Abstract
Occurrence of autoantibodies (autoAbs) is a hallmark of autoimmune diseases, and the analysis thereof is an essential part in the diagnosis of organ-specific autoimmune and systemic autoimmune rheumatic diseases (SARD), especially connective tissue diseases (CTDs). Due to the appearance of autoAb profiles in SARD patients and the complexity of the corresponding serological diagnosis, different diagnostic strategies have been suggested for appropriate autoAb testing. Thus, evolving assay techniques and the continuous discovery of novel autoantigens have greatly influenced the development of these strategies. Antinuclear antibody (ANA) analysis by indirect immunofluorescence (IIF) on tissue and later cellular substrates was one of the first tests introduced into clinical routine and is still an indispensable tool for CTD serology. Thus, screening for ANA by IIF is recommended to be followed by confirmatory testing of positive findings employing different assay techniques. Given the continuous growth in the demand for autoAb testing, IIF has been challenged as the standard method for ANA and other autoAb analyses due to lacking automation, standardization, modern data management, and human bias in IIF pattern interpretation. To address these limitations of autoAb testing, the CytoBead® technique has been introduced recently which enables automated interpretation of cell-based IIF and quantitative autoAb multiplexing by addressable microbead immunoassays in one reaction environment. Thus, autoAb screening and confirmatory testing can be combined for the first time. The present review discusses the history of autoAb assay techniques in this context and gives an overview and outlook of the recent progress in emerging technologies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autoantibodies as Diagnostic Markers
Connective Tissue Disease-Specific Autoantibodies
The loss of immune tolerance characteristic for connective tissue diseases (CTDs) such as systemic lupus erythematosus (SLE), systemic sclerosis (SSc), poly/dermatomyositis (PM/DM), Sjögren’s syndrome (SjS), and mixed connective tissue disease (MCTD) brings about the generation of various nonorgan-specific autoantibodies (autoAbs) [1–3]. Although the triggering factors for the occurrence of autoAbs and their role in the pathogenesis of CTD are still not entirely understood, autoAbs are widely used as diagnostic markers in clinical routine nowadays [4, 5]. The L.E. cell phenomenon described by Hargraves in the late 1940 in patients suffering from SLE proved to be a result of autoAb binding to nuclear material of polymorphs and marked the beginning of a rapidly evolving autoAb era in clinical diagnostics [6]. Indirect immunofluorescence (IIF) was the first assay technique employed to reveal autoAbs in patients with CTD [7]. The groundbreaking works of Holborow and Friou et al. led to the discovery of so-called antinuclear antibodies (ANAs) as marker autoAbs of CTD like SLE [8, 9]. In the following years, clinicians made tremendous efforts to understand the clinical significance of autoAbs and their potential use for the serological diagnosis of CTD and beyond [10]. This process was greatly driven by novel emerging assay techniques used for autoAb testing and their respective assay performance characteristics (Fig. 1; Table 1). The ensuing discourse has led to the definition of various diagnostic strategies for the serological diagnosis of autoimmune disorders and continues to date. Of note, ANA detected by IIF was included into the diagnostic criteria of SLE and autoimmune hepatitis (AIH) later [11–13]. In this context, the discovery of autoAbs to extractable nuclear antigens (ENAs) apart from autoAbs to dsDNA or histones in the search for disease-specific autoAbs provides an intriguing example for the change in the understanding of the clinical meaning of autoAbs as diagnostic markers [14–16]. Thus, the seminal paper of E.M. Tan and H.G. Kunkel on the identification of Sm as an autoantigenic target of SLE and the use of double radial immunodiffusion (DRID; Ouchterlony technique) for its detection ushered in a new era in autoAb diagnostics and its clinical application [17]. Although ANA turned out to be a sensitive marker for SARD as a whole disease group, its specificity for distinct SARD entities was not satisfactory despite being defined as a diagnostic marker for SLE [11]. Thus, the clinical need for more specific “ANA” was met by the pioneering work of H.G. Kunkel, E.M. Tan, and others discovering more and more novel autoAbs to ENA with clinical significance [14, 18]. However, not all ENAs identified as targets for CTD-specific autoAbs could be isolated by the saline extraction technique reported previously and should not be termed ENA [19]. Furthermore, apart from autoAbs recognizing nuclear autoantigens, anticytoplasmic autoAbs (ACyA) have been introduced into the autoAb panel for SARD serology [20]. Thus, the anti-SjS antigen A (SS-A) autoAbs also termed Ro have been shown to interact with its respective target in the cytoplasm [21]. As a fact, the progress in proteomics enabled the identification of cytoplasmic autoantigenic targets interacting with for instance myositis-specific autoAbs like anti-histidyl tRNAse autoAbs (Jo-1) or SLE specific autoAb against ribosomal proteins [22–24]. Obviously, this created confusion among clinical and laboratory experts and called for clarification. In terms of ANA testing, the introduction of human epidermoid laryngeal carcinoma (HEp-2) cells as improved autoantigenic substrate in IIF has encouraged the reporting of CTD-specific cytoplasmic patterns over the years [2]. This contradiction in terminology was addressed by a recent consensus recommending the use of anticellular antibodies instead of ANA [4]. Notwithstanding, the use of ANA and ENA is well established particularly among clinicians and it remains to be seen how this issue will be solved adequately in the years to come [25]. In summary, autoAb testing is an integral part in the serological diagnosis of CTD and may also assist in the prognosis, subclassification, as well as monitoring of disease activity [4, 10, 26–29].
Evolving autoantibody (autoAb) testing and strategies for the serological diagnosis of systemic autoimmune rheumatic diseases. ANA antinuclear antibody, autoAb autoantibody, CIE counterimmunoelectrophoresis, D/LIA dot/line immunoassay, ELISA enzyme-linked immunosorbent assay, ENA extractable nuclear antigen, IB immunoblot/westernblot, ID/DRID immunodiffusion/double radial immunodiffusion, IIF indirect immunofluorescence, IP immunoprecipitation, MIA microbead immunoassay, RIP radioimmunoprecipitation
As mentioned earlier, not only the discovery of novel SARD-specific autoAbs has challenged the diagnostic skills of clinicians but the introduction of novel assay techniques with differing assay performance, too [30]. Thus, the change from immunodiffusion-based detection techniques like DRID or counterimmunoelectrophoresis (CIE) detecting precipitating autoAbs to enzyme-linked immunosorbent assay (ELISA) regarding the analysis of autoAbs to Sm or SS-A called the specificity of these distinct markers suddenly into question [31–33]. The solid-phase ELISA brought about a significantly elevated sensitivity which in turn is related to a diminished diagnostic specificity [34]. Furthermore, with the better understanding of the chemical structure of for instance the small nuclear ribonucleoprotein (snRNP) complex representing the Sm autoantigen, six different protein structures (B, B’, D, E, F, G) were identified as autoantigenic targets with SmD being apparently the most specific one for SLE [35–37]. Alone, these critical aspects require a comprehensive knowledge on the interpretation of assay characteristics by clinicians which were not always conveyed by laboratorians adequately [1, 3]. The badly needed comprehension of pretest and posttest probabilities of presence of disease and its relation to the diagnostic performance of autoAb analysis such as ANA testing appears not satisfactorily developed in clinicians [19, 38, 39]. Thus, novel diagnostic strategies translating the progress in autoAb testing proved difficult to get in line with established diagnostic pathways [27, 40, 41]. The recent attempt to substitute ANA IIF testing as screening assay within the two-tier strategy by novel multiplex techniques failed or met with great resistance among rheumatologists [4, 42, 43]. Consequently, the two-stage strategy recommending ANA testing by IIF as screening and appropriate confirmation of ANA positives by a different analysis was confirmed by expert consensus for CTD serology recently [4].
