Abstract
Purpose
To evaluate the accuracy of the uterine artery pulsatility index (PI) for the diagnosis of pubertal onset in girls.
Methods
Cross-sectional study of girls with normal pubertal development. Puberty was diagnosed by the presence of Tanner breast development score ≥2. All girls underwent pelvic ultrasound and Doppler imaging of the uterine arteries. We evaluated the uterine artery PI and uterine, endometrial, and ovarian measurements. We used ROC curves with cutoffs determined by Youden index for data analysis.
Results
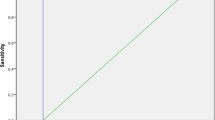
We included 169 girls aged 5–16 years who underwent 202 pelvic ultrasound examinations. Prepubertal girls had a significantly higher mean PI (6.70 ± 2.15) than girls in initial puberty (4.14 ± 1.55) and in late puberty (2.81 ± 1.05) (P < 0.001 for all comparisons), which reflects a progressive increase in blood flow to the uterus with the progression of puberty. ROC curve analysis showed that the PI was able to identify the onset of puberty with a mean area under the curve of 0.838 ± 0.04 (P < 0.001), and the PI cutoff point of 5.05 had a sensitivity of 77%, specificity of 85%, positive predictive value (PPV) of 92%, and accuracy of 79%. The combination of PI < 5.05 plus uterine volume >3.75 cm³ had a sensitivity of 73%, specificity of 95%, PPV of 97%, and accuracy of 79% to detect initial puberty.
Conclusions
We found a significant reduction in the PI during pubertal development, which can possibly be a valuable noninvasive tool in the evaluation of pubertal disorders, alone or in combination with uterine and ovarian volumes.




Similar content being viewed by others
Data availability
Data and material are available from the authors upon request.
References
F. Ziereisen, G. Guissard, N. Damry, E.F. Avni, Sonographic imaging of the paediatric female pelvis. Eur. Radiol. 15, 1296–1309 (2005).
L. de Vries, M. Phillip, Role of pelvic ultrasound in girls with precocious puberty. Horm. Res. Paediatr. 75, 148–152 (2011).
L. Garel, J. Dubois, A. Grignon, D. Filiatrault, G. Van Vliet, US of the pediatric female pelvis: a clinical perspective. Radiographics 21, 1393–1407 (2001).
C. Asăvoaie, O. Fufezan, M. Coşarcă, Ovarian and uterine ultrasonography in pediatric patients. Pictorial essay. Med. Ultrason. 16, 160–167 (2014).
E. Mosfeldt Laursen, K. Holm, V. Brocks, M. Jarden, J. Müller, Doppler assessment of flow velocity in the uterine artery during pubertal maturation. Ultrasound Obstet. Gynecol. 8, 341–345 (1996).
M.G. Long, J.E. Boultbee, M.E. Hanson, R.H. Begent, Doppler time velocity waveform studies of the uterine artery and uterus. Br. J. Obstet. Gynaecol. 96, 588–593 (1989).
F. Ziereisen, C. Heinrichs, D. Dufour, M. Saerens, E.F. Avni, The role of Doppler evaluation of the uterine artery in girls around puberty. Pediatr. Radiol. 31, 712–719 (2001).
R. Golestani, M. Sheikhvatan, A.M. Behpour, M. Mehdizadeh, A.A. Hajiashrafi, Relationship between uterine and ovarian arterial blood flow measured by Doppler sonography at different stages of puberty. Taiwan J. Obstet. Gynecol. 47, 62–65 (2008).
P.L. Paesano, C. Colantoni, S. Mora et al. Validation of an accurate and noninvasive tool to exclude female precocious puberty: pelvic ultrasound with uterine artery pulsatility index. AJR Am. J. Roentgenol. 213, 451–457 (2019).
J.F. Cohen, D.A. Korevaar, D.G. Altman et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open 6, e012799 (2016).
W.A. Marshall, J.M. Tanner, Variations in pattern of puberal changes in girls. Arch. Dis. Child. 44, 291–303 (1969).
M. de Onis, A.W. Onyango, E. Borghi et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health. Organ. 85, 660–667 (2007).
J.M. Tanner, H. Goldstein, R.H. Whitehouse, Standards for children’s height at ages 2-9 years allowing for heights of parents. Arch. Dis. Child. 45, 755–762 (1970).
