Abstract
The synthetic estrogen diethylstilbestrol is used to prevent miscarriages and as a therapeutic treatment for prostate cancer, but it has been reported to have adverse effects on endocrine homeostasis. However, the toxicity mechanism is poorly understood. Recently, we reported that diethylstilbestrol impairs adrenal steroidogenesis via cholesterol insufficiency in adult male rats. In the present study, we found that the adrenal cholesterol level was significantly reduced without of the decrease in other precursors in the adrenal steroidogenesis 24 h after a single dose of diethylstilbestrol (0.33 μg/g body mass). The serum HDL/cholesterol level was also reduced only 12 h after the diethylstilbestrol exposure. The level of Apo E, which is indispensable for HDL/cholesterol maturation, was decreased in both the HDL and VLDL/LDL fractions, whereas the level of Apo A1, which is an essential constituent of HDL, was not altered in the HDL fraction. Because the liver is a major source of Apo E and Apo A1, the secretion rates of these proteins were examined using a liver perfusion experiment. The secretion rate of Apo A1 from the liver was consistent between DES-treated and control rats, but that of Apo E was comparatively suppressed in the DES-treated rats. The disruption of adrenal steroidogenesis by diethylstilbestrol was caused by a decrease in serum HDL/cholesterol, which is the main source of adrenal steroidogenesis, due to the inhibition of Apo E secretion from the liver.







Similar content being viewed by others
Abbreviations
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- VLDL:
-
Very low-density lipoprotein
- DES:
-
Diethylstilbestrol
- Apo E:
-
Apolipoprotein E
- Apo A1:
-
Apolipoprotein A1
- StAR:
-
Acute regulatory protein
- ER:
-
Estrogen receptor
- SR-B1:
-
Scavenger receptor class B type 1
- MALDI-TOF MS:
-
Matrix-assisted laser desorption ionization-time-of-flight mass spectrometry
- LC–MS:
-
Liquid chromatography–mass spectrometry
- CHAPS:
-
3-((3-cholamidopropyl)dimethylammonium)-1-propanesulfonate
References
E. Diamanti-Kandarakis, J.P. Bourguignon, L.C. Giudice, R. Hauser, G.S. Prins, A.M. Soto, R.T. Zoeller, A.C. Gore, Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr. Rev. 30, 293–342 (2009)
R. Hampl, J. Kubatova, L. Starka, Steroids and endocrine disruptors-History, recent state of art and open questions. J. Steroid Biochem. Mol. Biol. (2014). doi:10.1016/j.jsbmb.2014.04.013
O.V. Martin, T. Shialis, J.N. Lester, M.D. Scrimshaw, A.R. Boobis, N. Voulvoulis, Testicular dysgenesis syndrome and the estrogen hypothesis: a quantitative meta-analysis. Environ. Health Perspect. 116, 149–157 (2008)
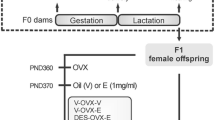
R.R. Newbold, E. Padilla-Banks, W.N. Jefferson, Adverse effects of the model environmental estrogen diethylstilbestrol are transmitted to subsequent generations. Endocrinology 147, S11–S17 (2006)
J.R. Palmer, A.L. Herbst, K.L. Noller, D.A. Boggs, R. Troisi, L. Titus-Ernstoff, E.E. Hatch, L.A. Wise, W.C. Strohsnitter, R.N. Hoover, Urogenital abnormalities in men exposed to diethylstilbestrol in utero: a cohort study. Environ. Health 8, 37 (2009)
S. Schrager, B.E. Potter, Diethylstilbestrol exposure. Am. Fam. Physician 69, 2395–2400 (2004)
J.H. Shin, T.S. Kim, I.H. Kang, T.S. Kang, H.J. Moon, S.Y. Han, Effects of postnatal administration of diethylstilbestrol on puberty and thyroid function in male rats. J Reprod Dev 55, 461–466 (2009)
T. Unuvar, A. Buyukgebiz, Fetal and neonatal endocrine disruptors. J. Clin. Res. Pediatr. Endocrinol. 4, 51–60 (2012)
R.M. Giusti, K. Iwamoto, E.E. Hatch, Diethylstilbestrol revisited: a review of the long-term health effects. Ann. Intern. Med. 122, 778–788 (1995)
D.V. Henley, K.S. Korach, Endocrine-disrupting chemicals use distinct mechanisms of action to modulate endocrine system function. Endocrinology 147, S25–S32 (2006)