Autoimmune Vasculitis-Specific Autoantibodies
Of note, like revealed for the L.E. phenomenon in patients with SLE, patients suffering from autoimmune vasculitides demonstrate loss of tolerance to polymorphs, too [44]. In contrast, the occurring autoAbs recognize specific neutrophil cytoplasmic and not nonspecific nuclear components and were described first in association with glomerulonephritis in 1982 by Davies et al. [45]. Van de Woude’s group reported so-called antineutrophil cytoplasmic antibodies (ANCAs) to be associated with granulomatosis with polyangiitis (GPA, formerly Wegener’s granulomatosis) shortly later and, consequently, the term ANCA-associated vasculitides (AAV) was coined [44, 46, 47]. Thus, this group of autoimmune vascular disorders comprises GPA, microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA, formerly Churg-Strauss syndrome) [48, 49]. Their leading clinical characteristics are microvascular inflammation, tissue necrosis, and the appearance of ANCAs [50].
Interestingly, similar to ANA testing, IIF was the first method to be used for the detection of ANCA revealing two major patterns, cytoplasmic (cANCA) and perinuclear ANCA (pANCA) [45, 51]. Not surprisingly, the respective main autoantigenic neutrophilic targets, proteinase 3 (PR3), and myeloperoxidase (MPO) were discovered shortly afterward [52, 53]. Consequently, a two-stage strategy for ANCA testing highlighting IIF as a standard method is recommended by international consensus for the serology of AAV, too [54]. Indeed, the unsurpassed high sensitivity of autoAb analysis employing cellular substrates by IIF renders this method an ideal tool for the screening stage followed by confirmatory testing with different immunological assay technologies [47]. However, similar to ANA IIF reading, interpretation of ANCA patterns is rather time consuming due to lack of automation and skilled laboratory experts [55]. Thus, IIF is in general highly subjective what renders appropriate standardization difficult [56, 57]. Therefore, attempts to replace IIF by novel techniques based on solid-phase immunoassays (e.g., ELISA, dot/line immunoassay, addressable bead/microarray assays) for ANCA as well as ANA analyses are increasing currently [58–62]. Indeed, in contrast to IIF, these assay techniques can be automated and proved to be more cost-efficient in the modern laboratory environment characterized by a rising diagnostic demand due to the growing clinical impact of autoimmune diseases. However, worrying rates of false-negative findings have been reported for these techniques in terms of ANA as well as ANCA testing [42]. Of note, this fact also appears to be relevant for organ-specific autoimmune disorders like celiac disease (CD).
Celiac Disease-Specific (Auto)Antibodies
Celiac disease, a gluten-related and immune-mediated small intestinal disease, is one of the few autoimmune disorders which the triggering factor was identified for [63]. Indeed, gliadin peptides deamidated by tissue transglutaminase type 2 (TG2) were shown as gluten-related T-cell epitopes triggering chronic inflammatory intestinal lesions and leading to villous atrophy and hyperplasia of the crypts [64].
Like for CTD and AAV, serology is paramount for the diagnosis of CD encompassing the detection of (auto)Abs to endomysium (EmA), deamidated gliadin peptides (DGP), and TG2 of the IgA isotype [65]. As a fact, due to the excellent assay performance of EmA testing by IIF, this particular autoAb is still considered the reference standard for CD-specific (auto)Abs [65–67]. However, similar to ANA and ANCA testing by IIF, EmA IIF analysis was questioned more and more because it may be subject to interobserver as well as substrate-related variability and is difficult to automate [68]. Obviously, testing of anti-TG2 autoAbs by immunometric solid-phase assays was favored instead [69–72].
In summary, IIF as one of the first techniques employed for autoAb testing in various autoimmune disease diagnostics appears to keep its appeal with laboratorians and clinicians despite several shortcomings [73, 74]. The integration of IIF as screening or standard method for autoAb analysis into two-stage or multiplex strategies was necessary as yet, but creates cost constraints for health care systems already burdened with spiraling costs. This calls for innovative solutions to meet the growing demand for autoAb testing in clinical routine.
Evolving Assay Techniques for Autoantibody Testing
Single Tests for autoAb Analysis
The introduction of fluorescent dyes and the development of immunochemical methods for the labeling of antibodies on the one hand and fluorescence microscopy on the other hand paved the way for IIF as powerful tool for autoAb analysis in the 1950s [75]. Thus, the detection of ANA by IIF employing first rodent liver tissue and later HEp-2 cells as autoantigenic substrate marks the beginning of autoAb detection in the serological diagnosis of CTD [7, 9, 76, 77]. However, it turned out soon that the clinical need for disease-specific autoAbs was not appropriately addressed by ANA testing alone. The search for more specific autoAbs led to the introduction of immunodiffusion techniques which enabled the discovery of disease-specific autoAbs like the Sm autoAb in patients suffering from SLE [16, 17, 21]. In particular, DID employing thymic extracts was used and clinicians learnt to appreciate the high specificity of this new parameter for CTD serology. Not surprisingly, autoAbs to Sm were included along with ANA in the diagnostic criteria for SLE later and are still considered as one of the most specific serological parameters for SLE [11, 14]. However, DRID is a time-consuming technique and, thus, was replaced by CIE enabling a faster and more sensitive detection of precipitating autoAbs later on [31]. Several other important autoAbs to the spliceosomal complex such as autoAbs to U1 ribonucleoprotein (U1-RNP) were identified in the quest for new CTD markers [21]. Anti-U1-RNP was established as a specific serological marker for MCTD and found in patients with SLE as well [78, 79]. The introduction of new assay techniques like radio- (RIA) and enzyme immunoassays as well as radio/immunoprecipitation paved the way for the development of autoAb detection assays with better assay performance [32, 62, 80–86]. In particular, the progress in proteomics and the introduction of the immunoblot technique enabled the purification and identification of the distinct autoantigenic targets [33, 87–89]. It turned out that Sm and U1-RNP consist of several autoantigenic components including U1-RNA with different characteristics regarding their performance as split autoantigens especially in solid-phase ELISAs [79, 90, 91]. Furthermore, the SjS-specific autoantigens SS-A and SS-B form a complex interacting with yRNA [92]. Of note, this confers only to the SS-A 60 kDa unit whereas the 52 kDa SS-A (TRIM21) does not bind to yRNA and is not related to this snRNP complex [93, 94]. This raised the question of the best composition of these targets for the detection of the distinct autoAbs or the use of the target subcomponent with the best assay performance [90]. In terms of U1-RNP consisting of components A, C, and a 68 kDa polypeptide, it was found that at least two of these three should be used as solid-phase antigens to set up an appropriate ELISA for the detection of autoAbs to U1-RNP [19]. In contrast, SmD of the Sm complex with its six subcomponents mentioned earlier appeared to be the most specific and sensitive autoantigenic target in ELISA for the serology of SLE [14].
