Abstract
Purpose
Low plasma corticotropin is considered a useful parameter for the diagnosis of subclinical hypercortisolism in patients with an adrenal incidentaloma. However, immunoassays are vulnerable to interference from endogenous antibodies. In this study, subjects who underwent Hypothalamus-pituitary-adrenal axis evaluation for the assessment of subclinical hypercortisolism were evaluated. The objective of the study was to ascertain whether antibody interference in corticotropin immunoassay affected the diagnostic work-up and clinical decisions.
Methods
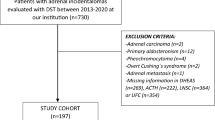
The 437 consecutive patients with incidentally discovered adrenal adenomas were included in this single centre study. Patients who had a combination of a nonsuppressed corticotropin concentration (>4.4 pmol/L) and a non-suppressed cortisol concentration after 1 mg overnight dexamethasone suppression test (>50 nmol/L) were selected. Eight eligible subjects without specific features of Cushing's syndrome were identified and recruited for interference studies and follow-up. Nine controls including one patient with unilateral adrenalectomy and one patient with Cushing's disease were recruited as well.
Measurements
Eligible subjects and controls were subjected to hormonal tests and investigations for suspected interference. Interference studies included measurement of corticotropin on a different analytical platform, serial dilutions, polyethylene glycol precipitation and heterophilic antibody analysis. Patients were followed with clinical and laboratory parameters for a median duration of 30 (12–90) months.
Results
Antibody interference was identified in four patients. Rheumatoid factor was responsible for the interference in one patient. Clinical management of the patients was affected by the erroneous results. Interference tests were negative in control subjects.
Conclusions
Erroneous results associated with analytical interference negatively impacted on clinical decision making in this patient group. This should be considered particularly in conditions such as subclinical hypercortisolism which decisions depend on laboratory investigations mainly. Analytical interference could explain the high variability observed both in field measurements from patients who were expected to have lower corticotropin concentrations and in subclinical hypercortisolism prevalence reported by different studies. Many problems can be resolved by ensuring good communication between clinical and laboratory staff.



Similar content being viewed by others
References
G. Di Dalmazi, R. Pasquali, F. Beuschlein, M. Reincke, Subclinical hypercortisolism: a state, a syndrome, or a disease? Eur. J. Endocrinol. 173, M61–M71 (2015)
M. Fassnacht, W. Arlt, I. Bancos, H. Dralle, J. Newell-Price, A. Sahdev, A. Tabarin, M. Terzolo, S. Tsagarakis, O.M. Dekkers, Management of adrenal incidentalomas: European society of endocrinology clinical practice guideline in collaboration with the european network for the study of adrenal tumors. Eur. J. Endocrinol. 175, G1–G34 (2016)
M. Terzolo, A. Stigliano, I. Chiodini, P. Loli, L. Furlani, G. Arnaldi, G. Reimondo, A. Pia, V. Toscano, M. Zini, G. Borretta, E. Papini, P. Garofalo, B. Allolio, B. Dupas, F. Mantero, A. Tabarin, Ame position statement on adrenal incidentaloma. Eur. J. Endocrinol. 164, 851–870 (2011)
I. Chiodini, Clinical review: diagnosis and treatment of subclinical hypercortisolism. J. Clin. Endocrinol. Metab. 96, 1223–1236 (2011)
L.K. Nieman, Approach to the patient with an adrenal incidentaloma. J. Clin. Endocrinol. Metab. 95, 4106–4113 (2010)
M. Debono, J. Newell-Price, Subclinical hypercortisolism in adrenal incidentaloma. Curr. Opin. Endocrinol. Diabetes Obes. 22, 185–192 (2015)
F. Pecori Giraldi, A. Saccani, F. Cavagnini, Assessment of acth assay variability: a multicenter study. Eur. J. Endocrinol. 164, 505–512 (2011)
C.M. Sturgeon, A. Viljoen, Analytical error and interference in immunoassay: minimizing risk. Ann. Clin. Biochem. 48, 418–432 (2011)
N. Bolstad, D.J. Warren, K. Nustad, Heterophilic antibody interference in immunometric assays. Best. Pract. Res. Clin. Endocrinol. Metab. 27, 647–661 (2013)
N. Bolstad, A.M. Kazaryan, M.E. Revheim, S. Distante, K. Johnsrud, D.J. Warren, K. Nustad, B. Edwin, A man with abdominal pain: enough evidence for surgery? Clin. Chem. 58, 1187–1190 (2012)