K.S. Korach, J.A. McLachlan, The role of the estrogen receptor in diethylstilbestrol toxicity. Arch. Toxicol. Suppl. 8, 33–42 (1985)
G.G. Kuiper, B. Carlsson, K. Grandien, E. Enmark, J. Haggblad, S. Nilsson, J.A. Gustafsson, Comparison of the ligand binding specificity and transcript tissue distribution of estrogen receptors alpha and beta. Endocrinology 138, 863–870 (1997)
J. Kaludjerovic, W.E. Ward, The interplay between estrogen and fetal adrenal cortex. J Nutr Metab 2012, 837901 (2012)
J. Shamash, J. Stebbing, C. Sweeney, G. Sonpavde, S. Harland, G. Dawkins, C. Brock, W. Abelman, P. Wilson, A. Sanitt, T. Oliver, T. Powles, A validated prognostic index predicting response to dexamethasone and diethylstilbestrol in castrate-resistant prostate cancer. Cancer 116, 3595–3602 (2010)
S. Kitahara, H. Umeda, M. Yano, F. Koga, S. Sumi, H. Moriguchi, Y. Hosoya, M. Honda, K. Yoshida, Effects of intravenous administration of high dose-diethylstilbestrol diphosphate on serum hormonal levels in patients with hormone-refractory prostate cancer. Endocr. J. 19, 659–664 (1999)
S. Haeno, N. Maeda, T. Yagi, S. Tahata, M. Sato, K. Sakaguchi, T. Miyasho, H. Ueda, H. Yokota, Diethylstilbestrol decreased adrenal cholesterol and corticosterone in rats. J. Endocrinol. 221, 269–280 (2014)
F.B. Kraemer, Adrenal cholesterol utilization. Mol. Cell. Endocrinol. 265–266, 42–45 (2007)
H. Inoue, H. Yokota, T. Makino, A. Yuasa, S. Kato, Bisphenol a glucuronide, a major metabolite in rat bile after liver perfusion. Drug Metab. Dispos. 29, 1084–1087 (2001)
T. Sugano, K. Suda, M. Shimada, N. Oshino, Biochemical and ultrastructural evaluation of isolated rat liver systems perfused with a hemoglobin-free medium. J. Biochem. 83, 995–1007 (1978)
Y. Li, K. Okumura, S. Nomura, N. Maeda, T. Miyasho, H. Yokota, Oxidatively damaged proteins in the early stage of testicular toxicities in male rats by orally administered with a synthetic oestrogen, diethylstilbestrol. Reprod. Toxicol. 31, 26–34 (2011)
O.H. Lowry, N.J. Rosebrough, A.L. Farr, R.J. Randall, Protein measurement with the Folin phenol reagent. J. Biol. Chem. 193, 265–275 (1951)
M.W. Duncan, A.L. Yergey, S.D. Patterson, Quantifying proteins by mass spectrometry: the selectivity of SRM is only part of the problem. Proteomics 9, 1124–1127 (2009)
N. Maeda, E. Tanaka, T. Suzuki, K. Okumura, S. Nomura, T. Miyasho, S. Haeno, H. Yokota, Accurate determination of tissue steroid hormones, precursors and conjugates in adult male rat. J. Biochem. 153, 63–71 (2013)
N. Maeda, K. Okumura, E. Tanaka, T. Suzuki, T. Miyasho, S. Haeno, H. Ueda, N. Hoshi, H. Yokota, Downregulation of cytochrome P450scc as an initial adverse effect of adult exposure to diethylstilbestrol on testicular steroidogenesis (Environ, Toxicol, 2013)
K.E. Kypreos, V.I. Zannis, Pathway of biogenesis of apolipoprotein E-containing HDL in vivo with the participation of ABCA1 and LCAT. Biochem. J. 403, 359–367 (2007)
M.A. Connelly, SR-BI-mediated HDL cholesteryl ester delivery in the adrenal gland. Mol. Cell. Endocrinol. 300, 83–88 (2009)
C. Parthasarathy, K. Balasubramanian, Assessment of in vitro effects of metyrapone on Leydig cell steroidogenesis. Steroids 73, 328–338 (2008)
S. Whirledge, J.A. Cidlowski, Glucocorticoids, stress, and fertility. Minerva Endocrinol. 35, 109–125 (2010)
C. Parthasarathy, K. Balasubramanian, Effects of corticosterone deficiency and its replacement on Leydig cell steroidogenesis. J. Cell. Biochem. 104, 1671–1683 (2008)
R.A. Srivastava, D. Baumann, G. Schonfeld, In vivo regulation of low-density lipoprotein receptors by estrogen differs at the post-transcriptional level in rat and mouse. Eur. J. Biochem. 216, 527–538 (1993)
R.A. Srivastava, N. Srivastava, M. Averna, R.C. Lin, K.S. Korach, D.B. Lubahn, G. Schonfeld, Estrogen up-regulates apolipoprotein E (ApoE) gene expression by increasing ApoE mRNA in the translating pool via the estrogen receptor alpha-mediated pathway. J. Biol. Chem. 272, 33360–33366 (1997)