In general, the introduction of solid-phase assays like ELISA was accompanied by four major aspects changing the understanding of autoAb testing for CTD diagnostics: (i) a better usability as assay platform, (ii) an increasing sensitivity compared with immunodiffusion techniques, (iii) the different assay performance of autoAbs recognizing conformational or nonconformational, linear epitopes, and (iv) the introduction of reference sera for standardized diagnostics. This was an essential step toward standardization and automation of autoAb testing addressing the growing demand thereof due to the inclusion of autoAb testing into diagnostic or classification criteria of more and more autoimmune diseases and changed the autoimmune laboratory environment dramatically [80, 95]. Consequently, assay techniques like IIF, which have been prone to subjectivity and difficult to automate until recently, were subjected to a rising pressure to be substituted [73, 96, 97]. In this context, several researchers were tempted by the advantages of the ELISA technique and in particular its higher sensitivity to develop assays employing cellular extracts of MOLT4 or HEp-2 cells [98–101]. Furthermore, the elevated sensitivity of particularly anti-SS-A ELISAs revealed false-negative ANA sera of patients suffering from CTD [102–105]. Indeed, this seems to be the only autoantigenic target which is not adequately presented even by HEp-2 cells and can result in false-negative ANA findings by IIF. To overcome this shortcoming of the appreciated IIF technique, genetically modified HEp-2 cells with a higher expression of the SS-A 60 kDA polypeptide were introduced in ANA testing [103, 106].
Of note, the increased sensitivity of ELISA resulted in positive autoAb findings in nondiseased individuals, too, which started an intense discourse on the right method for cutoff determination [80]. Finally, receiver operating characteristics curve analysis was approved for quantitative methods like ELISA as the best approach to do so [39]. Part of the false-positive findings could be assigned to autoAbs occurring before the onset of disease as putative predictive markers thereof [29, 107]. Nonetheless, false-positive findings in ELISA could be a result of autoAbs to less disease-specific nonconformational epitopes [108]. These autoAbs often belong to the natural autoAb repertoire and display a low affinity to its corresponding targets [109]. A very convincing example is the anti-double-stranded DNA (dsDNA) autoAb which was established as diagnostic marker of SLE [110]. Of note, the SLE-specific dsDNA epitope is ill-defined and IIF assays employing kinetoplast dsDNA of Crithidia luciliae (CLIFT) with its characteristic epitope structure appear to provide the best specificity for this important disease activity-associated SLE marker [108, 111–113]. The replacement of CLIFT and the Farr RIA measuring mainly high-affinity anti-dsDNA autoAbs due to a high-salt reaction environment by ELISAs detecting autoAbs to both nonconformational and conformational dsDNA epitopes resulted in high numbers of false-positives particularly in patients with infectious diseases [114].
A similar phenomenon was observed when recombinant or synthetic autoantigens were introduced into autoAb testing to overcome the difficulties related to antigen purification and standardization [115, 116]. Not in each case, these nonnative polypeptides could replace the native autoantigenic targets for an appropriate autoAb analysis. Thus, the SmD polypeptide was dependent on the symmetric methylation of arginine to represent the SLE-specific epitope for the sensitive detection of anti-Sm autoAbs [35, 36, 117]. Furthermore, the presence of yRNA for the autoantigenicity of the SS-A/SS-B complex on the one hand and of U1-RNA for the Sm/RNP unit on the other hand was obviously required for the sensitive analysis of the respective autoAbs [118, 119].
Remarkably, specific ANCA testing demonstrated similar difficulties. Like for ANA testing, IIF was introduced as first assay technique on fixed neutrophils [45]. However, the following identification of PR3 and MPO as the main ANCA targets and the subsequent analysis of respective autoAbs by ELISA were hampered by the nonsatisfactory sensitivity of anti-PR3 autoAb tests [120–122]. Indeed, the conformational epitopes on PR3 were difficult to preserve on the solid phases of ELISAs. Recently, the third generation of PR3-ANCA ELISA has been introduced employing anchor molecules during adsorption of PR3 to the solid phase to preserve its confirmation and accessibility of vasculitis-specific epitopes [121, 122]. Other attempts to develop highly sensitive PR3-ANCA ELISAs comprised the use of a mixture of native as well as recombinant PR3 [123].
The close relation between sensitivity and specificity is presumably the reason that direct-ligand RIAs with their excellent sensitivity have not been used widely for the analysis of CTD- or AAV-specific autoAbs. Interestingly, this is in contrast to organ-specific autoimmune entities such as type 1 diabetes (T1D) where RIAs are appreciated hitherto due to their high sensitivity [124, 125]. Of note, IIF on endocrine pancreas had also been the first technique used for autoAb analysis before the corresponding autoantigens were identified [126]. The detection of islet-cell autoAbs by IIF is still in use; however, the impact of conformational epitopes for T1D autoAbs testing in conjunction with the increased sensitivity of RIAs and recently emerging ELISAs with similar assay performances have almost replaced IIF [127].
After the discovery of TG2 as autoantigenic target of EmA for CD serology, a similar development was observed in the serological diagnosis of CD [128]. To obtain a sensitive anti-TG2 autoAb assay, conformational epitopes of TG2 seem to be essential, too [129]. In contrast to T1D autoAb testing, however, the detection of EmA by IIF is still the gold standard [65].
As a fact, the higher disease specificity of autoAbs to conformational epitopes is probably the reason for today’s infrequent use of immunoblot assays for autoAb serology [130]. Obviously, due to the poor presentation of such epitopes on the blot membrane as a result of the denaturing effect of sodium dodecyl sulfate during electrophoresis and the poor standardization of the method due to technical peculiarities, the immunoblot technique has lost its initial appeal for multiplex autoAb testing [89, 131].
Notwithstanding, due to the progress in the identification of ever more autoAbs aiding in diagnosing, predicting and prognosing autoimmune diseases, the search for the most adequate strategy of autoAb testing fulfilling clinical needs and cost constraints has been in the focus of laboratory and clinical experts ever since [5, 59, 132–134]. For instance, more than 100 autoAbs were found in SLE patients alone [135]. This led to the introduction of fully automated random-access instruments employing fluorescence or chemiluminescence as read out for autoAb testing as well as screening [136–139].
Remarkably, a two-stage strategy was recommended for both ANA and ANCA analyses by international consensus recommendations [4, 54]. Thus, IIF is still considered a reliable screening test characterized by a high negative predictive value. Positive IIF findings should be confirmed by specific autoAb testing employing assay techniques with high specificity. For several other autoimmune disorders like for instance CD, IIF is still considered a gold standard [65]. Thus, despite the introduction of assay techniques for the detection of specific autoAb reactivities, there is still a need for testing of autoAbs by various assay techniques.
Multiplex Assays for autoAb Testing
The rising number of autoAbs requested for the serology of one autoimmune entity as well as the growing demand for autoAb testing in general encouraged the development of multiplex testing [3, 140–142]. Despite the fact that ANA assessment by IIF using HEp-2 cells as autoantigenic substrate is already a multiplex test revealing different patterns according to the autoAbs present in the serum investigated, the analysis of specific autoAbs is hardly achievable [20, 96, 143, 144]. Even for such ready to detect ANA patterns like the centromere one with its more than 40 fluorescent dots spread in nuclei of interphase cells and densely aligned dots in the metaphase cells, several proteins could be recognized by autoAbs as autoantigenic targets (centromere-associated proteins A, B, and C) [57, 76, 145–147].
As mentioned earlier, immunoblot was one of the first attempts to establish an appropriate multiplex test for the confirmation of ANA by using whole cell extracts with a similar autoantigen composition of HEp-2 cells [98, 148]. However, due to technical challenges, poor reproducibility, and loss of the native conformational structure of the relevant autoantigenic epitopes, this method was not established as a standard for multiplex autoAb analysis [19, 25, 149, 150].
