Abstract
Purpose
Polycystic ovarian syndrome (PCOS) is a common heterogeneous condition with probably multifactorial genesis. Animal studies have proven the essential role of the sympathetic nervous system in the syndrome development, while human studies are still contradictory. The present study aims to investigate the possible influence of plasma-free metanephrine (MN), and normetanephrine (NMN), nerve growth factor (NGF), and renalase (RNL) on the hormonal and metabolic parameters in women with PCOS and healthy controls.
Methods
Fifty patients with PCOS and 30 healthy women participated in the study. The plasma-free MN and NMN, NGF, RNL, anti-Mullerian hormone (AMH), gonadotropin, androgen levels, and metabolic parameters were investigated.
Results
Plasma-free NMN and NGF concentrations were increased in PCOS individuals, while RNL levels were decreased compared to healthy volunteers. Increased plasma-free NMN (OR = 1.0213 [95%CI 1.0064–1.0364], p = 0.005) and NGF (OR = 1.0078 [95%CI 1.0001–1.0155], p = 0.046) but not MN or RNL levels were associated with a higher risk of PCOS after adjustment for age. Plasma-free NMN levels were positively associated with the LH (r = +0.253; p = 0.039). androstenedione (r = +0.265; p = 0.029), 17-OH progesterone (r = +0.285; p = 0.024), NGF (r = +0.320; p = 0.008), and AMH (r = +0.417; p < 0.001) concentrations of the investigated women. RNL levels were inversely related to the BMI (r = −0.245; p = 0.029), HOMA-IR (r = −0.250; p = 0.030), free testosterone (r = −0.303; p = 0.006) levels. systolic (r = −0.294; p = 0.008) and diastolic (r = −0.342; p = 0.002) blood pressure.
Conclusions
Increased sympathetic noradrenergic activity and NGF synthesis might be related to the increased AMH and delta-4 androgen levels in a subgroup of PCOS patients. RNL levels might influence the metabolic status of PCOS patients. Further studies are needed to explore the significance of adrenal medullar and autonomic dysfunction for developing different PCOS phenotypes and their subsequent cardiovascular complications.
Similar content being viewed by others
Introduction
Polycystic ovarian syndrome (PCOS) is a condition with various symptoms, which have been reported as far back as in the writings of ancient Greek and medieval physicians [1]. However, the first systematic description of the syndrome was published by Stein and Leventhal, presenting seven infertile amenorrheic women with bilateral enlarged polycystic ovaries [2]. After that, it became clear that symptoms of other disorders might overlap with PCOS phenotype, e.g., congenital adrenal hyperplasia, prolactinoma, and androgen-producing tumors [3]. Thus, current criteria for the syndrome require the exclusion of these conditions and support the heterogeneous nature of PCOS by allowing women with different clinical phenotypes to be diagnosed with the condition [4]. Nowadays, the presence of hyperandrogenism, chronic anovulation, and polycystic ovarian morphology by ultrasound are the key criteria for PCOS diagnosis [4, 5]. Additionally, screening for metabolic disturbances and cardiovascular risk factors in PCOS women is strongly recommended by most guidelines [6].
Despite the syndrome’s long history, the pathogenesis of PCOS is still unclarified, though a complex interaction of various genetic, neuroendocrine, and environmental factors has been assumed [7]. Therefore, different animal models of the condition were developed to reveal diverse mechanisms leading to ovarian dysfunction. For example, a PCOS-like phenotype might be induced in rodents by administering estrogens, androgens, antiprogestins, or aromatase inhibitors [reviewed in ref. 8]. The ovaries of rats injected with a single dose of estradiol valerate showed increased nerve growth factor (NGF) and noradrenaline (NA) concentrations and became polycystic [9]. However, the simultaneous treatment with estradiol valerate and beta-adrenoreceptor blocker decreased tyrosine hydroxylase activity, testosterone, and estradiol levels and prevented the development of multiple ovarian cysts [10]. The close interaction between ovarian sympathetic noradrenergic hyperstimulation, increased levels of NGF, and polycystic ovarian morphology in animals raises the question if the sympathetic hyperactivity might be involved in the pathogenesis of PCOS in women [11]. Hence, Sverrisdóttir et al. found increased sympathetic nerve activity in patients with PCOS by direct measurement [12]. Other authors obtained similar results using the heart rate variability for indirect evaluation of autonomous function [13, 14]. However, few studies have investigated the plasma levels of catecholamines and their metabolites in PCOS patients with somewhat contradictory results [15,16,17]. Furthermore, the role of the other factors probably involved in the catecholamine release and metabolism, e.g., the neurotrophin NGF and the flavoprotein renalase, has not been thoroughly evaluated in PCOS patients [18, 19].
Therefore, the present study aims to investigate the possible interaction between plasma-free nephrines, NGF, renalase, hormonal and metabolic parameters in women with PCOS compared to healthy controls.
Materials and methods
Participants
Eighty women of reproductive age (18–37 years) participated in the study. Fifty patients were diagnosed with PCOS according to the ESHRE criteria [4, 5]. They presented in the Endocrine department with different complaints, e.g., hirsutism, acne, menstrual irregularities, infertility, obesity, and metabolic disturbances. Thirty-six women were with “classic hyperandrogenic” PCOS (phenotypes A and B), while other 14 women were with “ovulatory” PCOS or “non-hyperandrogenic” PCOS (phenotypes C and D) [20].