K.W. Choy, J. Teng, N. Wijeratne, C.Y. Tan, J.C. Doery, Immunoassay interference complicating management of cushing’s disease: the onus is on the clinician and the laboratory. Ann. Clin. Biochem. 54, 183–184 (2016)
J. Grasko, R. Willliams, J. Beilin, P. Glendenning, S. Fermoyle, S. Vasikaran, A diagnostic conundrum: heterophilic antibody interference in an adrenocorticotropic hormone immunoassay not detectable using a proprietary heterophile blocking reagent. Ann. Clin. Biochem. 50, 433–437 (2013)
L. Saiegh, M. Odeh, L. Chen-Konak, N. Elias, M. Sheikh-Ahmad, M. Reut, G. Slobodin, J. Bejar, C. Shechner, A possible analytical and clinical role of endogenous antibodies causing discrepant adrenocorticotropic hormone measurement in a case of ectopic cushing’s syndrome. Ann. Clin. Biochem. 51, 490–494 (2014)
A. Lacroix, R.A. Feelders, C.A. Stratakis, L.K. Nieman, Cushing’s syndrome. Lancet 386, 913–927 (2015)
A.G. Ioachimescu, E.M. Remer, A.H. Hamrahian, Adrenal incidentalomas: a disease of modern technology offering opportunities for improved patient care. Endocrinol. Metab. Clin. North. Am. 44, 335–354 (2015)
C. Invitti, F. Pecori Giraldi, M. de Martin, F. Cavagnini, Diagnosis and management of cushing’s syndrome: results of an italian multicentre study. Study group of the italian society of endocrinology on the pathophysiology of the hypothalamic-pituitary-adrenal axis. J. Clin. Endocrinol. Metab. 84, 440–448 (1999)
M. Klose, A. Kofoed-Enevoldsen, L. Ostergaard Kristensen, Single determination of plasma acth using an immunoradiometric assay with high detectability differentiates between acth-dependent and -independent cushing’s syndrome. Scand. J. Clin. Lab. Invest. 62, 33–37 (2002)
M. De Leo, A. Cozzolino, A. Colao, R. Pivonello, Subclinical cushing’s syndrome. Best. Pract. Res. Clin. Endocrinol. Metab. 26, 497–505 (2012)
O. Gulbahar, C. Konca Degertekin, M. Akturk, M.M. Yalcin, I. Kalan, G.F. Atikeler, A.E. Altinova, I. Yetkin, M. Arslan, F. Toruner, A case with immunoassay interferences in the measurement of multiple hormones. J. Clin. Endocrinol. Metab. 100, 2147–2153 (2015)
S.H. Dobson, S. Gibson, A. White, Assessment of the potency of different standards in the immunoradiometric assay of acth. Ann. Clin. Biochem. 26(Pt 1), 96–101 (1989)
J.F. Emerson, G. Ngo, S.S. Emerson, Screening for interference in immunoassays. Clin. Chem. 49, 1163–1169 (2003)
A.M. Jones, J.W. Honour, Unusual results from immunoassays and the role of the clinical endocrinologist. Clin. Endocrinol. (Oxf). 64, 234–244 (2006)
M. Fahie-Wilson, D. Halsall, Polyethylene glycol precipitation: proceed with care. Ann. Clin. Biochem. 45, 233–235 (2008)
M.N. Fahie-Wilson, R. John, A.R. Ellis, Macroprolactin; high molecular mass forms of circulating prolactin. Ann. Clin. Biochem. 42, 175–192 (2005)
N.F. Jassam, A. Paterson, C. Lippiatt, J.H. Barth, Macroprolactin on the advia centaur: experience with 409 patients over a three-year period. Ann. Clin. Biochem. 46, 501–504 (2009)
D. Cantor, Reason for limitations of heterophilic blocking tube use on certain beckman coulter access assays. Clin. Chem. 51, 1311 (2005)
K. Nishimura, D. Sugiyama, Y. Kogata, G. Tsuji, T. Nakazawa, S. Kawano, K. Saigo, A. Morinobu, M. Koshiba, K.M. Kuntz, I. Kamae, S. Kumagai, Meta-analysis: diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis. Ann. Intern. Med. 146, 797–808 (2007)
H. Raff, Update on late-night salivary cortisol for the diagnosis of cushing’s syndrome: methodological considerations. Endocrine 44, 346–349 (2013)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that they have no competing interests
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Dokuz Eylul University Research Ethics Committee approved the study
Informed consent
Informed consent was obtained from all individual participants included in the study
Additional information
Serkan Yener and Tevfik Demir contributed equally to this work.
Rights and permissions
About this article
Cite this article
Yener, S., Demir, L., Demirpence, M. et al. Interference in ACTH immunoassay negatively impacts the management of subclinical hypercortisolism. Endocrine 56, 308–316 (2017). https://doi.org/10.1007/s12020-017-1268-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-017-1268-7