As a result of improved purification methods for native autoantigens and progress in the expression of recombinant autoantigenic targets, the use of both molecule sources did not only enable the development of singleplex autoAb ELISAs but of multiplex dot or line immunoassays (D/LIAs), too [116, 140, 151]. In daily laboratory routine, D/LIAs have been established as one of the standard tests for ANA and ANCA confirmation [140, 152–154]. Moreover, D/LIAs appear to be an ideal solution for other serological diagnoses, where multiple autoAbs are required [155–158]. This holds not only true for CD serology where even a simultaneous IgA deficiency can be conducted apart from the (auto)Ab testing but proved to be very effective for the serology of SSc, DM/PM, or autoimmune liver diseases [140, 154]. Thus, D/LIAs with more than 20 autoantigenic targets have been introduced for the confirmatory diagnostics of ANA successfully [159]. Of note, the miniaturization of the technique by deploying sophisticated nanoliter dispensing devices and pattern recognition software for optical density reading render this technique most potential for future multiplex autoAb testing [160].
It should be noted in this context, that the attempts to employ the 96-well ELISA platform for autoAb multiplexing by using single wells for the immobilization of distinct antigens appear to be just an intermediate stage which was called into question very soon due to obvious shortcomings of the approach.
The progress in fluorescence reading as well as flow cytometry and microscopy paved the way for a new era in multiplexing [161–169]. Thus, several multiplex assay developments employing surface-activated microbeads coded by fluorescent dyes, size, or shape on the one hand and fluorescence microscopy or flow cytometry as read-out on the other hand were reported [170–172].
The intriguing biochip mosaic technology enabled multiplex autoAb IIF reading by using various cellular and tissue substrates on one solid phase [173–175]. Further, the luminex technology deploying fluorescence-coded microbeads and flow cytometry enabled the development of an intriguing and very successful multiplex autoAb detection technique [176, 177]. Very soon, this novel technology was commercialized by several companies. The possibility to detect several autoAbs and the high throughput led to the development of such multiplex autoAb systems like Athena and FIDIS or the fully automated BioPlex2000 system covering various serological autoimmune diagnoses [172, 177–179]. The growing success and the ready automation of the luminex technology were very appealing especially for larger laboratories with ever growing sample volumes [177]. Indeed, demand for autoAb testing started rising exponentially in the 1980s and this phenomenon called into question even the recommended two-tier strategy encompassing IIF as the ideal autoAb screening [180–182]. As a matter of fact, laboratories in particular in the USA have begun replacing IIF due to its major shortcomings, namely lack of automation, standardization, modern data processing, and experts in IIF reading [3, 43, 73, 170, 183, 184]. Although the newly developed luminex applications for autoAb testing helped to ease the pressure in terms of rising autoAb analyses, there was growing dissatisfaction among rheumatologists with the assay performance of the technology [42]. Indeed, false-negative ANA findings leading to ill-defined diagnoses raised the concern of clinicians [185, 186]. Consequently, the American College of Rheumatology (ACR) initiated a task force in 2009 investigating the issue [42]. In conclusion, IIF was confirmed as standard method for ANA reading and laboratories requested to return to the two-stage strategy or to make sure that clinicians requesting ANA testing are aware of the different assay performance by multiplexing [4].
Of note, despite the development of similar multiplex tests for ANCA testing, IIF was also not challenged as screening assay in the two-stage strategy yet.
Improvement of IIF by Digital Fluorescence
The decision of the ANA task force of the ACR to retain the status of IIF and, thus, to confirm the two-stage strategy for CTD serology required an overhaul of the IIF technique badly [180, 181].
To employ this technique in a modern laboratory environment for CTD-associated antibody testing, the earlier mentioned shortcomings of IIF are needed to be addressed. In this context, the tremendous progress in fluorescence microscopy, image taking, and software development helped to usher in a new era of digital fluorescence [56, 161, 187, 188]. To the best of our knowledge, our group was the first to overcome critical disadvantages of ANA reading with IIF by introducing a standardized and automated fluorescence interpretation system which is based on the Videoscan technology and commercialized under the AKLIDES® brand [162, 189, 190]. AKLIDES® enables automated IIF reading by a sequential, multistage process including image acquisition by a CCD camera and software-controlled quality control, object segmentation, object description, and object classification by the use of novel pattern recognition algorithms. Thus, the system representing a composition of different hardware modules including a motorized inverse fluorescence microscope enables dynamic autofocusing resulting in the acquisition of quantitative fluorescence signals. The ensuing increased standardization and automation diminished the high intralaboratory and interlaboratory variability of ANA IIF reading, allowed the differentiation of cytoplasmic from nuclear staining, and rendered this method more applicable to high throughput screening [191–193].
Other diagnostic companies started developing similar systems and introducing new technologies for automated IIF pattern interpretation. In general, these commercially available systems are based on digital acquisition of fluorescence signals and most of them enable automated analysis of IIF images by pattern recognition algorithms (AKLIDES®, Medipan, Dahlewitz/Berlin, Germany; Nova View®, Inova, San Diego, USA; Zenit G Sight, A. Menarini Diagnostics, Grassina-Firenze, Italy; Europattern®, Euroimmun, Lübeck, Germany) [20, 194–196]. However, few systems distinguish between positive and negative screening results only (Helios, Aesku.Diagnostics, Wendelsheim, Germany; Image Navigator, Immuno Concepts, Sacramento, USA; Cytospot, Autoimmun Diagnostika, Straßberg, Germany) [185, 197]. In summary, all systems were reported to meet the demand for automated interpretation and satisfactory system performances were obtained by comparative studies at least for qualitative ANA evaluation [197, 198].
The fully automated interpretation system AKLIDES® was the first platform which performance was evaluated in clinical studies successfully [199–201]. Egerer et al. published the first clinical evaluation in 2010 by comparing the use of the new technology for ANA assessment of 1222 sera in the routine laboratory environment of both a university and a private referral laboratory [199]. An agreement of 93.0 % (859/924) and of 90.6 % (270/298) between automated AKLIDES® interpretation and classical ANA reading in the university and the private laboratory were reported, respectively. Remarkably, end-titer analysis based on quantitative fluorescence reading was shown for the first time, which overcomes a crucial shortcoming of IIF and levels it with other quantitative assay techniques established in routine clinical laboratories. Thus, the application range of the novel interpretation systems (AKLIDES®, Europattern®, NovaView®) was enlarged by adding ANCA and anti-dsDNA autoAb testing on human neutrophils and Crithidia luciliae, respectively [191, 202–204].
In summary, the intriguing development of these novel automated IIF interpretation systems strengthened the position of IIF as screening technique within the two-tier strategy for ANA and ANCA analyses. Thus, the demand of even large laboratories in terms of automated autoAb testing by IIF with modern data management could be addressed adequately. Tozzoli et al. concluded that a new technological era in the routine autoimmune laboratory was reached by the introduction of fully automated IIF in 2009 [180]. Furthermore, this technology may also stimulate clinical research regarding larger population studies, e.g., the prevalence of the dense-fine speckled (DFS) pattern, and hence, of the DFS70 autoAbs, in different apparently healthy and diseased populations [205].