In all of the patients, other causes for symptoms, e.g., prolactinoma, thyroid dysfunction, late-onset congenital adrenal hyperplasia, and the adrenal or ovarian tumor, had been excluded by appropriate tests. Additional exclusion criteria were: pregnancy and breastfeeding, the presence of overt diabetes mellitus, the presence of hypertension, the use of oral contraceptives, glucocorticoids, or other medication that could interfere with hormonal indices, renal or hepatic insufficiency, mental illnesses and other severe concomitant diseases. A total of 14 PCOS patients were on metformin treatment for insulin resistance or prediabetes.
Thirty healthy women with regular menstruations, no history of polycystic ovaries or ovarian surgery, and no clinical signs of hyperandrogenism volunteered for the study.
A complete personal and family history of participants was collected. Physical assessment, including height, weight, body mass index (BMI), presence of hirsutism and/or acne, as well as blood pressure, was performed in all women. In addition, blood samples for biochemical and hormonal assays were taken in the follicular phase of the menstrual cycle between 08.00 and 09.00 a.m. after an overnight fast, in a supine position after a 30-min rest as previously described [21, 22]. All participants gave written informed consent for participation.
Study protocol and hormonal investigations
All participants underwent biochemical investigations with measurement of fasting glucose, high-density lipoprotein cholesterol levels (HDL-ch), low-density lipoprotein cholesterol levels (LDL-ch), triglycerides (TG), total cholesterol (TC), creatinine, liver enzymes, and uric acid. All parameters were determined enzymatically by an automatic analyzer (Cobas Mira Plus; Hoffmann La Roche). Hormonal investigations included immunoreactive insulin (IRI), total testosterone (TT), sex-hormone binding globulin (SHBG), luteinizing hormone (LH), follicle-stimulating hormone (FSH), androstenedione (A4), dehydroepiandrosterone-sulfate (DHEAS), 17-OH progesterone (17OHP), prolactin (Prl), thyroid-stimulating hormone (TSH) and anti-Mullerian hormone (AMH), measured through commercially available radioimmunologic kits. Additionally, free testosterone levels (http://www.issam.ch/freetesto.html) (FT) and homeostasis model assessment—insulin resistance index (HOMA-IR) were calculated.
Blood samples for plasma-free metanephrines (metanephrine and normetanephrines), beta-nerve growth factor (NGF), and renalase (RNL) were taken in the morning, after 30 min of rest in a supine position and were stored at −80 °C until analyzes. NGF and RNL were measured in all participants, while plasma-free metanephrines were measured in 29 controls and 39 PCOS patients. NGF was measured by ELISA kit (MBS2603037, MyBioSource.com) with intra-assay precision ≤8%, inter-assay precision ≤12%, and analytical sensitivity—5 pg/ml. Human RNL was measured by ELISA kit (MBS2600871, MyBioSource.com) with intra-assay precision ≤8%, inter-assay precision ≤12%, and analytical sensitivity—0.5 ng/ml. Plasma-free metanephrines were established by RIA (DER8300, Demeditec Diagnostic GmbH, Germany) with the following specific characteristics: for plasma-free metanephrine (MN): reference range <65 pg/ml; analytical sensitivity 6.4 pg/mL; for plasma-free normetanephrine (NMN) reference range <196 pg/ml; analytical sensitivity 24.1 pg/mL.
Statistical analysis
Descriptive statistics and frequency analyses were used. Differences between categorical variables were established by Chi-square and Fisher’s exact tests. A Kolmogorov–Smirnov test showed that most parameters deviated from the normal distribution. Therefore, nonparametric tests, e.g., Mann-Whitney and Kruskal Wallis tests, were used to establish differences between two or more groups, respectively. The results were presented as a median ± interquartile range for continuous variables or as a frequency (%). Associations between variables were estimated through a two-tailed Spearman’s correlation analysis. Binary logistic regression was used to explore the predictors of PCOS after adjustment for possible confounders. A p-level < 0.05 was considered statistically significant. The data were analyzed by MedCalc® Statistical Software version 20.110 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2022).
Results
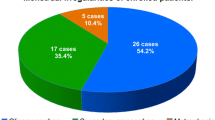
The anthropometric, biochemical, and hormonal results of women with PCOS compared to healthy controls are presented in Table 1. Patients with PCOS were younger than healthy women, but with increased levels of insulin, HOMA-IR, triglycerides, androgens, prolactin, LH and AMH as expected. Plasma-free NMN and NGF levels were increased in PCOS individuals, while RNL levels were decreased in comparison to healthy volunteers (Fig. 1).
Women with regular menstrual cycle had significantly lower levels of plasma-free NMN and NGF and higher levels of RNL in comparison to women with menstrual disturbances (Fig. 2). Individuals with polycystic ovaries by ultrasound had increased levels of plasma-free NMN and NGF levels compared to other women, but no differences in plasma-free MN and RNL levels were found (Fig. 3).
