Abstract
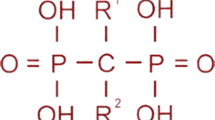
Most pediatric bone diseases result either from mutations of the essential genes for bone development or from abnormalities of mineral homeostasis. With an increase in non-invasive techniques to measure bone mineral density, the number of children with apparent low bone mineral density is rising. Furthermore, a new classification system proposed by the International Society for Clinical Densitometry now considers osteoporosis a valid diagnosis in children. Osteoporosis is a particular problem among children with conditions such as muscular dystrophy, immobilization, and chronic liver diseases and those who received a prolonged course of glucocorticoids. Pharmacologic agents for treatment of osteoporosis were developed primarily to prevent fragility fractures in postmenopausal women, and studies of their efficacy and safety in children are limited. Recent advances have seen new therapies for bone diseases in children; some of these conditions were deemed incurable in the past. This article reviews data regarding mechanism of action, safety, and efficacy of four bone drugs in pediatric patients. These are (1) zoledronic acid, a long-acting bisphosphonate; (2) denosumab, a RANKL inhibitor; (3) asfotase alfa, a synthetic alkaline phosphatase; and (4) burosumab, a monoclonal antibody against FGF23.

Similar content being viewed by others
References
Spranger JW, Brill PW, Nishimura G, Superti-Furga A, Unger S. Introduction. In: Spranger JW, Brill PW, Nishimura G, Superti-Furga A, Unger S, editors. Bone dysplasias. New York: Oxford University Press; 2012.
Geister KA, Camper SA. Advances in skeletal dysplasia genetics. Annu Rev Genomics Hum Genet. 2015;16(1):199–227. https://doi.org/10.1146/annurev-genom-090314-045904.
Dubail J, Brunelle P, Baujat G, Huber C, Doyard M, Michot C, et al. Homozygous loss-of-function mutations in CCDC134 are responsible for a severe form of osteogenesis imperfecta. J Bone Miner Res. 2020. https://doi.org/10.1002/jbmr.4011.
Rafati M, Mohamadhashem F, Hoseini A, Hoseininasab F, Ghaffari SR. A novel ACVR1 mutation detected by whole exome sequencing in a family with an unusual skeletal dysplasia. Eur J Med Genet. 2016;59(6–7):330–6. https://doi.org/10.1016/j.ejmg.2016.05.007.
Marini JC, Forlino A, Bachinger HP, Bishop NJ, Byers PH, Paepe A, et al. Osteogenesis imperfecta. Nat Rev Dis Primers. 2017;3(1):17052. https://doi.org/10.1038/nrdp.2017.52.
Lindahl K, Kindmark A, Rubin CJ, Malmgren B, Grigelioniene G, Soderhall S, et al. Decreased fracture rate, pharmacogenetics and BMD response in 79 Swedish children with osteogenesis imperfecta types I, III and IV treated with pamidronate. Bone. 2016;87:11–8. https://doi.org/10.1016/j.bone.2016.02.015.
The International For Clinical Densitometry. 2019 ISCD Official Positions – Pediatric. 2019. https://www.iscd.org/official-positions/2019-iscd-official-positions-pediatric/.
Bachrach LK, Gordon CM, Section on Endocrinology. Bone densitometry in children and adolescents. Pediatrics. 2016;138(4). https://doi.org/10.1542/peds.2016-2398.
Zemel BS, Leonard MB, Kelly A, Lappe JM, Gilsanz V, Oberfield S, et al. Height adjustment in assessing dual energy x-ray absorptiometry measurements of bone mass and density in children. J Clin Endocrinol Metab. 2010;95(3):1265–73. https://doi.org/10.1210/jc.2009-2057.
Klein GL. Introduction. In: Klein GL, editor. Bone drugs in pediatrics. New York: Springer; 2014.
Biggin A, Munns CF. Bisphosphonates in osteogenesis imperfecta. In: Klein GL, editor. Bone drug in pediatrics. New York: Springer; 2014.
Russell RG. Bisphosphonates: the first 40 years. Bone. 2011;49(1):2–19. https://doi.org/10.1016/j.bone.2011.04.022.
Sbrocchi AM, Forget S, Laforte D, Azouz EM, Rodd C. Zoledronic acid for the treatment of osteopenia in pediatric Crohn’s disease. Pediatr Int. 2010;52(5):754–61. https://doi.org/10.1111/j.1442-200X.2010.03174.x.