T.J. Schoenfeld, E. Gould, Stress, stress hormones, and adult neurogenesis. Exp. Neurol. 233, 12–21 (2012)
S.K. Droste, A. Gesing, S. Ulbricht, M.B. Muller, A.C. Linthorst, J.M. Reul, Effects of long-term voluntary exercise on the mouse hypothalamic-pituitary-adrenocortical axis. Endocrinology 144, 3012–3023 (2003)
A. Makatsori, R. Duncko, M. Schwendt, F. Moncek, B.B. Johansson, D. Jezova, Voluntary wheel running modulates glutamate receptor subunit gene expression and stress hormone release in Lewis rats. Psychoneuroendocrinology 28, 702–714 (2003)
A.M. Stranahan, D. Khalil, E. Gould, Social isolation delays the positive effects of running on adult neurogenesis. Nat. Neurosci. 9, 526–533 (2006)
F. Klaus, T. Hauser, L. Slomianka, H.P. Lipp, I. Amrein, A reward increases running-wheel performance without changing cell proliferation, neuronal differentiation or cell death in the dentate gyrus of C57BL/6 mice. Behav. Brain Res. 204, 175–181 (2009)
H. van Praag, G. Kempermann, F.H. Gage, Running increases cell proliferation and neurogenesis in the adult mouse dentate gyrus. Nat. Neurosci. 2, 266–270 (1999)
J.S. Snyder, L.R. Glover, K.M. Sanzone, J.F. Kamhi, H.A. Cameron, The effects of exercise and stress on the survival and maturation of adult-generated granule cells. Hippocampus 19, 898–906 (2009)
S.S. Yi, I.K. Hwang, K.Y. Yoo, O.K. Park, J. Yu, B. Yan, I.Y. Kim, Y.N. Kim, T. Pai, W. Song, I.S. Lee, M.H. Won, J.K. Seong, Y.S. Yoon, Effects of treadmill exercise on cell proliferation and differentiation in the subgranular zone of the dentate gyrus in a rat model of type II diabetes. Neurochem. Res. 34, 1039–1046 (2009)
D.J. Gordon, B.M. Rifkind, High-density lipoprotein–the clinical implications of recent studies. N. Engl. J. Med. 321, 1311–1316 (1989)
F.E. Thorngate, P.G. Yancey, G. Kellner-Weibel, L.L. Rudel, G.H. Rothblat, D.L. Williams, Testing the role of apoA-I, HDL, and cholesterol efflux in the atheroprotective action of low-level apoE expression. J. Lipid Res. 44, 2331–2338 (2003)
Acknowledgments
The authors are grateful to Mr. Michio Sasaki of Japan Meat Science and Technology Institute for his suggestions and helpful advice. This work was supported in part by the Supported Program for the Strategic Research Foundation at Private Universities (2013–2017) of the Ministry of Education, Culture, Science and Technology, Japan.
Author Contributions
Conceived and designed the experiments: SH and HY. Performed the experiments: SH, NM, KY, MS and AU. Analyzed the data: SH, NM and HY. Contributed reagents/materials/analysis tools: SH, NM, KY, MS, AU and HY. Wrote the paper: SH and HY.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Author H. Yokota has received research grant from a Grant-in-aid and Support Project to Assist Private Universities in Developing Bases for Research from the Ministry of Education, Science, Sports and Culture and Technology in Japan.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12020_2015_732_MOESM1_ESM.eps
Supplementary material 1 Fig. 1 Illustrated procedure of liver perfusion. Rats were orally administered DES (0.33 µg/g of body mass), and livers were prepared as described in the Materials and Methods. Oxygenated Krebs–Ringer buffer was perfused into the liver via the portal vein as described in the Materials and Methods. The resultant perfusate (100 μl) was sampled at each time point. The amount of Apo A1 and Apo E secreted from the liver into the perfusate was assayed by western blotting analysis using each antibody. (EPS 1342 kb)
Rights and permissions
About this article
Cite this article
Haeno, S., Maeda, N., Yamaguchi, K. et al. Adrenal steroidogenesis disruption caused by HDL/cholesterol suppression in diethylstilbestrol-treated adult male rat. Endocrine 52, 148–156 (2016). https://doi.org/10.1007/s12020-015-0732-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0732-5