Patients with PCOS and hirsutism (n = 28) were with significantly lower SHBG (40.40 nmol/l [23.20–53.35] vs. 64.45 nmol/l [30.50–93.20], p = 0.021), increased androstendione (5.25 ng/ml [4.77–5.86] vs. 4.00 ng/ml [2.70–5.70], p = 0.041) and plasma-free NMN (98.15 pg/ml [93.80–126.20] vs. 80.70 pg/ml [47.70–110.15], p = 0.016) levels compared to non-hirsute PCOS patients (n = 22), while no differences were found in regard to other laboratory parameters (p > 0.05 for all). A total of 18 PCOS patients suffered from acne, but their hormonal characteristics were similar to those without skin lesions (p > 0.05 for all). Patients with “hyperandrogenic” PCOS phenotype were with increased BMI (24.07 kg/m2 [20.43–29.45] vs. 20.40 kg/m2 [18.50–24.16], p = 0.041), androgen (free testosterone: 38.95 pmol/l [21.35–63.10] vs. 16.70 pmol/l [12.40–37.80], p = 0.010; androstendione: 5.35 ng/ml [4.10–6.30] vs. 3.45 ng/ml [2.60–4.40], p = 0.007), and LH levels (6.35 IU/l [4.30–9.00] vs. 3.45 IU/l [2.70–5.30], p = 0.004) compared to other PCOS phenotypes, as expected, while no differences in plasma-free metanephrines, NGF and RNL were established (p > 0.05 for all). Overweight and obese PCOS women (n = 19) (BMI ≥ 25) showed significantly lower RNL levels than leaner patients (n = 31) (10,50 ng/ml [9.16–11.76] vs. 12.30 ng/ml [10.96–13.42], p = 0.035), while the levels of NGF, and plasma-free metanephrines were similar in both groups.
Logistic regression analyses showed that increased plasma-free NMN (OR = 1.0213 [95%CI 1.0064–1.0364], p = 0,005) but not plasma-free MN (p > 0.05) were associated with a higher risk of PCOS after adjustment for age. Similarly, the levels of NGF (OR = 1,0078 [95%CI 1.0001–1.0155], p = 0,046) but not the RNL (p > 0.05) levels were significantly associated with increased risk of PCOS after adjustment for age. Similar results were obtained after adjustment for age, BMI, and metformin use (data not shown).
Plasma-free NMN levels were positively associated with the LH, androstendione, 17-OH progesterone, NGF, and AMH concentrations of investigated women. Plasma free MN levels were positively related to age, and inversely associated with the free testosterone levels (Table 2).
NGF levels correlated with LH, prolactin, AMH, androstendione and 17-OH progesterone (Table 2). RNL levels were related to the creatinine levels (r = +0.313; p = 0.005), BMI (r = −0.245; p = 0.029), systolic (r = −0.294; p = 0.008) and diastolic (r = −0.342; p = 0.002) blood pressure.
Discussion
Our study has shown increased fasting plasma-free NMN but not MN levels in PCOS women compared to healthy women, thus, emphasizing the vital role of increased sympathetic activity in PCOS [23]. Forty years ago, Lobo et al. have found increased noradrenalin (NA) metabolites in PCOS patients [15], but nevertheless, the topic still needs to be revised. In a comprehensive study evaluating the catecholamines and their metabolites in adolescents, Garcia-Rudaz et al. described significantly higher normetanephrine excretion in PCOS patients than in controls [16]. Additionally, increased plasma and urine levels of the main catecholamine metabolite 3-methoxy-4-hydroxyphenyl-glycol were detected in PCOS patients compared to healthy women [15, 17, 24]. However, the plasma NA levels did not differ between PCOS patients and controls or between infertile PCOS individuals and women with other reasons for infertility [11, 25]. Therefore, the discrepancy between normal plasma NA levels and increased catecholamine metabolites in PCOS might be explained by a decreased neuronal NA reuptake leading to exaggerated extraneuronal metabolism [16, 24, 26]. Hence, NA reuptake, transport, storage, regulated release, and conversion to NMN have been observed in human granulosa and theca cells [27, 28]. Moreover, the density of ovarian noradrenergic fibers is increased in PCOS patients compared to women with regular menstruation, which could influence ovarian steroidogenesis [29, 30].
In contrast to increased plasma-free NMN in PCOS patients, our former study did not find differences in urine NMN excretion between PCOS patients and controls [21]. Thus, increased subsequent NMN conversion to other metabolites might be suggested, but further studies are needed to test that hypothesis.
Additionally, plasma-free NMN levels in our participants were positively related to LH, 17-OH progesterone, androstenedione, and AMH concentrations. Our results support the experimental finding that NA might amplify human chorionic gonadotropin-dependent androgen production in theca-interstitial cells, influencing the delta-4-pathway [31]. Other studies did not find associations between plasma catecholamine metabolites and LH, while the urine 3-methoxy-4-hydroxyphenyl-glycol concentrations were positively related to LH, testosterone, and DHEAS levels in PCOS patients [15, 17]. Interestingly, Ramadan fasting but not the sympatholytic drug moxonidine might significantly decrease the sympathetic activity in women with PCOS [32, 33]. Therefore, further studies are needed to reveal if chronic caloric restriction could influence the hyperandrogenic environment in PCOS women by modulating NA levels.