Combination of Screening and Confirmatory Testing
Irrespectively of the tremendous progress in automated autoAb testing by IIF at the beginning of this millennium, the constraint to use two different assay techniques for the recommended two-stage strategy of ANA and ANCA analyses has not been abolished yet [4]. This strategy enables a plausibility control of the obtained results because specific autoAb assays may give false-positive findings. For instance, a positive anti-dsDNA finding in ELISA in combination with ANA negativity cannot be regarded as relevant regarding diagnosis of SLE. However, the possibility of false-negative findings using the two-tier strategy especially for ANA reading in terms of sera positive for autoAbs to SS antigen A (SS-A/Ro) is still eminent at hand and represents an essential drawback of such approach [206]. Only the combination of both stages in one multiplex test would overcome these shortcomings and provide an ideal solution for autoAb testing addressing key clinical and laboratory needs. As a fact, this intriguing idea is quite simple, and thus, it appears astonishing that no such attempt was undertaken earlier. Hence, combination of the advantages of cell-based assays and the potential for multiplexing by microbead immunoassay (MIA) employing IIF within one reaction environment could revolutionize autoimmune diagnostics (Fig. 2).
Multiplexing strategy of CytoBead® technology exemplified for CytoBead® ANA assay. Combination of ANA screening with HEp-2 cells (middle part) and anti-ENA testing with antigen-coated microbeads (peripheral parts I–IV) in one reaction environment. Example of an ANA positive serum with positive homogeneous fluorescence pattern on HEp-2 cells and positive signal on dsDNA-coated microbeads presented as green fluorescence halo (small red microbeads in part III). ANA antinuclear antibody, CENP centromere protein, Da Dalton, dsDNA double-stranded DNA, ENA extractable nuclear antigen, hom homogeneous, RNP ribonuclear protein, Scl-70 DNA-Topoisomerase I, Sm Smith, SS Sjögren-Syndrome, (+) positive, (−) negative
Second-Generation ANA Testing
To realize the idea of combining autoAb screening and confirmation, we started developing a unique IIF reaction environment encompassing classical ANA analysis on HEp-2 cells and simultaneous multiplex detection of autoAbs by MIA. Indeed, merging screening and confirmatory testing for disease-specific autoAbs could generate many benefits including shorter hands-on times, better reproducibility of autoAb findings, and higher cost-effectiveness especially for larger sample series.
First, a MIA which utilizes multiple carboxylated polymethylmethacrylate bead populations differing in size and/or concentrations of fluorescent dye for multiplexing was developed [207]. The classification of bead populations and measurement of corresponding ligand fluorescence intensity was readily performed by AKLIDES® enabling the detection of six different antinuclear autoAbs to Scl-70, Sm, SS-A (Ro60), SS-B (La), CENP-B, and, dsDNA. This assay development created the basis for the design of a unique IIF reaction environment which could integrate the classical ANA testing on HEp-2 cells in one test [102]. The new assay technique combining classical ANA testing with confirmatory analysis by MIA was termed CytoBead® technology (Fig. 3a). Intriguingly, the novel options of digital fluorescence enabling quantitative analysis not only of specific autoAb testing by MIA but also of classical ANA reading on HEp-2 cells can be readily employed by CytoBead® assays. Thus, they can be standardized by calibrated interpretation systems for automated autoAb testing. Consequently, this is a new age of standardization of ANA testing as a whole which was not feasible with classical ANA testing by IIF in the past.
CytoBead® assays for the detection of a antinuclear antibodies (ANA) with CytoBead® ANA assay, b antineutrophil cytoplasmic autoantibodies (ANCA) with CytoBead® ANCA assay, and c celiac disease (CD)-specific (auto)antibodies (auto/Abs) with CytoBead® CeliAK assay. Matching principle of specific fluorescence patterns on HEp-2 cells (a), neutrophil granulocytes (b), and esophagus tissue (c) with positive reactions of antigen-coated microbeads immobilized in peripheral compartments. CENP centromere protein, Da Dalton, dsDNA double-stranded DNA, EmA endomysial antibody, GBM glomerular basement membrane, MPO myeloperoxidase, PR3 proteinase 3, RNP ribonuclear protein, Scl-70 DNA-Topoisomerase I, Sm Smith, SS Sjögren-Syndrome, (+) positive, (−) negative
Altogether, a new generation of autoAb testing could be established that can meet the demand of modern routine service laboratories for the serology of SARD/CTD by addressing the key disadvantages of the currently recommended two-stage autoAb testing.
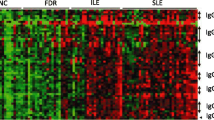
Recently, this new assay referred to as second generation ANA testing was evaluated in a comprehensive serological study comprising inter alia 174 patients with SLE, 103 with SSc, 46 with SjS, 36 with RA, 13 with MCTD, 21 with DM/PM, 21 with infectious disease, 93 with autoimmune liver diseases, 78 with inflammatory bowel disease, and 101 blood donors [102]. The CytoBead® ANA simultaneously determines ANA on HEp-2 cells and autoAbs to dsDNA, CENP-B, SS-A/Ro52, SS-A/Ro60, SS-B/La, RNP-Sm, Sm, and Scl-70. The obtained good agreement of the CytoBead® ANA with classical ANA reading by IIF and ELISA supports the notion that the novel combined reaction IIF environment for one-step ANA analysis employing HEp-2 cells and autoantigen-coated fluorescent beads as respective targets can provide at least the same assay performance like classical two-tier ANA testing.
Furthermore, simultaneous detection of ANA and specific autoAbs such as to SS-A/Ro by CytoBead® ANA can almost eliminate the risk of false-negative findings and increase the already high negative predictive value of ANA testing. Of note, this is especially in the interest of rheumatologists who would like to exclude the presence of autoimmunity in their differential diagnosis of SARD by ordering ANA testing. In this study, 4/267 (1.5 %) ANA-negative patients with positive anti-SS-A or anti-CENP-B autoAbs were determined by second-generation ANA analysis. As a fact, these distinct patients with RA and SjS would have been missed by the currently recommended two-tier strategy since ANA negativity and positivity for anti-SS-A and anti-CENP-B autoAbs were confirmed by classical testing.
New-Generation ANCA Testing
The CytoBead® technology was also applied for the comprehensive analysis of ANCA and the resulting CytoBead® ANCA was evaluated in terms of its assay performance [208]. Indeed, the combination of both IIF and antigen-specific assays was found in several studies to be the optimal strategy for ANCA detection and led to the recommendation of a two-stage ANCA testing.
Alike CytoBead® ANA development, after having designed a multiplex addressable MIA detecting MPO-ANCA, PR3-ANCA, and autoAbs against the noncollagen region of the alpha-3 subunit of collagen IV representing the glomerular basement membrane (GBM) antigen, a unique reaction environment for the additional detection of ANCA on fixed neutrophils was generated (Fig. 3b). The novel CytoBead® ANCA is a unique combination of a classical cell-based assay with multiplexing microbead technology [204, 208].
Sowa et al. recruited 592 patients including 118 patients with AAV, 133 with RA, 49 with infectious diseases, 77 with inflammatory bowel disease, 20 with autoimmune liver diseases, 70 with primary sclerosing cholangitis (PSC), and 125 blood donors and compared multiplex CytoBead® ANCA testing with classical methods such as IIF and ELISA [208]. Quantitative PR3- and MPO-ANCA analysis by multiplex CytoBead® technology turned out to be at least equal or better compared to classical ELISA testing for specific ANCA. Remarkably, automated endpoint ANCA titer analysis by only one serum dilution employing the automated interpretation system AKLIDES® revealed a very good agreement with the classical ANCA IIF on neutrophils. Another intriguing finding was the detection of PR3-ANCA in patients suffering from ulcerative colitis (UC) and PSC apart from those with GPA. These data appear to confirm a recent report of PR3-ANCA positive patients suffering from UC and PSC detected by another sensitive MIA technique [138]. Thus, the new reaction environment of the CytoBead® ANCA enables highly sensitive PR3-ANCA testing and might compete with third-generation ELISA in terms of assay performance.
