al. High prevalence of Hashimoto’s thyroiditis in patients with polycystic ovary syndrome: does the imbalance between estradiol and progesterone play a role? Endocr. Res. 40(4), 204–210 (2015). https://doi.org/10.3109/07435800.2015.1015730
C.W. Ho, H.H. Chen, M.C. Hsieh et al. Increased Risk of Polycystic Ovary Syndrome and It’s Comorbidities in Women with Autoimmune Thyroid Disease. Int J. Environ. Res. Public Health 17(7), 2422 (2020). https://doi.org/10.3390/ijerph17072422
M. Sharma, A. Modi, M. Goyal, P. Sharma, P. Purohit, Anti-thyroid antibodies and the gonadotrophins profile (LH/FSH) in euthyroid polycystic ovarian syndrome women. Acta Endocrinol. Buchar. Rom. 18(1), 79–85 (2022). https://doi.org/10.4183/aeb.2022.79
C. De Geyter, L. Matt, I. De Geyter, R. Moffat, C. Meier, In infertile women with subclinical hypothyroidism, with or without thyroid peroxidase antibodies, serum TSH during pregnancy follows preconception values and thyroid hormones remain stable. Hum. Reprod. Open 2023(4), hoad038 (2023). https://doi.org/10.1093/hropen/hoad038
C.A. Emdin, A.V. Khera, S. Kathiresan, Mendelian Randomization. JAMA 318(19), 1925–1926 (2017). https://doi.org/10.1001/jama.2017.17219
A. Teumer, L. Chaker, S. Groeneweg et al. Genome-wide analyses identify a role for SLC17A4 and AADAT in thyroid hormone regulation. Nat. Commun. 9(1), 4455 (2018). https://doi.org/10.1038/s41467-018-06356-1
F. Day, T. Karaderi, M.R. Jones et al. Large-scale genome-wide meta-analysis of polycystic ovary syndrome suggests shared genetic architecture for different diagnosis criteria. PLoS Genet. 14(12), e1007813 (2018). https://doi.org/10.1371/journal.pgen.1007813
M. I. Kurki, J. Karjalainen, P. Palta, T. P. Sipilä, K. Kristiansson, K. M. Donner, M. P. Reeve, H. Laivuori, M. Aavikko, M. A. Kaunisto, A. Loukola, E. Lahtela, H. Mattsson, P. Laiho, P. Della Briotta Parolo, A. A. Lehisto, M. Kanai, N. Mars, J. Rämö, T. Kiiskinen, … A. Palotie, FinnGen provides genetic insights from a well-phenotyped isolated population. Nature, 613(7944), 508–518 (2023). https://doi.org/10.1038/s41586-022-05473-8
J.S. Tyrmi, R.K. Arffman, N. Pujol-Gualdo et al. Leveraging Northern European population history: novel low-frequency variants for polycystic ovary syndrome. Hum. Reprod. Oxf. Engl. 37(2), 352–365 (2022). https://doi.org/10.1093/humrep/deab250
J. M. Fussey, R. N. Beaumont, A. R. Wood, B. Vaidya, J. Smith, J. Tyrrell, Does Obesity Cause Thyroid Cancer? A Mendelian Randomization Study. J. Clin. Endocrinol. Metab. 105(7), e2398–e2407 (2020). https://doi.org/10.1210/clinem/dgaa250
GIANT Consortium, P. Wojciechowski, A. Lipowska et al. Impact of FTO genotypes on BMI and weight in polycystic ovary syndrome: a systematic review and meta-analysis. Diabetologia 55(10), 2636–2645 (2012). https://doi.org/10.1007/s00125-012-2638-6
C. J. Glueck, N. Goldenberg, Characteristics of obesity in polycystic ovary syndrome: Etiology, treatment, and genetics. Metabolism: clinical and experimental, 92, 108–120 (2019). https://doi.org/10.1016/j.metabol.2018.11.002
Q. Liu, Z. Zhu, P. Kraft, Q. Deng, E. Stener-Victorin, X. Jiang, Genomic correlation, shared loci, and causal relationship between obesity and polycystic ovary syndrome: a large-scale genome-wide cross-trait analysis. BMC medicine, 20(1), 66 (2022). https://doi.org/10.1186/s12916-022-02238-y
C. Yao, Y. Zhang, P. Lu et al. Exploring the bidirectional relationship between pain and mental disorders: a comprehensive Mendelian randomization study. J. Headache Pain. 24(1), 82 (2023). https://doi.org/10.1186/s10194-023-01612-2
L. Chen, H. Yang, H. Li, C. He, L. Yang, G. Lv, Insights into modifiable risk factors of cholelithiasis: A Mendelian randomization study. Hepatology (Baltimore, Md.) 75(4), 785–796. (2022). https://doi.org/10.1002/hep.32183
Y. Guo, Y. Dai, H. Yu, S. Zhao, D.C. Samuels, Y. Shyr, Improvements and impacts of GRCh38 human reference on high throughput sequencing data analysis. Genomics 109(2), 83–90 (2017). https://doi.org/10.1016/j.ygeno.2017.01.005
S. Burgess, A. Butterworth, S.G. Thompson, Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 37(7), 658–665 (2013). https://doi.org/10.1002/gepi.21758
J. Bowden, M. F. Del Greco, C. Minelli, G. Davey Smith, N. A. Sheehan, J. R. Thompson, Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: the role of the I2 statistic. Int. J. Epidemiol. 45(6), 1961–1974 (2016). https://doi.org/10.1093/ije/dyw220
J. Bowden, G. Davey Smith, S. Burgess, Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J. Epidemiol. 44(2), 512–525 (2015). https://doi.org/10.1093/ije/dyv080