NGF is a significant trophic factor for the peripheral sympathetic neurons that influences NA levels by the selective increase of the tyrosine hydroxylase and dopamine-beta hydroxylase activity in the sympathetic ganglia and adrenal medulla [34]. Inversely, catecholamines could also stimulate NGF synthesis in different tissues by a mechanism independent of adrenergic receptors [35]. In the ovaries of transgenic mice overexpressing NGF, the increased neurotrophin synthesis amplifies the local NA production and induces systemic sympathetic hyperactivity [36]. Furthermore, estradiol valerate application in female rodents increases the NGF synthesis and noradrenergic activity leading to increased androgen production and the development of PCOS-like phenotype [37,38,39]. Though rodent models could not fully resemble the multifaceted PCOS presentation in humans [40], our results showed similarly increased systemic NGF levels in PCOS women compared to the control group, which correlated positively with plasma-free NMN and AMH concentrations. Likewise, in women undergoing in vitro procedures, different though not all, authors have described increased NGF levels in the follicular fluid of PCOS individuals compared to other patients [41,42,43]. However, in circulation, Zangenesh et al. found significantly lower NGF levels in PCOS patients compared to other individuals, which might be explained by prolonged chronic psychological stress [44, 45]. Hence, in the Iranian study, the PCOS and the control group comprised women with infertility – a well-known risk factor for anxiety and depression [44, 46]. Conversely, infertile women were not included as controls in our study, and the presence of psychiatric disorders or treatment was among the exclusion criteria for all participants.
Our data showed that the NGF levels correlated positively with 17-OH progesterone and androstenedione of the investigated women, as in rodent models [36, 37]. Additionally, we found positive associations between NGF and LH levels, while ovarian NGF overexpression did not influence gonadotropin concentrations in transgenic mice [36, 41]. However, the interrelations between NGF and LH might be species-specific because NGF is a potent stimulator of gonadotropin-releasing hormone activity and LH release in other female animals, e.g., llamas and dairy heifers [47, 48]. Thus, our data suggest possible interrelations between systemic NGF concentrations, ovarian androgen synthesis, and pituitary gonadotropin release that might favor the development of PCOS in a subset of women.
The increased NGF levels in the circulation of our patients might originate from ovaries, but other sources, including pituitary and adipose tissue, could not be excluded [49, 50]. Hence, NGF and prolactin are co-secreted by the mammotroph cells in the anterior pituitary, and hypothalamic dysregulation might alter their systemic levels [49, 51]. Tubero-infundibular dopaminergic dysfunction is a well-known feature of PCOS, leading to mild hyperprolactinemia in many patients [52, 53]. Our data showed significant associations between NGF and prolactin levels, which need further evaluation.
Additionally, NGF synthesis has been observed in rodent and human white adipose tissue [50]. However, the sympathetic system is not a significant modulator of the NGF release in fat mass, unlike ovaries [50]. NGF secretion has been studied in patients with obesity and metabolic disturbances, but the results are somewhat contradictory [54,55,56]. Chronic sympathetic nervous system overactivity is a well-known factor linking adiposity, insulin resistance, and metabolic abnormalities [57]. However, in our study, NGF levels did not differ between lean and obese PCOS women, and no correlations between the neurotrophin and metabolic parameters were established. Conceivably, the powerful and complex effects of hyperandrogenism and hyperinsulinemia on metabolic parameters in PCOS and the heterogeneity of the syndrome per se could mask the influence of other milder factors. Additional studies are needed to investigate the possible impact of NGF on metabolic indices in different PCOS phenotypes.
Renalase (RNL) has been discovered in 2005 as a flavoprotein involved in the extracellular inactivation of dopamine, adrenaline, and noradrenaline, though its plasma catalytic function has been doubted by some researchers [19, 58]. Additionally, RNL is a cytokine that modulates the mitogen-activated protein kinase pathway leading to cytoprotective, anti-inflammatory, and antiapoptotic effects [reviewed in 59]. According to current knowledge, RNL might modulate blood pressure in animals and humans by influencing catecholamine metabolism, renal dopamine secretion, and renal sympathetic innervation [19, 59, 60]. For instance, the renalase-knockout mice showed increased systolic and diastolic blood pressure and increased catecholamine concentrations compared to the wild-type animals despite normal renal function [61]. Additionally, the genetically modified animals suffered from more severe ischemic myocardial damage suggesting substantial tissue-protective effects of the RNL in hypoxia [61]. Plasma RNL levels might vary in hypertensive patients according to their age, renal function, catecholamine levels, reasons for increased blood pressure, and antihypertensive therapy [62, 63]. For instance, a low level of renalase has been related to an increased risk of preeclampsia during pregnancy, and the flavoprotein concentrations were negatively associated with pregnant women’s systolic and diastolic blood pressure [64]. However, RNL levels were increased in adolescent hypertensive patients compared to controls and correlated positively with blood pressure values [65]. The renalase levels have not been investigated in hypertensive PCOS patients. Still, our results showed slightly lower RNL levels in young normotensive PCOS women compared to healthy controls with negative correlations between RNL and blood pressure levels. Further, longitudinal studies are needed to reveal if the slightly lower RNL levels in PCOS predict an increased prevalence of hypertension and cardiovascular complications in the future.