Consequently, automated multiplex IIF combining screening and confirmatory ANCA testing in one test may replace the time-consuming current two-stage ANCA testing strategy by a one-step multiplexing CytoBead® analysis [206]. In context of the emergency diagnostics required for rapidly progressive glomerulonephritis, the novel multiplex ANCA analysis by CytoBead® appears to be an attractive approach to meet the clinical need for comprehensive ANCA testing in the fastest way possible.
Comprehensive CD Serology
The serological diagnosis of CD comprises the detection of EMA and auto/Abs against deamidated gliadin and TG2 of the IgA isotype. As a fact, EmA detected by IIF is still considered the gold standard for (auto)Ab testing in CD [65]. To address the need for comprehensive CD-specific (auto)Ab testing in terms of workload and cost reduction in routine autoimmune laboratories, we developed a multiplex CytoBead® CeliAK assay (Fig. 3c) [209]. Multiplex CD-specific (auto)Ab testing might even be an attractive diagnostic tool in the context of the novel diagnostic criteria published by the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) recently [65]. These criteria obviously strengthen the role of CD serology within the workup of patients with the suspicion of CD. Thus, CD can be diagnosed without histology by waiving duodenal biopsy in case of anti-TG2 autoAb IgA levels 10 times higher than the upper limit of normal (ULN) in patients positive for HLA-DQ2 or HLA-DQ8 and a positive response to gluten-free diet or confirmation by EmA testing.
Hence, the novel CytoBead® CeliAK was evaluated by investigating in total 380 patients and controls comprising 155 CD patients, 5 with IgA-deficiency, 68 with cystic fibrosis, 59 with eye diseases, and 93 blood donors [209]. Findings were compared with classical IgA-(auto)Ab analyses by ELISA and IIF. As a fact, the difference between CytoBead® and classical testing was only significant for anti-TG2 autoAb testing whereas the eight discrepant sera with anti-TG2 autoAb positivity by ELISA and negative levels by CytoBead® CeliAK belonged to four CD patients and four controls. Altogether, the CytoBead® CeliAK represents the first multiplex quantitative IgA anti-TG2 autoAb and anti-DG Ab multiplex assay which provides simultaneous EmA analysis as reference method and IgA deficiency testing. This comprehensive approach has the potential to improve CD serology and demonstrated excellent results regarding the great number of CD patients with anti-TG2 autoAb levels >10× ULN due to its high sensitivity. Additionally, due to the flexibility of the technique, further autoAbs such as those to GP2 stratifying CD patients further might be included [210, 211].
Conclusion
Hitherto, the history of autoAb testing has been characterized by an intriguing development of several assay techniques to keep up with the tremendous progress in the understanding of autoimmune diseases and their appropriate diagnostics [180, 197]. Today, autoAb analysis is an integral part in the serological diagnosis of SARD like CTD and AAV and organ-specific autoimmune disorders [4, 26, 60]. Hence, there is no doubt that the introduction and further evolvement of IIF as one of the first autoAb-detecting assay techniques had and have an essential impact on this process [162, 197]. In the history of autoAb testing, various techniques emerged and were replaced by newer ones providing better assay performance and benefits regarding higher sample throughput and standardization [34, 80]. In this context, it is astonishing to note that IIF is still one of the key techniques to analyze autoAbs and even recommended as screening assay within the two-stage strategy for ANA and ANCA testing. In addition, IIF remains a reference method for the detection of distinct autoAbs like EmA in the serology of organ-specific autoimmune disorders indeed [65].
Despite the obvious benefits of IIF, this assay technique has been characterized by time consuming and subjective evaluation, insufficient automation, as well as poor standardization since its introduction [162]. In particular, pattern reading for ANA and ANCA testing was prone to inconsistencies in description and classification of respective staining patterns.
As a consequence, novel assay techniques based on solid-phase immunoassays like ELISA or multiplexing technologies creating the basis for different commercial platforms evolved and were introduced into routine autoimmune laboratories [149]. Nonetheless, IIF is still recommended to be used as the gold standard method for instance for ANA testing due to the unsatisfactory assay performance of even the latest multiplex technologies in this important area of autoAb analysis [4].
This situation changed dramatically by the development of digital fluorescence and its implementation in IIF testing. The breathtaking new options of pattern recognition combined with progress in automated fluorescence microscopy paved the way for the evolvement of an entirely new generation of automated interpretation systems [206]. Different commercially available IIF platforms for autoAb testing were designed and applied for ANA and ANCA reading in particular. First evaluation studies support the good performance of these systems and high agreement between visual and automated autoAb interpretation [212].
Of note, this enormous technology development comprising digital fluorescence image acquisition and automatic pattern recognition could be extended to other cell-based IIF assays in the search for new biomarkers. Thus, the quantification of γH2AX foci for DNA damage analysis, which used to be time consuming, subjective, and not suitable for high-throughput screening, could be standardized and automated [213, 214]. Successful evaluation studies support the introduction of this new DNA damage marker into clinical routine for cytostatic resistance development diagnostics [215].
Nevertheless, since the majority of clinical immunology laboratories follow the two-stage strategy for ANA and ANCA testing, substantial constraints regarding high-throughput and cost-effectiveness remain. The expansion of automated IIF interpretation systems like AKLIDES® to assess addressable MIAs created a unique novel assay platform allowing fully automated evaluation of cell-based screening tests and antigen-specific multiplex assays in one reaction environment for the first time. The evolvement of the CytoBead® technology combining quantitative autoAb screening and confirmatory testing in one IIF analysis enables second-generation autoAb detection in one test. This intriguing multiplex reaction environment addresses key needs for an effective standardized autoAb testing in laboratory routine. Major disadvantages of classical autoAb analysis by IIF were overcome by this new technique. First diagnostic applications for second-generation ANA and ANCA testing as well as comprehensive serology of CD-specific (auto)Abs were developed and successfully evaluated.