L. Xiao, S. Liu, Y. Wu et al. The interactions between host genome and gut microbiome increase the risk of psychiatric disorders: Mendelian randomization and biological annotation. Brain Behav. Immun. 113, 389–400 (2023). https://doi.org/10.1016/j.bbi.2023.08.003
D.A. Lawlor, L. Benfield, J. Logue et al. Association between general and central adiposity in childhood, and change in these, with cardiovascular risk factors in adolescence: prospective cohort study. BMJ 341, c6224 (2010). https://doi.org/10.1136/bmj.c6224
F.P. Hartwig, N.M. Davies, G. Hemani, G. Davey Smith, Two-sample Mendelian randomization: avoiding the downsides of a powerful, widely applicable but potentially fallible technique. Int J. Epidemiol. 45(6), 1717–1726 (2016). https://doi.org/10.1093/ije/dyx028
M. Verbanck, C.Y. Chen, B. Neale, R. Do, Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet 50(5), 693–698 (2018). https://doi.org/10.1038/s41588-018-0099-7
S. Burgess, G. Davey Smith, N.M. Davies et al. Guidelines for performing Mendelian randomization investigations. Wellcome Open Res 4, 186 (2019). https://doi.org/10.12688/wellcomeopenres.15555.2
S. Burgess, G. Davey Smith, N.M. Davies et al. Guidelines for performing Mendelian randomization investigations: update for summer 2023. Wellcome Open Res 4, 186 (2023). https://doi.org/10.12688/wellcomeopenres.15555.3
J. H. Jung, J. R. Hahm, T. S. Jung, H. J.Kim, H. S. Kim, S. Kim, S. K. Kim, S. M. Lee, D. R. Kim, W. J. Choi, Y. M. Seo, S. I. Chung, A 27-year-old woman diagnosed as polycystic ovary syndrome associated with Graves' disease. Internal medicine (Tokyo, Japan), 50(19), 2185–2189 (2011). https://doi.org/10.2169/internalmedicine.50.5475
S. Nisar, P.A. Shah, M.S. Kuchay et al. Association of polycystic ovary syndrome and Graves’ disease: Is autoimmunity the link between the two diseases. Indian J. Endocrinol. Metab. 16(6), 982–986 (2012). https://doi.org/10.4103/2230-8210.103006
S. Gaberšček, K. Zaletel, V. Schwetz, T. Pieber, B. Obermayer-Pietsch, E. Lerchbaum, Mechanisms in Endocrinology: Thyroid and polycystic ovary syndrome. Eur. J. Endocrinol. 172(1), R9–R21 (2015). https://doi.org/10.1530/EJE-14-0295
R. S. Legro, D. Driscoll, J. F. Strauss, J. Fox, A. Dunaif, Evidence for a genetic basis for hyperandrogenemia in polycystic ovary syndrome. Proceedings of the National Academy of Sciences of the United States of America 95(25), 14956–14960 (1998). https://doi.org/10.1073/pnas.95.25.14956
S. Feigl, B. Obermayer-Pietsch, P. Klaritsch et al. Impact of Thyroid Function on Pregnancy and Neonatal Outcome in Women with and without PCOS. Biomedicines 10(4), 750 (2022). https://doi.org/10.3390/biomedicines10040750
G. Morgante, M.C. Musacchio, R. Orvieto, M.G. Massaro, V. De Leo, Alterations in thyroid function among the different polycystic ovary syndrome phenotypes. Gynecol. Endocrinol. J. Int Soc. Gynecol. Endocrinol. 29(11), 967–969 (2013). https://doi.org/10.3109/09513590.2013.829445
R. Pasquali, A. Gambineri, U. Pagotto, The impact of obesity on reproduction in women with polycystic ovary syndrome. BJOG : an international journal of obstetrics and gynaecology, 113(10), 1148–1159 (2006). https://doi.org/10.1111/j.1471-0528.2006.00990.x
Acknowledgements
We express our gratitude to the patients and investigators who contributed to the GWAS. We thank the Figdraw platform for providing drawing materials. Q.Z. and B.Z. thank Dr. Liang Zheng from Department of Epidemiology and Public Health, Tongji University School of Medicine, Shanghai for statistical support of this paper.
Funding
This work was supported by the Natural Science Foundation of Shanghai (Grant Number:22ZR1448700) and Foundation of Shanghai Fifth People’s Hospital (Grant Number:2022WYZD01). The funders have no influence on the data collection, analyses or conclusions of the study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Q.Z. and B.Z. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Q.Z., K.W. and B.Z. conceived and designed the study. Q.Z. and W.K. undertook the statistical analyses. Q.Z. and J.Y. wrote the first draft of the manuscript. K.W. and B.Z. are the study guarantor. Q.Z., P.Z., Q.Y. and F.P. interpreted data, reviewed the paper, and made critical revision of the manuscript for important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Q., Ke, W., Ye, J. et al. Is thyroid function associated with polycystic ovary syndrome? A bidirectional Mendelian randomization study. Endocrine (2024). https://doi.org/10.1007/s12020-024-03756-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12020-024-03756-w