Currently, RNL is investigated mainly in the context of chronic kidney, cardiovascular and oncologic diseases [60], while the possible associations with reproductive disturbances are poorly explored. However, abundant RNL expression has been described in rodent ovaries and adrenal glands [66]. Moreover, the gonadotropin-releasing hormone antagonist administration leads to decreased ovarian RNL expression [66]. At the same time, leptin deficiency increases the RNL levels in ovaries, which suggests possible associations between RNL, metabolism, and ovarian function [66]. Studies investigating RNL concentrations in PCOS are lacking, though rs10887800 RNL genetic polymorphism has been associated with PCOS-related infertility [67]. Fatima et al. hypothesize that polymorphisms in the RNL gene might be related to impaired catecholamine degradation and stress-induced changes in fertility [67]. Accordingly, we found decreased RNL and increased plasma-free NMN levels in women with PCOS. However, we did not find direct associations between catecholamine metabolites and RNL, which suggests that other factors might contribute to simultaneous changes in catecholamines and RNL in patients with PCOS. Moreover, our results showed decreased RNL concentrations in obese patients with PCOS compared to lean PCOS patients, which might result from the well-known adverse effects of obesity on renal function [68]. Our study also found that RNL was inversely related to insulin resistance, total and free testosterone. Further investigations are needed to explain the pathophysiological mechanisms underlying these findings.
Based on the comprehensive Rotterdam criteria, women with different phenotypes might be diagnosed with PCOS [4, 5]. Nevertheless, PCOS is still a diagnosis of exclusion with heterogenous clinical symptoms and probably multi-causal genesis [4, 5, 69, 70]. Therefore, we could assume that increased ovarian sympathetic noradrenergic activity and NGF synthesis are common characteristics of a subgroup of PCOS patients, who present with polycystic ovaries, increased AMH, LH, and delta-4 androgen levels irrespective of their metabolic status. Additionally, the lower RNL levels in some obese PCOS patients might be associated with the development of renal dysfunction and increased blood pressure. To the best of our knowledge, the current study explores the complex interrelations between catecholamine metabolites, NGF, and RNL in adult PCOS patients for the first time. However, we have measured systemic blood concentrations but not local ovarian production of NMN or NGF, which is the study’s main limitation. Additionally, blood samples were collected during the Covid-19 pandemic, which could be associated with higher-than-usual levels of distress in the general population [71], thus, influencing the endogenous stress response mechanisms in the participants.
In conclusion, our study has found increased plasma-free NMN and NGF levels in PCOS, especially in patients with ovarian cystic morphology. These correlate with the ovarian delta-4 androgen and AMH levels but not with the metabolic characteristics of patients. Differences in RNL levels between lean and obese PCOS patients might modulate the development of increased blood pressure. Further studies are needed to explore the significance of adrenal medullar and autonomic dysfunction for developing different PCOS phenotypes and their subsequent cardiovascular complications.
References
R. Azziz, D.A. Dumesic, M.O. Goodarzi, Polycystic ovary syndrome: an ancient disorder? Fertil. Steril. 95, 1544–1548 (2011)
I. Stein, M. Leventhal, Amenorrhea associated with bilateral polycystic ovaries. Am. J. Obstet. Gynecol. 29, 181–191 (1935)
H.F. Escobar-Morreale, Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat. Rev. Endocrinol. 14, 270–284 (2018)
H.J. Teede, M.L. Misso, M.F. Costello, A. Dokras, J. Laven, L. Moran, T. Piltonen, R.J. Norman, Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum. Reprod. 33, 1602–1618 (2018)
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group, Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil. Steril. 81, 19–25 (2004)
B.H. Al Wattar, M. Fisher, L. Bevington, V. Talaulikar, M. Davies, G. Conway, E. Yasmin, Clinical practice guidelines on the diagnosis and management of polycystic ovary syndrome: a systematic review and quality assessment study. J. Clin. Endocrinol. Metab. 106, 2436–2446 (2021)
R.L. Rosenfield, D.A. Ehrmann, The Pathogenesis of Polycystic Ovary Syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr. Rev. 37, 467–520 (2016)
S. Osuka, N. Nakanishi, T. Murase, T. Nakamura, M. Goto, A. Iwase, F. Kikkawa, Animal models of polycystic ovary syndrome: a review of hormone-induced rodent models focused on hypothalamus-pituitary-ovary axis and neuropeptides. Reprod. Med. Biol. 18, 151–160 (2018)