Barros ER, Saraiva GL, de Oliveira TP, Lazaretti-Castro M. Safety and efficacy of a 1-year treatment with zoledronic acid compared with pamidronate in children with osteogenesis imperfecta. J Pediatr Endocrinol Metab. 2012;25(5–6):485–91. https://doi.org/10.1515/jpem-2012-0016.
Bowden SA, Mahan JD. Zoledronic acid in pediatric metabolic bone disorders. Transl Pediatr. 2017;6(4):256–68. https://doi.org/10.21037/tp.2017.09.10.
Otaify GA, Aglan MS, Ibrahim MM, Elnashar M, El Banna RA, Temtamy SA. Zoledronic acid in children with osteogenesis imperfecta and Bruck syndrome: a 2-year prospective observational study. Osteoporos Int. 2016;27(1):81–92. https://doi.org/10.1007/s00198-015-3216-9.
Panigrahi I, Das RR, Sharda S, Marwaha RK, Khandelwal N. Response to zolendronic acid in children with type III osteogenesis imperfecta. J Bone Miner Metab. 2010;28(4):451–5. https://doi.org/10.1007/s00774-009-0149-4.
Constantino CS, Krzak JJ, Fial AV, Kruger KM, Rammer JR, Radmanovic K, et al. Effect of bisphosphonates on function and mobility among children with osteogenesis imperfecta: a systematic review. JBMR Plus. 2019;3(10):e10216. https://doi.org/10.1002/jbm4.10216.
Li LJ, Zheng WB, Zhao DC, Yu W, Wang O, Jiang Y, et al. Effects of zoledronic acid on vertebral shape of children and adolescents with osteogenesis imperfecta. Bone. 2019;127:164–71. https://doi.org/10.1016/j.bone.2019.06.011.
Robinson ME, Trejo P, Palomo T, Glorieux FH, Rauch F. Osteogenesis imperfecta: skeletal outcomes after bisphosphonate discontinuation at final height. J Bone Miner Res. 2019;34(12):2198–204. https://doi.org/10.1002/jbmr.3833.
George S, Weber DR, Kaplan P, Hummel K, Monk HM, Levine MA. Short-term safety of zoledronic acid in young patients with bone disorders: an extensive institutional experience. J Clin Endocrinol Metab. 2015;100(11):4163–71. https://doi.org/10.1210/jc.2015-2680.
Sbrocchi AM, Rauch F, Jacob P, McCormick A, McMillan HJ, Matzinger MA, et al. The use of intravenous bisphosphonate therapy to treat vertebral fractures due to osteoporosis among boys with Duchenne muscular dystrophy. Osteoporos Int. 2012;23(11):2703–11. https://doi.org/10.1007/s00198-012-1911-3.
Lim A, Zacharin M, Pitkin J, de Valle K, Ryan MM, Simm PJ. Therapeutic options to improve bone health outcomes in Duchenne muscular dystrophy: zoledronic acid and pubertal induction. J Paediatr Child Health. 2017;53(12):1247–8. https://doi.org/10.1111/jpc.13692.
Nasomyont N, Hornung LN, Wasserman H. Intravenous bisphosphonate therapy in children with spinal muscular atrophy. Osteoporos Int. 2020;31(5):995–1000. https://doi.org/10.1007/s00198-019-05227-9.
Boyce AM, Chong WH, Yao J, Gafni RI, Kelly MH, Chamberlain CE, et al. Denosumab treatment for fibrous dysplasia. J Bone Miner Res. 2012;27(7):1462–70. https://doi.org/10.1002/jbmr.1603.
Eller-Vainicher C, Rossi DS, Guglielmi G, Beltramini GA, Cairoli E, Russillo A, et al. Prompt clinical and biochemical response to denosumab in a young adult patient with craniofacial fibrous dysplasia. Clin Cases Miner Bone Metab. 2016;13(3):253–6. https://doi.org/10.11138/ccmbm/2016.13.3.253.
Majoor BCJ, Papapoulos SE, Dijkstra PDS, Fiocco M, Hamdy NAT, Appelman-Dijkstra NM. Denosumab in patients with fibrous dysplasia previously treated with bisphosphonates. J Clin Endocrinol Metab. 2019;104(12):6069–78. https://doi.org/10.1210/jc.2018-02543.