References
Stinton LM, Fritzler MJ (2007) A clinical approach to autoantibody testing in systemic autoimmune rheumatic disorders. Autoimmun Rev 7:77–84
Damoiseaux J, Andrade LE, Fritzler MJ, Shoenfeld Y (2015) Autoantibodies 2015: from diagnostic biomarkers toward prediction, prognosis and prevention. Autoimmun Rev 14:555–563
Fritzler MJ, Wiik A, Fritzler ML, Barr SG (2003) The use and abuse of commercial kits used to detect autoantibodies. Arthritis Res Ther 5:192–201
Agmon-Levin N, Damoiseaux J, Kallenberg C et al (2014) International recommendations for the assessment of autoantibodies to cellular antigens referred to as anti-nuclear antibodies. Ann Rheum Dis 73:17–23
Conrad K, Roggenbuck D, Reinhold D, Sack U (2012) Autoantibody diagnostics in clinical practice. Autoimmun Rev 11:207–211
Hargraves MM, Richmond H, Morton R (1948) Presentation of two bone marrow elements; the tart cell and the L.E. cell. Proc Staff Meet Mayo Clin 23:25–28
Friou GJ, Finch SC, Detre KD (1958) Interaction of nuclei and globulin from lupus erythematosis serum demonstrated with fluorescent antibody. J Immunol 80:324–329
Friou GJ (1958) Clinical application of a test for lupus globulin-nucleohistone interaction using fluorescent antibody. Yale J Biol Med 31:40–47
Holbrow EJ, Weir DM, Johnson G (1957) A serum factor in lupus erythematosus with affinity for tissue nuclei. Br Med J 2:732–734
Fritzler MJ (2008) Challenges to the use of autoantibodies as predictors of disease onset, diagnosis and outcomes. Autoimmun Rev 7:616–620
Tan EM, Cohen AS, Fries JF et al (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–1277
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Alvarez F, Berg PA, Bianchi FB et al (1999) International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol 31:929–938
Tan EM, Kunkel HG (2006) Characteristics of a soluble nuclear antigen precipitating with sera of patients with systemic lupus erythematosus. J. Immunol. 1966. 96: 464-471. J Immunol 176:1297–1304
Seligmann M (1958) Immunological studies on disseminated lupus erythematosus. Rev Fr Etud Clin Biol 3:558–584
Tan EM, Schur PH, Carr RI, Kunkel HG (1966) Deoxyribonucleic acid (DNA) and antibodies to DNA in the serum of patients with systemic lupus erythematosus. J Clin Invest 45:1732–1740
Tan EM, Kunkel HG (1966) Characteristics of a soluble nuclear antigen precipitating with sera of patients with systemic lupus erythematosus. J Immunol 96:464–471
Kunkel HG, Tan EM (1964) Autoantibodies and disease. Adv Immunol 27:351–395
Damoiseaux JG, Tervaert JW (2006) From ANA to ENA: how to proceed? Autoimmun Rev 5:10–17
Mahler M, Meroni PL, Bossuyt X, Fritzler MJ (2014) Current concepts and future directions for the assessment of autoantibodies to cellular antigens referred to as anti-nuclear antibodies. J Immunol Res 2014:315179
Clark G, Reichlin M, Tomasi TB Jr (1969) Characterization of a soluble cytoplasmic antigen reactive with sera from patients with systemic lupus erythmatosus. J Immunol 102:117–122
Targoff IN, Reichlin M (1987) Measurement of antibody to Jo-1 by ELISA and comparison to enzyme inhibitory activity. J Immunol 138:2874–2882
Targoff IN (2000) Update on myositis-specific and myositis-associated autoantibodies. Curr Opin Rheumatol 12:475–481
Elkon KB, Parnassa AP, Foster CL (1985) Lupus autoantibodies target ribosomal P proteins. J Exp Med 162:459–471
Damoiseaux J, Agmon-Levin N, Van BM et al (2014) From ANA-screening to antigen-specificity: an EASI-survey on the daily practice in European countries. Clin Exp Rheumatol 32:539–546
Roggenbuck D, Borghi MO, Somma V et al (2016) Antiphospholipid antibodies detected by line immunoassay differentiate among patients with antiphospholipid syndrome, with infections and asymptomatic carriers. Arthr Res Ther 18:111
Wiik A, Cervera R, Haass M et al (2006) European attempts to set guidelines for improving diagnostics of autoimmune rheumatic disorders. Lupus 15:391–396
Hoffman IE, Peene I, Meheus L et al (2004) Specific antinuclear antibodies are associated with clinical features in systemic lupus erythematosus. Ann Rheum Dis 63:1155–1158
Arbuckle MR, McClain MT, Rubertone MV et al (2003) Development of autoantibodies before the clinical onset of systemic lupus erythematosus. N Engl J Med 349:1526–1533
Dahle C, Skogh T, Aberg AK, Jalal A, Olcen P (2004) Methods of choice for diagnostic antinuclear antibody (ANA) screening: benefit of adding antigen-specific assays to immunofluorescence microscopy. J Autoimmun 22:241–248
Kurata N, Tan EM (1976) Identification of antibodies to nuclear acidic antigens by counterimmunoelectrophoresis. Arthritis Rheum 19:574–580
Meilof JF, Bantjes I, de Jong J, Van Dam AP, Smeenk RJ (1990) The detection of anti-Ro/SS-A and anti-La/SS-B antibodies. A comparison of counterimmunoelectrophoresis with immunoblot, ELISA, and RNA-precipitation assays. J Immunol Methods 133:215–226
Lock RJ, Unsworth DJ (2001) Antibodies to extractable nuclear antigens. Has technological drift affected clinical interpretation? J Clin Pathol 54:187–190
Bizzaro N, Tozzoli R, Tonutti E et al (1998) Variability between methods to determine ANA, anti-dsDNA and anti-ENA autoantibodies: a collaborative study with the biomedical industry. J Immunol Methods 219:99–107
Mahler M (2011) Sm peptides in differentiation of autoimmune diseases. Adv Clin Chem 54:109–128
Mahler M, Fritzler MJ, Bluthner M (2005) Identification of a SmD3 epitope with a single symmetrical dimethylation of an arginine residue as a specific target of a subpopulation of anti-Sm antibodies. Arthritis Res Ther 7:R19–R29
Riemekasten G, Marell J, Hentschel C et al (2002) Casein is an essential cofactor in autoantibody reactivity directed against the C-terminal SmD1 peptide AA 83-119 in systemic lupus erythematosus. Immunobiology 206:537–545
Abeles AM, Abeles M (2013) The clinical utility of a positive antinuclear antibody test result. Am J Med 126:342–348
Bossuyt X (2009) Clinical performance characteristics of a laboratory test. A practical approach in the autoimmune laboratory. Autoimmun Rev 8:543–548
Kumar Y, Bhatia A, Minz RW (2009) Antinuclear antibodies and their detection methods in diagnosis of connective tissue diseases: a journey revisited. Diagn Pathol 4:1
Thomson KF, Murphy A, Goodfield MJ, Misbah SA (2001) Is it useful to test for antibodies to extractable nuclear antigens in the presence of a negative antinuclear antibody on Hep-2 cells? J Clin Pathol 54:413
Meroni PL, Schur PH (2010) ANA screening: an old test with new recommendations. Ann Rheum Dis 69:1420–1422
Satoh M, Tanaka S, Chan EK (2015) The uses and misuses of multiplex autoantibody assays in systemic autoimmune rheumatic diseases. Front Immunol 6:181
van der Woude FJ, Rasmussen N, Lobatto S et al (1985) Autoantibodies against neutrophils and monocytes: tool for diagnosis and marker of disease activity in Wegener’s granulomatosis. Lancet 1:425–429
Davies DJ, Moran JE, Niall JF, Ryan GB (1982) Segmental necrotising glomerulonephritis with antineutrophil antibody: possible arbovirus aetiology? Br Med J (Clin Res Ed) 285:606