R. Sotomayor-Zárate, M. Dorfman, A. Paredes, H.E. Lara, Neonatal exposure to estradiol valerate programs ovarian sympathetic innervation and follicular development in the adult rat. Biol. Reprod. 78, 673–680 (2008)
B. Venegas, L.Y. De León Gordillo, G. Rosas, J.A. Espinoza, C. Morán, R. Domínguez, L. Morales-Ledesma, In rats with estradiol valerate-induced polycystic ovary syndrome, the acute blockade of ovarian β-adrenoreceptors improve ovulation. Reprod. Biol. Endocrinol. 17, 95 (2019)
A. Lansdown, D.A. Rees, The sympathetic nervous system in polycystic ovary syndrome: a novel therapeutic target? Clin. Endocrinol. 77, 791–801 (2012)
Y.B. Sverrisdóttir, T. Mogren, J. Kataoka, P.O. Janson, E. Stener-Victorin, Is polycystic ovary syndrome associated with high sympathetic nerve activity and size at birth? Am. J. Physiol. Endocrinol. Metab. 294, E576–E581 (2008)
A. Yildirir, F. Aybar, G. Kabakci, H. Yarali, A. Oto, Heart rate variability in young women with polycystic ovary syndrome. Ann. Noninvasive Electrocardiol. 11, 306–312 (2006)
H.R. Ji, H.L. Woo, Y.J. Park, D.S. Hwang, J.M. Lee, C.H. Lee, J.B. Jang, K.S. Park, Characteristics of heart rate variability in women with polycystic ovary syndrome: a retrospective cross-sectional study. Medicines 97, e12510 (2018)
R.A. Lobo, L.R. Granger, W.L. Paul, U. Goebelsmann, D.R. Mishell Jr., Psychological stress and increases in urinary norepinephrine metabolites, platelet serotonin, and adrenal androgens in women with polycystic ovary syndrome. Am. J. Obstet. Gynecol. 145, 496–503 (1983)
C. Garcia-Rudaz, I. Armando, G. Levin, M.E. Escobar, M. Barontini, Peripheral catecholamine alterations in adolescents with polycystic ovary syndrome. Clin. Endocrinol. 49, 221–228 (1998)
K. Yoshino, K. Takahashi, A. Nishigaki, Y. Eda, M. Kitao, Plasma catecholamine metabolites and polycystic ovary syndrome. Asia Ocean. J. Obstet. Gynaecol. 16, 57–62 (1990)
R. Levi-Montalcini, R. Dal Toso, F. della Valle, S.D. Skaper, A. Leon, Update of the NGF saga. J. Neurol. Sci. 130, 119–127 (1995)
J. Xu, G. Li, P. Wang, H. Velazquez, X. Yao, Y. Li, Y. Wu, A. Peixoto, S. Crowley, G.V. Desir, Renalase is a novel, soluble monoamine oxidase that regulates cardiac function and blood pressure. J. Clin. Investig. 115, 1275–1280 (2005)
D. Lizneva, L. Suturina, W. Walker, S. Brakta, L. Gavrilova-Jordan, R. Azziz, Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil. Steril. 106, 6–15 (2016)
R. Robeva, N. Arnaudova, G. Kirilov, A. Elenkova, S. Zacharieva, Metanephrine and normetanephrine urine excretion in patients with PCOS. Acta Med. Bulg. 49, 5–10 (2022)
D. Dewailly, M.Š. Alebić, A. Duhamel, N. Stojanović, Using cluster analysis to identify a homogeneous subpopulation of women with polycystic ovarian morphology in a population of non-hyperandrogenic women with regular menstrual cycles. Hum. Reprod. 29, 2536–2543 (2014)
A.J. Lansdown, E.A.H. Warnert, Y. Sverrisdóttir, R.G. Wise, D.A. Rees, Regional cerebral activation accompanies sympathoexcitation in women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 104, 3614–3623 (2019)
G. Eisenhofer, W. Pecorella, K. Pacak, D. Hooper, I.J. Kopin, D.S. Goldstein, The neuronal and extraneuronal origins of plasma 3-methoxy-4-hydroxyphenylglycol in rats. J. Auton. Nerv. Syst. 50, 93–107 (1994)
X. Shi, L. Zhang, S. Fu, N. Li, Co-involvement of psychological and neurological abnormalities in infertility with polycystic ovarian syndrome. Arch. Gynecol. Obstet. 284, 773–778 (2011)
G. Eisenhofer, I.J. Kopin, D.S. Goldstein, Catecholamine metabolism: a contemporary view with implications for physiology and medicine. Pharmacol. Rev. 56, 331–349 (2004)
S. Saller, J. Merz-Lange, S. Raffael, S. Hecht, R. Pavlik, C. Thaler, D. Berg, U. Berg, L. Kunz, A. Mayerhofer, Norepinephrine, active norepinephrine transporter, and norepinephrine-metabolism are involved in the generation of reactive oxygen species in human ovarian granulosa cells. Endocrinology 153, 1472–1483 (2012)
M. Greiner, A. Paredes, V. Rey-Ares, S. Saller, A. Mayerhofer, H.E. Lara, Catecholamine uptake, storage, and regulated release by ovarian granulosa cells. Endocrinology 149, 4988–4996 (2008)
U. Heider, I. Pedal, K. Spanel-Borowski, Increase in nerve fibers and loss of mast cells in polycystic and postmenopausal ovaries. Fertil. Steril. 75, 1141–1147 (2001)
M. Greiner, A. Paredes, V. Araya, H.E. Lara, Role of stress and sympathetic innervation in the development of polycystic ovary syndrome. Endocrine 28, 319–324 (2005)
C.A. Dyer, G.F. Erickson, Norepinephrine amplifies human chorionic gonadotropin-stimulated androgen biosynthesis by ovarian theca-interstitial cells. Endocrinology 116, 1645–1652 (1985)