W.J. Youden, Index for rating diagnostic tests. Cancer 3, 32–35 (1950).
E.S. Venkatraman, C.B. Begg, A distribution-free procedure for comparing receiver operating characteristic curves from a paired experiment. Biometrika 83, 835–848 (1996)
R.B. Borges et al. Power and sample size for health researchers. Clin. Biomed. Res. (2020) https://hcpa-unidade-bioestatistica.shinyapps.io/PSS_Health/
M. Perrot-Applanat, M.T. Groyer-Picard, E. Garcia, F. Lorenzo, E. Milgrom, Immunocytochemical demonstration of estrogen and progesterone receptors in muscle cells of uterine arteries in rabbits and humans. Endocrinology 123, 1511–1519 (1988).
D. de Ziegler, R. Bessis, R. Frydman, Vascular resistance of uterine arteries: physiological effects of estradiol and progesterone. Fertil. Steril. 55, 775–779 (1991)
R.R. Shankar, G.J. Eckert, C. Saha, W. Tu, J.H. Pratt, The change in blood pressure during pubertal growth. J. Clin. Endocrinol. Metab. 90, 163–167 (2005).
C. Battaglia, F. Mancini, G. Regnani, N. Persico, L. Iughetti, D. De Aloysio, Pelvic ultrasound and color Doppler findings in different isosexual precocities. Ultrasound Obstet. Gynecol. 22, 277–283 (2003).
E.F. Schisterman, N. Perkins, Confidence intervals for the Youden index and corresponding optimal cut-point. Commun. Stat. B Simul. Comput. 36, 549–563 (2007).
L. de Vries, G. Horev, M. Schwartz, M. Phillip, Ultrasonographic and clinical parameters for early differentiation between precocious puberty and premature thelarche. Eur. J. Endocrinol. 154, 891–898 (2006).
X. Wen, D. Wen, H. Zhang, H. Zhang, Y. Yang, Observational study pelvic ultrasound a useful tool in the diagnosis and differentiation of precocious puberty in Chinese girls. Medicine 97, e0092 (2018).
L.D. Herter, E. Golendziner, J.A. Flores et al. Ovarian and uterine findings in pelvic sonography: comparison between prepubertal girls, girls with isolated thelarche, and girls with central precocious puberty. J. Ultrasound Med. 21, 1237–1246 (2002).
M. Badouraki, A. Christoforidis, I. Economou, A.S. Dimitriadis, G. Katzos, Evaluation of pelvic ultrasonography in the diagnosis and differentiation of various forms of sexual precocity in girls. Ultrasound Obstet. Gynecol. 32, 819–827 (2008).
F. Buzi, A. Pilotta, D. Dordoni, A. Lombardi, S. Zaglio, P. Adlard, Pelvic ultrasonography in normal girls and in girls with pubertal precocity. Acta. Paediatr. 87, 1138–1145 (1998).
H.P. Haber, H.A. Wollmann, M.B. Ranke, Pelvic ultrasonography: early differentiation between isolated premature thelarche and central precocious puberty. Eur. J. Pediatr. 154, 182–186 (1995).
Acknowledgements
Hospital de Clínicas de Porto Alegre Research and Events Support Fund and Universidade Federal do Rio Grande do Sul Medical Science Program: Endocrinology.
Funding
This work was supported by grants from Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (FAPERGS), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Programa de Apoio a Núcleos de Excelência (PRONEX process number 16/2551-0000-476-5), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), and Fundo de Incentivo à Pesquisa e Eventos (FIPE) Hospital de Clínicas de Porto Alegre.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The study protocol was approved by the Hospital de Clínicas de Porto Alegre Research Ethics Committee (GPPG number 2019-0468).
Informed consent
The researchers signed a term of commitment for the use of data collected from medical records. They also agreed that this information would be used solely and exclusively for the execution of this project. The pediatric endocrinologists have signed a document authorizing the use of data from their patients’ medical records. Written informed consent was waived by the Institutional Review Board because of the retrospective nature of the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Cheuiche, A.V., da Silveira, L.G., Escott, G.M. et al. Accuracy of Doppler assessment of the uterine arteries in healthy girls for the diagnosis of pubertal onset. Endocrine 76, 172–178 (2022). https://doi.org/10.1007/s12020-021-02948-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02948-y