Semler O, Netzer C, Hoyer-Kuhn H, Becker J, Eysel P, Schoenau E. First use of the RANKL antibody denosumab in osteogenesis imperfecta type VI. J Musculoskelet Neuronal Interact. 2012;12(3):183–8.
Hoyer-Kuhn H, Netzer C, Koerber F, Schoenau E, Semler O. Two years’ experience with denosumab for children with osteogenesis imperfecta type VI. Orphanet J Rare Dis. 2014;9(1):145. https://doi.org/10.1186/s13023-014-0145-1.
Trejo P, Palomo T, Montpetit K, Fassier F, Sato A, Glorieux FH, et al. Long-term follow-up in osteogenesis imperfecta type VI. Osteoporos Int. 2017;28(10):2975–83. https://doi.org/10.1007/s00198-017-4141-x.
Ward L, Bardai G, Moffatt P, Al-Jallad H, Trejo P, Glorieux FH, et al. Osteogenesis imperfecta type VI in individuals from Northern Canada. Calcif Tissue Int. 2016;98(6):566–72. https://doi.org/10.1007/s00223-016-0110-1.
Federman N, Brien EW, Narasimhan V, Dry SM, Sodhi M, Chawla SP. Giant cell tumor of bone in childhood: clinical aspects and novel therapeutic targets. Paediatr Drugs. 2014;16(1):21–8. https://doi.org/10.1007/s40272-013-0051-3.
Bardakhchyan S, Kager L, Danielyan S, Avagyan A, Karamyan N, Vardevanyan H, et al. Denosumab treatment for progressive skull base giant cell tumor of bone in a 14 year old female - a case report and literature review. Ital J Pediatr. 2017;43(1):32. https://doi.org/10.1186/s13052-017-0353-0.
Karras NA, Polgreen LE, Ogilvie C, Manivel JC, Skubitz KM, Lipsitz E. Denosumab treatment of metastatic giant-cell tumor of bone in a 10-year-old girl. J Clin Oncol. 2013;31(12):e200–2. https://doi.org/10.1200/JCO.2012.46.4255.
Reddy K, Ramirez L, Kukreja K, Venkatramani R. Response to denosumab in 2 children with recurrent giant cell tumor of the bone with pulmonary metastasis. J Pediatr Hematol Oncol. 2019;Publish Ahead of Print. https://doi.org/10.1097/MPH.0000000000001654.
Uday S, Gaston CL, Rogers L, Parry M, Joffe J, Pearson J, et al. Osteonecrosis of the jaw and rebound hypercalcemia in young people treated with denosumab for giant cell tumor of bone. J Clin Endocrinol Metab. 2018;103(2):596–603. https://doi.org/10.1210/jc.2017-02025.
Bredell M, Rordorf T, Kroiss S, Rucker M, Zweifel DF, Rostetter C. Denosumab as a treatment alternative for central giant cell granuloma: a long-term retrospective cohort study. J Oral Maxillofac Surg. 2018;76(4):775–84. https://doi.org/10.1016/j.joms.2017.09.013.
Naidu A, Malmquist MP, Denham CA, Schow SR. Management of central giant cell granuloma with subcutaneous denosumab therapy. J Oral Maxillofac Surg. 2014;72(12):2469–84. https://doi.org/10.1016/j.joms.2014.06.456.
Upfill-Brown A, Bukata S, Bernthal NM, Felsenfeld AL, Nelson SD, Singh A, et al. Use of denosumab in children with osteoclast bone dysplasias: report of three cases. JBMR Plus. 2019;3(10):e10210. https://doi.org/10.1002/jbm4.10210.
Kurucu N, Akyuz C, Ergen FB, Yalcin B, Kosemehmetoglu K, Ayvaz M et al. Denosumab treatment in aneurysmal bone cyst: evaluation of nine cases. Pediatr Blood Cancer. 2018;65(4). https://doi.org/10.1002/pbc.26926.
Lange T, Stehling C, Frohlich B, Klingenhofer M, Kunkel P, Schneppenheim R, et al. Denosumab: a potential new and innovative treatment option for aneurysmal bone cysts. Eur Spine J. 2013;22(6):1417–22. https://doi.org/10.1007/s00586-013-2715-7.
Durr HR, Grahneis F, Baur-Melnyk A, Knosel T, Birkenmaier C, Jansson V, et al. Aneurysmal bone cyst: results of an off label treatment with denosumab. BMC Musculoskelet Disord. 2019;20(1):456. https://doi.org/10.1186/s12891-019-2855-y.