F. Zangeneh, R. Salman Yazdi, M.M. Naghizadeh, N. Abedinia, Effect of Ramadan fasting on stress neurohormones in women with polycystic ovary syndrome. J. Fam. Reprod. Health 9, 51–57 (2015)
S. Shorakae, E.A. Lambert, E. Jona, C. Ika Sari, B. de Courten, J.B. Dixon, G.W. Lambert, H.J. Teede, Effect of central sympathoinhibition with moxonidine on sympathetic nervous activity in polycystic ovary syndrome-a randomized controlled trial. Front. Physiol. 9, 1486 (2018)
U. Otten, M. Schwab, C. Gagnon, H. Thoenen, Selective induction of tyrosine hydroxylase and dopamine beta-hydroxylase by nerve growth factor: comparison between adrenal medulla and sympathetic ganglia of adult and newborn rats. Brain Res. 133, 291–303 (1977)
Y. Furukawa, S. Furukawa, E. Satoyoshi, K. Hayashi, Catecholamines induce an increase in nerve growth factor content in the medium of mouse L-M cells. J. Biol. Chem. 261(13), 6039–6047 (1986)
J.L. Wilson, W. Chen, G.A. Dissen, S.R. Ojeda, M.A. Cowley, C. Garcia-Rudaz, P.J. Enriori, Excess of nerve growth factor in the ovary causes a polycystic ovary-like syndrome in mice, which closely resembles both reproductive and metabolic aspects of the human syndrome. Endocrinology 155, 4494–4506 (2014)
G.A. Dissen, H.E. Lara, V. Leyton, A. Paredes, D.F. Hill, M.E. Costa, A. Martinez-Serrano, S.R. Ojeda, Intraovarian excess of nerve growth factor increases androgen secretion and disrupts estrous cyclicity in the rat. Endocrinology 141, 1073–1082 (2000)
H.E. Lara, G.A. Dissen, V. Leyton, A. Paredes, H. Fuenzalida, J.L. Fiedler, S.R. Ojeda, An increased intraovarian synthesis of nerve growth factor and its low affinity receptor is a principal component of steroid-induced polycystic ovary in the rat. Endocrinology 141, 1059–1072 (2000)
A. Benitez, R. Riquelme, M. Del Campo, C. Araya, H.E. Lara, Nerve growth factor: a dual activator of noradrenergic and cholinergic systems of the rat ovary. Front. Endocrinol. 12, 636600 (2021)
A.V. Roland, S.M. Moenter, Reproductive neuroendocrine dysfunction in polycystic ovary syndrome: insight from animal models. Front. Neuroendocrinol. 35, 494–511 (2014)
G.A. Dissen, C. Garcia-Rudaz, A. Paredes, C. Mayer, A. Mayerhofer, S.R. Ojeda, Excessive ovarian production of nerve growth factor facilitates development of cystic ovarian morphology in mice and is a feature of polycystic ovarian syndrome in humans. Endocrinology 150, 2906–2914 (2009)
F.A. Gulino, E. Giuffrida, E. Leonardi, I. Marilli, M.A. Palumbo, Intrafollicular nerve growth factor concentration in patients with polycystic ovary syndrome: a case-control study. Minerva Ginecol. 68, 110–116 (2016)
E. Buyuk, D.B. Seifer, Follicular-fluid neurotrophin levels in women undergoing assisted reproductive technology for different etiologies of infertility. Fertil. Steril. 90, 1611–1615 (2008)
F.Z. Zangeneh, M.M. Naghizadeh, M. Bagheri, M. Jafarabadi, Are CRH & NGF as psychoneuroimmune regulators in women with polycystic ovary syndrome?. Gynecol. Endocrinol. 33, 227–233 (2017)
Y.W. Chen, P.Y. Lin, K.Y. Tu, Y.S. Cheng, C.K. Wu, P.T. Tseng, Significantly lower nerve growth factor levels in patients with major depressive disorder than in healthy subjects: a meta-analysis and systematic review. Neuropsychiatr. Dis. Treat. 11, 925–933 (2015)
K.L. Rooney, A.D. Domar, The relationship between stress and infertility. Dialogues Clin. Neurosci. 20, 41–47 (2018)
R.A. Carrasco, J. Singh, G.P. Adams, The relationship between gonadotropin releasing hormone and ovulation inducing factor/nerve growth factor receptors in the hypothalamus of the llama. Reprod. Biol. Endocrinol. 31(16), 83 (2018)
G. Gajardo, L. Paiva, C. Ulloa-Leal, X. Valderrama, G. López, A. Carrasco, A.I. Hidalgo, M.E. Silva, P.I. Palma, M.H. Ratto, Administration of beta-nerve growth factor during the preovulatory stage improves endocrine and luteal function in dairy heifers. Animals 9(13), 1004 (2023)
C. Missale, F. Boroni, S. Sigala, A. Buriani, M. Fabris, A. Leon, R. Dal Toso, P. Spano, Nerve growth factor in the anterior pituitary: localization in mammotroph cells and cosecretion with prolactin by a dopamine-regulated mechanism. Proc. Natl Acad. Sci. USA. 93, 4240–4245 (1996)
M.R. Peeraully, J.R. Jenkins, P. Trayhurn, NGF gene expression and secretion in white adipose tissue: regulation in 3T3-L1 adipocytes by hormones and inflammatory cytokines. Am. J. Physiol. Endocrinol. Metab. 287, E331–E339 (2004)
I. Hernández, A. Parra, I. Méndez, V. Cabrera, M.C. Cravioto, M. Mercado, V. Díaz-Sánchez, F. Larrea, Hypothalamic dopaminergic tone and prolactin bioactivity in women with polycystic ovary syndrome. Arch. Med. Res. 31, 216–222 (2000)
