Abstract
Introduction
Juvenile primary hyperparathyroidism is uncommon and more symptomatic than the adult counterpart. The aim of this prospective monocentric study, conducted in a tertiary referral center, was to evaluate the clinical, biochemical, and densitometric data, and the outcome of a series of patients with juvenile primary hyperparathyroidism.
Material and Methods
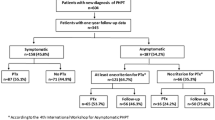
The study group included 154 patients with sporadic and familial juvenile primary hyperparathyroidism, aged ≤40 years. Relative frequency of sporadic and familial forms, comparison of the clinical and biochemical characteristics, rate of cure after parathyroidectomy and the outcome of patients not undergoing surgery were evaluated.
Results
Familial cases (n = 42) were younger, less frequently females, and had milder disease compared to sporadic cases (n = 112). No difference was observed in biochemical and densitometric parameters. Among patients undergoing parathyroidectomy (n = 116), familial cases had a higher rate of multigland disease and a higher persistence/relapse rate compared to sporadic cases (73 vs. 3.6% and 48.1 vs. 5.7%, respectively). Patients who did not undergo parathyroidectomy had stable clinical, biochemical, and densitometric parameters during follow-up (median 27 months). Using the cut-off age of 25 years, there was no difference in clinical, biochemical and densitometric parameters between younger and older patients, with the exception of parathyroid hormone and phosphate, which were significantly lower and higher, respectively, in patients <25 years.
Conclusions
In conclusion, this prospective study shows that juvenile primary hyperparathyroidism is frequently a sporadic disease, with no difference in the biochemical phenotype between sporadic and familial forms. Patients with familial juvenile primary hyperparathyroidism have a milder clinical phenotype and higher rate of persistence/recurrence after PTx than those with sporadic juvenile primary hyperparathyroidism.

Similar content being viewed by others
References
J.P. Bilezikian, M.L. Brandi, R. Eastell, S.J. Silverberg, R. Udelsman, C. Marcocci, J.T. Potts, Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the fourth international workshop. J. Clin. Endocrinol. Metab. 99, 3561–3569 (2014)
C. Marcocci, F. Cetani, Clinical practice. Primary hyperparathyroidism. N. Engl. J. Med. 365, 2389–2397 (2011)
N. Yu, P.T. Donnan, M.J. Murphy, G.P. Leese, Epidemiology of primary hyperparathyroidism in Tayside, Scotland, UK. Clin. Endocrinol. 71, 485–493 (2009)
A. Abood, P. Vestergaard, Increasing incidence of primary hyperparathyroidism in Denmark. Dan. Med. J. 60, A4567 (2013)
J. Roizen, M.A. Levine, Primary hyperparathyroidism in children and adolescents. J. Chin. Med. Assoc. 75, 425–434 (2012)
M. Allo, N.W. Thompson, J.K. Harness, R.H. Nishiyama, Primary hyperparathyroidism in children, adolescents, and young adults. World J. Surg. 6, 771–776 (1982)
C.S. Cronin, T.S. Reeve, B. Robinson, P. Clifton-Bligh, A. Guinea, L. Delbridge, Primary hyperparathyroidism in childhood and adolescence. J. Paediatr. Child Health 32, 397–399 (1996)
E. Kandil, D.S. Majid, K.A. Carson, R.P. Tufano, A comparison of outcomes for younger and older adult patients undergoing surgery for primary hyperparathyroidism. Ann. Surg. Oncol. 19, 1897–1901 (2012)
M.L. Lawson, S.F. Miller, G. Ellis, R.M. Filler, S.W. Kooh, Primary hyperparathyroidism in a paediatric hospital. QJM 89, 921–32 (1996)
K.C. Loh, Q.Y. Duh, D. Shoback, L. Gee, A. Siperstein, O.H. Clark, Clinical profile of primary hyperparathyroidism in adolescents and young adults. Clin. Endocrinol. 48, 435–443 (1998)
S.C. Hsu, M.A. Levine, Primary hyperparathyroidism in children and adolescents: the Johns Hopkins Children’s Center experience 1984–2001. J Bone Miner. Res. 17(Suppl 2), N44–50 (2002)
J. Kollars, A.E. Zarroug, J. van Heerden, A. Lteif, P. Stavlo, L. Suarez, C. Moir, M. Ishitani, D. Rodeberg, Primary hyperparathyroidism in pediatric patients. Pediatrics 115, 974–980 (2005)