Raux S, Bouhamama A, Gaspar N, Brugieres L, Entz-Werle N, Mallet C, et al. Denosumab for treating aneurysmal bone cysts in children. Orthop Traumatol Surg Res. 2019;105(6):1181–5. https://doi.org/10.1016/j.otsr.2019.04.028.
Grasemann C, Schundeln MM, Hovel M, Schweiger B, Bergmann C, Herrmann R, et al. Effects of RANK-ligand antibody (denosumab) treatment on bone turnover markers in a girl with juvenile Paget’s disease. J Clin Endocrinol Metab. 2013;98(8):3121–6. https://doi.org/10.1210/jc.2013-1143.
Whyte MP, Greenberg CR, Salman NJ, Bober MB, McAlister WH, Wenkert D, et al. Enzyme-replacement therapy in life-threatening hypophosphatasia. N Engl J Med. 2012;366(10):904–13. https://doi.org/10.1056/NEJMoa1106173.
Whyte MP, Simmons JH, Moseley S, Fujita KP, Bishop N, Salman NJ, et al. Asfotase alfa for infants and young children with hypophosphatasia: 7 year outcomes of a single-arm, open-label, phase 2 extension trial. Lancet Diabetes Endocrinol. 2019;7(2):93–105. https://doi.org/10.1016/S2213-8587(18)30307-3.
Whyte MP, Rockman-Greenberg C, Ozono K, Riese R, Moseley S, Melian A, et al. Asfotase alfa treatment improves survival for perinatal and infantile hypophosphatasia. J Clin Endocrinol Metab. 2016;101(1):334–42. https://doi.org/10.1210/jc.2015-3462.
Whyte MP, Madson KL, Phillips D, Reeves AL, McAlister WH, Yakimoski A, et al. Asfotase alfa therapy for children with hypophosphatasia. JCI Insight. 2016;1(9):e85971. https://doi.org/10.1172/jci.insight.85971.
Kishnani PS, Rockman-Greenberg C, Rauch F, Bhatti MT, Moseley S, Denker AE, et al. Five-year efficacy and safety of asfotase alfa therapy for adults and adolescents with hypophosphatasia. Bone. 2019;121:149–62. https://doi.org/10.1016/j.bone.2018.12.011.
Carpenter TO, Whyte MP, Imel EA, Boot AM, Hogler W, Linglart A, et al. Burosumab therapy in children with X-linked hypophosphatemia. N Engl J Med. 2018;378(21):1987–98. https://doi.org/10.1056/NEJMoa1714641.
Whyte MP, Carpenter TO, Gottesman GS, Mao M, Skrinar A, San Martin J, et al. Efficacy and safety of burosumab in children aged 1-4 years with X-linked hypophosphataemia: a multicentre, open-label, phase 2 trial. Lancet Diabetes Endocrinol. 2019;7(3):189–99. https://doi.org/10.1016/S2213-8587(18)30338-3.
Imel EA, Glorieux FH, Whyte MP, Munns CF, Ward LM, Nilsson O, et al. Burosumab versus conventional therapy in children with X-linked hypophosphataemia: a randomised, active-controlled, open-label, phase 3 trial. Lancet. 2019;393(10189):2416–27. https://doi.org/10.1016/S0140-6736(19)30654-3.
Bell JM, Shields MD, Watters J, Hamilton A, Beringer T, Elliott M, et al. Interventions to prevent and treat corticosteroid-induced osteoporosis and prevent osteoporotic fractures in Duchenne muscular dystrophy. Cochrane Database Syst Rev. 2017;1:CD010899. https://doi.org/10.1002/14651858.CD010899.pub2.
Faienza MF, Chiarito M, D’Amato G, Colaianni G, Colucci S, Grano M, et al. Monoclonal antibodies for treating osteoporosis. Expert Opin Biol Ther. 2018;18(2):149–57. https://doi.org/10.1080/14712598.2018.1401607.
Boyce AM. Denosumab: an emerging therapy in pediatric bone disorders. Curr Osteoporos Rep. 2017;15(4):283–92. https://doi.org/10.1007/s11914-017-0380-1.
Gibiansky L, Sutjandra L, Doshi S, Zheng J, Sohn W, Peterson MC, et al. Population pharmacokinetic analysis of denosumab in patients with bone metastases from solid tumours. Clin Pharmacokinet. 2012;51(4):247–60. https://doi.org/10.2165/11598090-000000000-00000.
