Abstract
Objective
To explore the relationship between triglyceride (TG) levels and aggressive pathological characteristics in papillary thyroid microcarcinoma (PTMC) patients, especially the relationship between TG, BMI, age, and extrathyroidal extension (ETE).
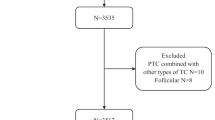
Methods
A retrospective analysis of 9663 patients with PTMC in a single center from 2010 to 2017 was included in this study. Binary logistic regression was used to analyze the relationship between serum TG and aggressive pathological characteristics of PTMC in different genders. Further analyzing the risk of high TG in different ages and BMI groups.
Results
Even after adjustment for confounding factors, high TG is still a risk factor for ETE in women with PTMC, but not a risk factor for men. Compared with the group with lower than 0.90 mmol/L, when the TG level is higher than 1.93 mmol/L, the risk of ETE in women increased by about 1.35-fold. The remaining two variables (BMI, age) as risk factors for ETE are analyzed. In the normal BMI group, high TG is still a risk factor for ETE. The risk of ETE in women more than 55 years old is significantly increased by 1.96-fold (1.34-fold in less than 55 years).
Conclusion
High TG in women is positively correlated with the risk of ETE in PTMC. PTMC with high TG in elderly women (more than 55 years) has a higher risk of ETE. TG is a potential serological index for predicting the risk of ETE in women with normal BMI.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Y. Ito, A. Miyauchi, T. Kudo, H. Oda, M. Yamamoto, H. Sasai et al. Trends in the implementation of active surveillance for low-risk papillary thyroid microcarcinomas at Kuma Hospital: gradual increase and heterogeneity in the acceptance of this new management option. Thyroid 28(4), 488–95 (2018). https://doi.org/10.1089/thy.2017.0448
H. Kwon, H.-S. Oh, M. Kim, S. Park, M.J. Jeon, W.G. Kim et al. Active surveillance for patients with papillary thyroid microcarcinoma: a single center’s experience in Korea. J. Clin. Endocrinol. Metab. 102(6), 1917–25 (2017). https://doi.org/10.1210/jc.2016-4026
Q. Zhao, J. Ming, C. Liu, L. Shi, X. Xu, X. Nie et al. Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma. Ann. surgical Oncol. 20(3), 746–52 (2013). https://doi.org/10.1245/s10434-012-2654-2
L. Davies, H.G. Welch, Current thyroid cancer trends in the United States. JAMA Otolaryngol. Head. Neck Surg. 140(4), 317–22 (2014). https://doi.org/10.1001/jamaoto.2014.1
L.G.T. Morris, A.G. Sikora, T.D. Tosteson, L. Davies, The increasing incidence of thyroid cancer: the influence of access to care. Thyroid 23(7), 885–91 (2013). https://doi.org/10.1089/thy.2013.0045
K.-L. Lin, O.-C. Wang, X.-H. Zhang, X.-X. Dai, X.-Q. Hu, J.-M. Qu, The BRAF mutation is predictive of aggressive clinicopathological characteristics in papillary thyroid microcarcinoma. Ann. surgical Oncol. 17(12), 3294–300 (2010). https://doi.org/10.1245/s10434-010-1129-6
M. Yun, T.-W. Noh, A. Cho, Y.-J. Choi, S.-W. Hong, C.-S. Park et al. Visually discernible [18F]fluorodeoxyglucose uptake in papillary thyroid microcarcinoma: a potential new risk factor. J. Clin. Endocrinol. Metab. 95(7), 3182–8 (2010). https://doi.org/10.1210/jc.2009-2091
I. Sugitani, Y. Ito, D. Takeuchi, H. Nakayama, C. Masaki, H. Shindo, et al. Indications and strategy for active surveillance of adult low-risk papillary thyroid microcarcinoma: consensus statements from the Japan Association of Endocrine Surgery Task Force on management for papillary thyroid microcarcinoma. Thyroid 2020. https://doi.org/10.1089/thy.2020.0330.