A. Velardo, M. Pantaleoni, C. Zironi, G. Zizzo, P. Marrama, Evidence of altered dopaminergic modulation of prolactin and thyrotropin secretion in patients with polycystic ovary syndrome. Horm. Res. 35, 4–7 (1991)
M. Saei Ghare Naz, M. Mousavi, F. Mahboobifard, A. Niknam, F. Ramezani Tehrani, A meta-analysis of observational studies on prolactin levels in women with polycystic ovary syndrome. Diagnostics 12, 2924 (2022)
M. Bulló, M.R. Peeraully, P. Trayhurn, J. Folch, J. Salas-Salvadó, Circulating nerve growth factor levels in relation to obesity and the metabolic syndrome in women. Eur. J. Endocrinol. 157, 303–310 (2007)
G.N. Chaldakov, M. Fiore, I.S. Stankulov, M. Hristova, A. Antonelli, L. Manni, P.I. Ghenev, F. Angelucci, L. Aloe, NGF, BDNF, leptin, and mast cells in human coronary atherosclerosis and metabolic syndrome. Arch. Physiol. Biochem. 109, 357–360 (2001)
J. Samario-Román, C. Larqué, P. Pánico, R.I. Ortiz-Huidobro, M. Velasco, R. Escalona, M. Hiriart, NGF and its role in immunoendocrine communication during metabolic syndrome. Int. J. Mol. Sci. 24, 1957 (2023)
M.M. Smith, C.T. Minson, Obesity and adipokines: effects on sympathetic overactivity. J. Physiol. 590, 1787–1801 (2012)
G.R. Moran, The catalytic function of renalase: a decade of phantoms. Biochim. Biophys. Acta 1864, 177–186 (2016)
J. Czubilińska-Łada, A. Gliwińska, A. Badeński, M. Szczepańska, Associations between renalase concentration and the occurrence of selected diseases. Endokrynol. Pol. 71, 334–342 (2020)
A. Vijayakumar, N.R. Mahapatra, Renalase: a novel regulator of cardiometabolic and renal diseases. Hypertens. Res. 45, 1582–1598 (2022)
Y. Wu, J. Xu, H. Velazquez, P. Wang, G. Li, D. Liu, B. Sampaio-Maia, J. Quelhas-Santos, K. Russell, R. Russell, R.A. Flavell, M. Pestana, F. Giordano, G.V. Desir, Renalase deficiency aggravates ischemic myocardial damage. Kidney Int. 79, 853–860 (2011)
E. Zbroch, D. Musialowska, E. Koc-Zorawska, J. Malyszko, Age influence on renalase and catecholamines concentration in hypertensive patients, including maintained dialysis. Clin. Interv. Aging 11, 1545–1550 (2016)
H. Akbari, G. Asadikaram, S. Vakili, M. Masoumi, Atorvastatin and losartan may upregulate renalase activity in hypertension but not coronary artery diseases: the role of gene polymorphism. J. Cell Biochem. 120, 9159–9171 (2019)
X. Li, Q. Huang, J. Xu, Renalase gene polymorphisms and plasma levels are associated with preeclampsia: a hospital-based study in the Chinese cohort. Women Health 61, 957–967 (2021)
M. Lemiesz, E. Tenderenda-Banasiuk, D. Sosnowska, K. Taranta-Janusz, A. Wasilewska, Serum renalase levels in adolescents with primary hypertension. Pediatr. Cardiol. 39, 1258–1264 (2018)
M. Zhou, T. Liang, Y. Wang, D. Jin, J. Wang, L. Jia, S. Zhang, Expression and tissue localization of renalase, a novel soluble FAD-dependent protein, in reproductive/steroidogenic systems. Mol. Biol. Rep. 40, 3987–3994 (2013)
S.S. Fatima, R. Rehman, R.S. Martins, F. Alam, M. Ashraf, Single nucleotide polymorphisms in Renalase and KCNQ1 genes and female infertility: a cross-sectional study in Pakistan. Andrologia 51, e13434 (2019)
C.P. Kovesdy, S.L. Furth, C. Zoccali; World Kidney Day Steering Committee, Obesity and kidney disease: hidden consequences of the epidemic. Can. J. Kidney Health Dis. 4, 2054358117698669 (2017)
J. Finsterer, Mitochondrial dysfunction in polycystic ovary syndrome. Reprod. Sci. 30, 1435–1442 (2023)
S. Patlolla, S. Vaikkakara, A. Sachan, A. Venkatanarasu, B. Bachimanchi, A. Bitla, S. Settipalli, S. Pathiputturu, R.N. Sugali, S. Chiri, Heterogenous origins of hyperandrogenism in the polycystic ovary syndrome in relation to body mass index and insulin resistance. Gynecol. Endocrinol. 34, 238–242 (2018)
M. Manchia, A.W. Gathier, H. Yapici-Eser, M.V. Schmidt, D. de Quervain, T. van Amelsvoort, J.I. Bisson, J.F. Cryan, O.D. Howes, L. Pinto, N.J. van der Wee, K. Domschke, I. Branchi, C.H. Vinkers, The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: a critical review across waves. Eur. Neuropsychopharmacol. 55, 22–83 (2022)
Funding
This work was supported by the Medical University-Sofia (GRANT 2021, N7873/18.11.2020, D-120/04.06.2021).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Ralitsa Robeva, Atanaska Elenkova, and Georgi Kirilov. The first draft of the manuscript was written by Ralitsa Robeva and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Medical University—Sofia (26.05.2021/Protocol №16).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Robeva, R., Elenkova, A., Kirilov, G. et al. Plasma-free metanephrines, nerve growth factor, and renalase significance in patients with PCOS. Endocrine 81, 602–612 (2023). https://doi.org/10.1007/s12020-023-03404-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03404-9