E. Mallet, B. Amrein, C. Bost, D. David, F. Despert, G. Garabedian, L. Guillot, L. Lienhardt, L. Loirat, P. Nicolino, S. Simonin, T. Thieuleux, Y. Wagner, Primary hyperparathyroidism in neonates and childhood: The French experience (1984–2004). Horm. Res. 69, 180–188 (2008)
V.N. Shah, S.K. Bhadada, A. Bhansali, A. Behera, B.R. Mittal, V. Bhavin, Influence of age and gender on presentation of symptomatic primary hyperparathyroidism. J. Postgrad. Med. 58, 107–111 (2012)
J. George, S.V. Acharya, T.R. Bandgar, P.S. Menon, N.S. Shah, Primary hyperparathyroidism in children and adolescents. Indian J. Pediatr. 77, 175–178 (2010)
E.T. Durkin, P.F. Nichol, D.P. Lund, H. Chen, R.S. Sippel, What is the optimal treatment for children with primary hyperparathyroidism? J. Pediatr. Surg. 45, 1142–1146 (2010)
J.F. Burke, K. Jacobson, A. Gosain, R.S. Sippel, H. Chen, Radioguided parathyroidectomy effective in pediatric patients. J. Surg. Res. 184, 312–317 (2013)
I. Paunovic, V. Zivaljevic, R. Stojanic, N. Kalezic, M. Kazic, A. Diklic, Primary hyperparathyroidism in children and young adults: a single institution experience. Acta Chir. Belg. 113, 35–39 (2013)
J. Roizen, M.A. Levine, A meta-analysis comparing the biochemistry of primary hyperparathyroidism in youths to the biochemistry of primary hyperparathyroidism in adults. J. Clin. Endocrinol. Metab. 99, 4555–4564 (2014)
J.P. Bilezikian, C.S. Kovacs, The parathyroids Section II, Chapter 23, AP Editor (2015)
Y.H. Chou, E.M. Brown, T. Levi, G. Crowe, A.B. Atkinson, H.J. Arnqvist, G. Toss, G.E. Fuleihan, J.G. Seidman, C.E. Seidman, The gene responsible for familial hypocalciuric hypercalcemia maps to chromosome 3q in four unrelated families. Nat. Genet. 1, 295–300 (1992)
A. Szalat, S. Shpitzen, A. Tsur, I. Zalmon Koren, S. Shilo, L. Tripto-Shkolnik, R. Durst, E. Leitersdorf, V. Meiner, Stepwise CaSR, AP2S1, and GNA11 sequencing in patients with suspected familial hypocalciuric hypercalcemia. Endocrine 55(3), 741–747 (2017)
R.V. Thakker, P.J. Newey, G.V. Walls, J. Bilezikian, H. Dralle, P.R. Ebeling, S. Melmed, A. Sakurai, F. Tonelli, M.L. Brandi, Clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1). J. Clin. Endocrinol. Metab. 97, 2990–3011 (2012)
F. Cetani, E. Pardi, S. Borsari, M. Tonacchera, E. Morabito, A. Pinchera, C. Marcocci, Two Italian kindreds with familial hypocalciuric hypercalcaemia caused by loss-of-function mutations in the calcium-sensing receptor (CaR) gene: functional characterization of a novel CaR missense mutation. Clin. Endocrinol. 58, 199–206 (2003)
G. Viccica, F. Cetani, E. Vignali, M. Miccoli, C. Marcocci, Impact of vitamin D deficiency on the clinical and biochemical phenotype in women with sporadic primary hyperparathyroidism. Endocrine 25, (2016). doi:10.1007/s12020-016-0931-8
E. Vignali, A. Picone, G. Materazzi, S. Steffe, P. Berti, L. Cianferotti, F. Cetani, E. Ambrogini, P. Miccoli, A. Pinchera, C. Marcocci, A quick intraoperative parathyroid hormone assay in the surgical management of patients with primary hyperparathyroidism: a study of 206 consecutive cases. Eur. J. Endocrinol. 146, 783–788 (2002)
E. Pardi, C. Marcocci, S. Borsari, F. Saponaro, L. Torregrossa, M. Tancredi, B. Raspini, F. Basolo, F. Cetani, Aryl hydrocarbon receptor interacting protein (AIP) mutations occur rarely in sporadic parathyroid adenomas. J. Clin. Endocrinol. Metab. 98, 2800–2810 (2013)
R.V. Thakker, Multiple endocrine neoplasia type 1 (MEN1) and type 4 (MEN4). Mol. Cell. Endocrinol. 386, 2–15 (2014)
R. Udelsman, G. Akerström, C. Biagini, Q.-Y. Duh, P. Miccoli, B. Niederle, F. Tonelli, The surgical management of asymptomatic primary hyperparathyroidism: proceedings of the fourth international workshop. J. Clin. Endocrinol. Metab. 99, 3595–3606 (2014)
Acknowledgements
We thank Dr. Giuseppe Viccica for his work collecting some clinical data used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Saponaro, F., Marcocci, C., Cacciatore, F. et al. Clinical profile of juvenile primary hyperparathyroidism: a prospective study. Endocrine 59, 344–352 (2018). https://doi.org/10.1007/s12020-017-1318-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-017-1318-1