S.-M. Chow, S.C.K. Law, J.K.C. Chan, S.-K. Au, S. Yau, W.-H. Lau, Papillary microcarcinoma of the thyroid-Prognostic significance of lymph node metastasis and multifocality. Cancer 98(1), 31–40 (2003)
J.-S. Pyo, J.H. Sohn, G. Kang, Detection of tumor multifocality is important for prediction of tumor recurrence in papillary thyroid microcarcinoma: a retrospective study and meta-analysis. J. Pathol. Transl. Med. 50(4), 278–86 (2016). https://doi.org/10.4132/jptm.2016.03.29
J.C. Riss, I. Peyrottes, E. Chamorey, J. Haudebourg, A. Sudaka, D. Benisvy et al. Prognostic impact of tumour multifocality in thyroid papillary microcarcinoma based on a series of 160 cases. Eur. Ann. Otorhinolaryngol. Head. Neck Dis. 129(4), 175–8 (2012). https://doi.org/10.1016/j.anorl.2011.11.003
Y.K. So, M.W. Kim, Y.-I. Son, Multifocality and bilaterality of papillary thyroid microcarcinoma. Clin. Exp. Otorhinolaryngol. 8(2), 174–8 (2015). https://doi.org/10.3342/ceo.2015.8.2.174
H. Shimano, Novel qualitative aspects of tissue fatty acids related to metabolic regulation: lessons from Elovl6 knockout. Prog. Lipid Res 51(3), 267–71 (2012). https://doi.org/10.1016/j.plipres.2011.12.004
D. Janković, P. Wolf, C.-H. Anderwald, Y. Winhofer, M. Promintzer-Schifferl, A. Hofer et al. Prevalence of endocrine disorders in morbidly obese patients and the effects of bariatric surgery on endocrine and metabolic parameters. Obes. Surg. 22(1), 62–9 (2012). https://doi.org/10.1007/s11695-011-0545-4
M. Zhao, X. Zhang, L. Gao, Y. Song, C. Xu, C. Yu et al. Palmitic acid downregulates thyroglobulin (TG), sodium iodide symporter (NIS), and thyroperoxidase (TPO) in human primary thyrocytes: a potential mechanism by which lipotoxicity affects thyroid? Int. J. Endocrinol. 2018, 4215848 (2018). https://doi.org/10.1155/2018/4215848
M. Zhao, X. Tang, T. Yang, B. Zhang, Q. Guan, S. Shao et al. Lipotoxicity, a potential risk factor for the increasing prevalence of subclinical hypothyroidism?. J. Clin. Endocrinol. Metab. 100(5), 1887–94 (2015). https://doi.org/10.1210/jc.2014-3987
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP), Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 285(19), 2486–97 (2001)
D.S. Cooper, B. Biondi, Subclinical thyroid disease. Lancet (Lond., Engl.) 379(9821), 1142–54 (2012). https://doi.org/10.1016/S0140-6736(11)60276-6
J.R. Garber, R.H. Cobin, H. Gharib, J.V. Hennessey, I. Klein, J.I. Mechanick et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid 22(12), 1200–35 (2012). https://doi.org/10.1089/thy.2012.0205
M.P.J. Vanderpump, Should we treat mild subclinical/mild hyperthyroidism? No. Eur. J. Intern. Med. 22(4), 330–3 (2011). https://doi.org/10.1016/j.ejim.2011.03.009
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series. 894:i–xii, 1–253 (2000). Epub 2001/03/10.
B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1) (2016). https://doi.org/10.1089/thy.2015.0020
C. Tomoda, T. Uruno, Y. Takamura, Y. Ito, A. Miya, K. Kobayashi et al. Ultrasonography as a method of screening for tracheal invasion by papillary thyroid cancer. Surg. today 35(10), 819–22 (2005)
K. Shimamoto, H. Satake, A. Sawaki, T. Ishigaki, H. Funahashi, T. Imai. Preoperative staging of thyroid papillary carcinoma with ultrasonography. Eur. J. Radiol. 29(1) (1998).
J.Y. Kwak, E.-K. Kim, J.H. Youk, M.J. Kim, E.J. Son, S.H. Choi et al. Extrathyroid extension of well-differentiated papillary thyroid microcarcinoma on US. Thyroid 18(6), 609–14 (2008). https://doi.org/10.1089/thy.2007.0345
C.Y. Lee, S.J. Kim, K.R. Ko, K.-W. Chung, J.-H. Lee, Predictive factors for extrathyroidal extension of papillary thyroid carcinoma based on preoperative sonography. J. Ultrasound Med. 33(2), 231–8 (2014). https://doi.org/10.7863/ultra.33.2.231
A. Kamaya, A.M. Tahvildari, B.N. Patel, J.K. Willmann, R.B. Jeffrey, T.S. Desser, Sonographic detection of extracapsular extension in papillary thyroid cancer. J. Ultrasound Med. 34(12), 2225–30 (2015). https://doi.org/10.7863/ultra.15.02006
Z. Al-Qurayshi, N. Nilubol, R.P. Tufano, E. Kandil, Wolf in sheep’s clothing: papillary thyroid microcarcinoma in the US. J. Am. Coll. Surg. 230(4), 484–91 (2020). https://doi.org/10.1016/j.jamcollsurg.2019.12.036
T. Diker-Cohen, D. Hirsch, I. Shimon, G. Bachar, A. Akirov, H. Duskin-Bitan, et al. Impact of minimal extra-thyroid extension in differentiated thyroid cancer: systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2018. https://doi.org/10.1210/jc.2018-00081.