Sutjandra L, Rodriguez RD, Doshi S, Ma M, Peterson MC, Jang GR, et al. Population pharmacokinetic meta-analysis of denosumab in healthy subjects and postmenopausal women with osteopenia or osteoporosis. Clin Pharmacokinet. 2011;50(12):793–807. https://doi.org/10.2165/11594240-000000000-00000.
Brunetti G, Papadia F, Tummolo A, Fischetto R, Nicastro F, Piacente L, et al. Impaired bone remodeling in children with osteogenesis imperfecta treated and untreated with bisphosphonates: the role of DKK1, RANKL, and TNF-alpha. Osteoporos Int. 2016;27(7):2355–65. https://doi.org/10.1007/s00198-016-3501-2.
Li H, Jiang X, Delaney J, Franceschetti T, Bilic-Curcic I, Kalinovsky J, et al. Immature osteoblast lineage cells increase osteoclastogenesis in osteogenesis imperfecta murine. Am J Pathol. 2010;176(5):2405–13. https://doi.org/10.2353/ajpath.2010.090704.
Glorieux FH, Ward LM, Rauch F, Lalic L, Roughley PJ, Travers R. Osteogenesis imperfecta type VI: a form of brittle bone disease with a mineralization defect. J Bone Miner Res. 2002;17(1):30–8. https://doi.org/10.1359/jbmr.2002.17.1.30.
Trejo P, Rauch F, Ward L. Hypercalcemia and hypercalciuria during denosumab treatment in children with osteogenesis imperfecta type VI. J Musculoskelet Neuronal Interact. 2018;18(1):76–80.
Hoyer-Kuhn H, Franklin J, Allo G, Kron M, Netzer C, Eysel P, et al. Safety and efficacy of denosumab in children with osteogenesis imperfect--a first prospective trial. J Musculoskelet Neuronal Interact. 2016;16(1):24–32.
Li G, Jin Y, Levine MAH, Hoyer-Kuhn H, Ward L, Adachi JD. Systematic review of the effect of denosumab on children with osteogenesis imperfecta showed inconsistent findings. Acta Paediatr. 2018;107(3):534–7.
Lipplaa A, Dijkstra S, Gelderblom H. Challenges of denosumab in giant cell tumor of bone, and other giant cell-rich tumors of bone. Curr Opin Oncol. 2019;31(4):329–35. https://doi.org/10.1097/CCO.0000000000000529.
Polyzos SA, Cundy T, Mantzoros CS. Juvenile Paget disease. Metabolism. 2018;80:15–26. https://doi.org/10.1016/j.metabol.2017.10.007.
Gossai N, Hilgers MV, Polgreen LE, Greengard EG. Critical hypercalcemia following discontinuation of denosumab therapy for metastatic giant cell tumor of bone. Pediatr Blood Cancer. 2015;62(6):1078–80. https://doi.org/10.1002/pbc.25393.
Setsu N, Kobayashi E, Asano N, Yasui N, Kawamoto H, Kawai A, et al. Severe hypercalcemia following denosumab treatment in a juvenile patient. J Bone Miner Metab. 2016;34(1):118–22. https://doi.org/10.1007/s00774-015-0677-z.
Kobayashi E, Setsu N. Osteosclerosis induced by denosumab. Lancet. 2015;385(9967):539. https://doi.org/10.1016/S0140-6736(14)61338-6.
Wang HD, Boyce AM, Tsai JY, Gafni RI, Farley FA, Kasa-Vubu JZ, et al. Effects of denosumab treatment and discontinuation on human growth plates. J Clin Endocrinol Metab. 2014;99(3):891–7. https://doi.org/10.1210/jc.2013-3081.
Scott LJ. Asfotase alfa in perinatal/infantile-onset and juvenile-onset hypophosphatasia: a guide to its use in the USA. BioDrugs. 2016;30(1):41–8. https://doi.org/10.1007/s40259-016-0161-x.
Yadav MC, de Oliveira RC, Foster BL, Fong H, Cory E, Narisawa S, et al. Enzyme replacement prevents enamel defects in hypophosphatasia mice. J Bone Miner Res. 2012;27(8):1722–34. https://doi.org/10.1002/jbmr.1619.