J.E. Paes, K. Hua, R. Nagy, R.T. Kloos, D. Jarjoura, M.D. Ringel, The relationship between body mass index and thyroid cancer pathology features and outcomes: a clinicopathological cohort study. J. Clin. Endocrinol. Metab. 95(9), 4244–50 (2010). https://doi.org/10.1210/jc.2010-0440. Epub 2010/06/04
S.T. Yu, W. Chen, Q. Cai, F. Liang, D. Xu, P. Han et al. Pretreatment BMI is associated with aggressive clinicopathological features of papillary thyroid carcinoma: a multicenter study. Int J. Endocrinol. 2017, 5841942 (2017). https://doi.org/10.1155/2017/5841942. Epub 2017/11/01
J. Lee, C.R. Lee, C.R. Ku, S.W. Kang, J.J. Jeong, D.Y. Shin et al. Association between obesity and BRAFV600E mutation status in patients with papillary thyroid cancer. Ann. surgical Oncol. 22(Suppl 3), S683–90 (2015). https://doi.org/10.1245/s10434-015-4765-z. Epub 2015/07/29
C. Li, L. Zhou, G. Dionigi, F. Li, Y. Zhao, H. Sun. The association between tumor tissue calcification, obesity, and thyroid cancer invasiveness in a cohort study. Endocr. Pract. 2020. https://doi.org/10.4158/EP-2020-0057
H.J. Kim, N.K. Kim, J.H. Choi, S.Y. Sohn, S.W. Kim, S.M. Jin et al. Associations between body mass index and clinico-pathological characteristics of papillary thyroid cancer. Clin. Endocrinol. (Oxf.) 78(1), 134–40 (2013). https://doi.org/10.1111/j.1365-2265.2012.04506.x
C. Wu, L. Wang, W. Chen, S. Zou, A. Yang, Associations between body mass index and lymph node metastases of patients with papillary thyroid cancer: a retrospective study. Medicine (Baltimore) 96(9), e6202 (2017). https://doi.org/10.1097/MD.0000000000006202
C. Tresallet, M. Seman, F. Tissier, C. Buffet, R.M. Lupinacci, H. Vuarnesson et al. The incidence of papillary thyroid carcinoma and outcomes in operative patients according to their body mass indices. Surgery 156(5), 1145–52 (2014). https://doi.org/10.1016/j.surg.2014.04.020. Epub 2014/06/01
P. Dieringer, E.M. Klass, B. Caine, J. Smith-Gagen, Associations between body mass and papillary thyroid cancer stage and tumor size: a population-based study. J. Cancer Res. Clin. Oncol. 141(1), 93–8 (2015). https://doi.org/10.1007/s00432-014-1792-2. Epub 2014/08/13
S.H. Kim, H.S. Park, K.H. Kim, H. Yoo, B.J. Chae, J.S. Bae et al. Correlation between obesity and clinicopathological factors in patients with papillary thyroid cancer. Surg. Today 45(6), 723–9 (2015). https://doi.org/10.1007/s00595-014-0984-3. Epub 2014/07/26
C.L. Li, G. Dionigi, Y.S. Zhao, N. Liang, H. Sun. Influence of body mass index on the clinicopathological features of 13,995 papillary thyroid tumors. J. Endocrinol. Invest. 2020. https://doi.org/10.1007/s40618-020-01216-6.
Y. Ito, A. Miyauchi, M. Kihara, T. Higashiyama, K. Kobayashi, A. Miya, Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid 24(1), 27–34 (2014). https://doi.org/10.1089/thy.2013.0367
Y. Ito, A. Miyauchi, T. Kudo, T. Higashiyama, H. Masuoka, M. Kihara et al. Kinetic analysis of growth activity in enlarging papillary thyroid microcarcinomas. Thyroid 29(12), 1765–73 (2019). https://doi.org/10.1089/thy.2019.0396.
J. Zhang, R. Jiang, L. Li, P. Li, X. Li, Z. Wang et al. Serum thyrotropin is positively correlated with the metabolic syndrome components of obesity and dyslipidemia in chinese adolescents. Int. J. Endocrinol. 2014, 289503 (2014). https://doi.org/10.1155/2014/289503.
S.K. Kota, L.K. Meher, S. Krishna, K. Modi, Hypothyroidism in metabolic syndrome. Indian J. Endocrinol. Metab. 16(Suppl 2), S332–3 (2012). https://doi.org/10.4103/2230-8210.104079
Acknowledgements
Thanks to Rui Du, MS, and Chengqiu Sui, MS, for valuable suggestions in academic discussions.
Funding
This study was supported by the grant from Liaoning Provincial Science and Technology Development Program (Grant # 2017225008).
Author information
Authors and Affiliations
Contributions
Conception and design: G.D., H.S., H.G.; administrative support: H.S.; collection and assembly of data: Q.H., Y.Z.; data analysis and interpretation: C.L.; manuscript writing: C.L. Final approval of manuscript: all authors.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Ethics Approval
The Institutional Review Board of China–Japan Union Hospital of Jilin University, Changchun, China, approved the protocol (Grant # 2019040806).
Consent to Participate
All patients had provided signed informed consent.
Consent for Publication
All authors are in agreement with the content of the manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Li, C., Guan, H., He, Q. et al. The relationship between lipotoxicity and risk of extrathyroidal extension in papillary thyroid microcarcinoma. Endocrine 74, 646–657 (2021). https://doi.org/10.1007/s12020-021-02809-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02809-8