Whyte MP. Hypophosphatasia - aetiology, nosology, pathogenesis, diagnosis and treatment. Nat Rev Endocrinol. 2016;12(4):233–46. https://doi.org/10.1038/nrendo.2016.14.
Scott LJ. Asfotase alfa: a review in paediatric-onset hypophosphatasia. Drugs. 2016;76(2):255–62. https://doi.org/10.1007/s40265-015-0535-2.
Mornet E. Hypophosphatasia. Metabolism. 2018;82:142–55. https://doi.org/10.1016/j.metabol.2017.08.013.
Whyte MP, Leung E, Wilcox WR, Liese J, Argente J, Martos-Moreno GA, et al. Natural history of perinatal and infantile hypophosphatasia: a retrospective study. J Pediatr. 2019;209:116–24 e4. https://doi.org/10.1016/j.jpeds.2019.01.049.
Hofmann CE, Harmatz P, Vockley J, Hogler W, Nakayama H, Bishop N, et al. Efficacy and safety of asfotase alfa in infants and young children with hypophosphatasia: a phase 2 open-label study. J Clin Endocrinol Metab. 2019;104(7):2735–47. https://doi.org/10.1210/jc.2018-02335.
Rush ET. Childhood hypophosphatasia: to treat or not to treat. Orphanet J Rare Dis. 2018;13(1):116. https://doi.org/10.1186/s13023-018-0866-7.
Mornet E. Genetics of hypophosphatasia. Arch Pediatr. 2017;24(5S2):5S51–5S6. https://doi.org/10.1016/S0929-693X(18)30014-9.
Bowden SA, Adler BH. Reappearance of hypomineralized bone after discontinuation of asfotase alfa treatment for severe childhood hypophosphatasia. Osteoporos Int. 2018;29(9):2155–6. https://doi.org/10.1007/s00198-018-4613-7.
Kishnani PS, Rush ET, Arundel P, Bishop N, Dahir K, Fraser W, et al. Monitoring guidance for patients with hypophosphatasia treated with asfotase alfa. Mol Genet Metab. 2017;122(1–2):4–17. https://doi.org/10.1016/j.ymgme.2017.07.010.
Lyseng-Williamson KA. Burosumab in X-linked hypophosphatemia: a profile of its use in the USA. Drugs Ther Perspect. 2018;34(11):497–506. https://doi.org/10.1007/s40267-018-0560-9.
Imel EA, Biggin A, Schindeler A, Munns CF. FGF23, hypophosphatemia, and emerging treatments. JBMR Plus. 2019;3(8):e10190. https://doi.org/10.1002/jbm4.10190.
Zhang X, Peyret T, Gosselin NH, Marier JF, Imel EA, Carpenter TO. Population pharmacokinetic and pharmacodynamic analyses from a 4-month intradose escalation and its subsequent 12-month dose titration studies for a human monoclonal anti-FGF23 antibody (KRN23) in adults with X-linked hypophosphatemia. J Clin Pharmacol. 2016;56(4):429–38. https://doi.org/10.1002/jcph.611.
Beck-Nielsen SS, Mughal Z, Haffner D, Nilsson O, Levtchenko E, Ariceta G, et al. FGF23 and its role in X-linked hypophosphatemia-related morbidity. Orphanet J Rare Dis. 2019;14(1):58. https://doi.org/10.1186/s13023-019-1014-8.
Gordon RJ, Levine MA. Burosumab treatment of children with X-linked hypophosphataemic rickets. Lancet. 2019;393(10189):2364–6. https://doi.org/10.1016/S0140-6736(19)31054-2.
Availability of Data and Material
The data that support this article are available from the corresponding author upon reasonable request.
Code Availability
Not applicable
Author information
Authors and Affiliations
Contributions
Supamit Ukarapong designed the concepts of the article, performed the literature search, drafted and revised the manuscript, and approved the version to be published. Tossaporn Seeherunvong performed the literature search, drafted and revised the manuscript, and approved the version to be published. Gary Berkovitz critically revised the manuscript and approved the version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethics Approval
The article does not contain any studies with human or animal subjects performed by any of the authors.
Consent to Participate
Not applicable
Consent for Publication
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ukarapong, S., Seeherunvong, T. & Berkovitz, G. Current and Emerging Therapies for Pediatric Bone Diseases. Clinic Rev Bone Miner Metab 18, 31–42 (2020). https://doi.org/10.1007/s12018-020-09272-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12018-020-09272-5