Rasmussen N, Wiik A, Hoier-Madsen M, Borregaard N, van der Woude F (1988) Anti-neutrophil cytoplasm antibodies 1988. Lancet 1:706–707
Wiik A (2003) Autoantibodies in vasculitis. Arthritis Res Ther 5:147–152
Jennette JC, Falk RJ, Andrassy K et al (1994) Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum 37:187–192
Falk RJ, Gross WL, Guillevin L et al (2011) Granulomatosis with polyangiitis (Wegener’s): an alternative name for Wegener’s granulomatosis. Arthritis Rheum 63:863–864
Jennette JC, Falk RJ, Hu P, Xiao H (2013) Pathogenesis of antineutrophil cytoplasmic autoantibody-associated small-vessel vasculitis. Annu Rev Pathol 8:139–160
Jennette JC, Falk RJ (1990) Antineutrophil cytoplasmic autoantibodies and associated diseases: a review. Am J Kidney Dis 15:517–529
Falk RJ, Jennette JC (1988) Anti-neutrophil cytoplasmic autoantibodies with specificity for myeloperoxidase in patients with systemic vasculitis and idiopathic necrotizing and crescentic glomerulonephritis. N Engl J Med 318:1651–1657
Tervaert JW, Goldschmeding R, Elema JD et al (1990) Association of autoantibodies to myeloperoxidase with different forms of vasculitis. Arthritis Rheum 33:1264–1272
Savige J, Gillis D, Benson E et al (1999) International Consensus Statement on Testing and Reporting of Antineutrophil Cytoplasmic Antibodies (ANCA). Am J Clin Pathol 111:507–513
Boomsma MM, Damoiseaux JG, Stegeman CA et al (2003) Image analysis: a novel approach for the quantification of antineutrophil cytoplasmic antibody levels in patients with Wegener’s granulomatosis. J Immunol Methods 274:27–35
Rigon A, Soda P, Zennaro D, Iannello G, Afeltra A (2007) Indirect immunofluorescence in autoimmune diseases: assessment of digital images for diagnostic purpose. Cytometry B Clin Cytom 72:472–477
Sack U, Conrad K, Csernok E et al (2009) Autoantibody detection using indirect immunofluorescence on HEp-2 cells. Ann N Y Acad Sci 1173:166–173
Van Blerk M, Van Campenhout C, Bossuyt X et al (2009) Current practices in antinuclear antibody testing: results from the Belgian External Quality Assessment Scheme. Clin Chem Lab Med 47:102–108
Damoiseaux J (2013) Autoantibodies in the grocery shop: does quantity matter? Immunol Res 56:413–419
Csernok E, Holle JU (2010) Twenty-eight years with antineutrophil cytoplasmic antibodies (ANCA): how to test for ANCA - evidence-based immunology? Auto Immun Highlights 1:39–43
Joossens S, Daperno M, Shums Z et al (2004) Interassay and interobserver variability in the detection of anti-neutrophil cytoplasmic antibodies in patients with ulcerative colitis. Clin Chem 50:1422–1425
Tan EM, Smolen JS, McDougal JS et al (1999) A critical evaluation of enzyme immunoassays for detection of antinuclear autoantibodies of defined specificities. I. Precision, sensitivity, and specificity. Arthritis Rheum 42:455–464
Sollid LM, Jabri B (2013) Triggers and drivers of autoimmunity: lessons from coeliac disease. Nat Rev Immunol 13:294–302
Ludvigsson JF, Leffler DA, Bai JC et al (2012) The Oslo definitions for coeliac disease and related terms. Gut 62:43–52
Husby S, Koletzko S, Korponay-Szabo IR et al (2012) European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr 54:136–160
Salmi TT, Collin P, Korponay-Szabo IR et al (2006) Endomysial antibody-negative coeliac disease: clinical characteristics and intestinal autoantibody deposits. Gut 55:1746–1753
Chorzelski TP, Beutner EH, Sulej J et al (1984) IgA anti-endomysium antibody. A new immunological marker of dermatitis herpetiformis and coeliac disease. Br J Dermatol 111:395–402
Volta U, Villanacci V (2011) Celiac disease: diagnostic criteria in progress. Cell Mol Immunol 8:96–102
Vermeersch P, Richter T, Hauer AC et al (2011) Use of likelihood ratios improves clinical interpretation of IgG and IgA anti-DGP antibody testing for celiac disease in adults and children. Clin Biochem 44:248–250
Dieterich W, Laag E, Schopper H et al (1998) Autoantibodies to tissue transglutaminase as predictors of celiac disease. Gastroenterology 115:1317–1321
Meensel BV, Hiele M, Hoffman I et al (2004) Diagnostic accuracy of ten second-generation (human) tissue transglutaminase antibody assays in celiac disease. Clin Chem 50:2125–2135
Villalta D, Tonutti E, Prause C et al (2010) IgG antibodies against deamidated gliadin peptides for diagnosis of celiac disease in patients with IgA deficiency. Clin Chem 56:464–468
Fritzler MJ (2011) The antinuclear antibody test: last or lasting gasp? Arthritis Rheum 63:19–22
Wiik AS, Bizzaro N (2012) Missing links in high quality diagnostics of inflammatory systemic rheumatic diseases: it is all about the patient! Auto Immun Highlights 3:35–49
Coons AH, Kaplan MH (1950) Localization of antigen in tissue cells; improvements in a method for the detection of antigen by means of fluorescent antibody. J Exp Med 91:1–13
Chan EKL, Fritzler MJ, Wiik A et al (2007) AutoAbSC.Org - Autoantibody Standardization Committee in 2006. Autoimmun Rev 6:577–580
Sheldon J (2004) Laboratory testing in autoimmune rheumatic diseases. Best Pract Res Clin Rheumatol 18:249–269
Hardin JA, Lerner MR, Lerner EA, Steitz JA (1982) New directions in antinuclear antibody research: the Sm, RNP, Ro, and La antigens are found on small-RNA protein particles. Am J Kidney Dis 2:98–100
Lerner MR, Boyle JA, Hardin JA, Steitz JA (1981) Two novel classes of small ribonucleoproteins detected by antibodies associated with lupus erythematosus. Science 211:400–402
Tan EM, Smolen JS, McDougal JS et al (2002) A critical evaluation of enzyme immunoassay kits for detection of antinuclear autoantibodies of defined specificities. II. Potential for quantitation of antibody content. J Rheumatol 29:68–74
Westgeest AA, van den Brink HG, de Jong J, Swaak AJ, Smeenk RJ (1987) Antinuclear antibodies in patients with systemic lupus erythematosus: a comparison of counterimmunoelectrophoresis and immunoblotting. Rheumatol Int 7:77–82
Lerner MR, Steitz JA (1979) Antibodies to small nuclear RNAs complexed with proteins are produced by patients with systemic lupus erythematosus. Proc Natl Acad Sci U S A 76:5495
Wooley JC, Cone RD, Targoff D, Chung SY (1982) Small nuclear ribonucleoprotein complexes of Drosophila melanogaster. Proc Natl Acad Sci U S A 76:6762
Reddy R, Tan EM, Henning D, Nohga K, Busch H (1983) Detection of a nucleolar 7-2 ribonucleoprotein and cytoplasmic 8-2 ribonucleoprotein with autoantibodies from patients with scleroderma. J Biol Chem 258:1383
Hardin J, Rahn DR, Shen C, Lemer MR, Wolin SL, Rosa MD, Steitz JA (1982) Antibodies from patients with connective tissue diseases bind specific subsets of cellular RNA-protein particles. J Clin Invest 70:141
White PJ, Hoch SO (1981) Definition of the antigenic polypeptides in the Sm and RNP ribonucleoprotein complexes. Biochim Biophys Acta 102:365
Douvas AS (1982) Autoantibodies occurring in two different rheumatic diseases react with the same nuclear ribonucleoprotein particle. Proc Natl Acad Sci U S A 79:5401
Elkon KB, Culhane L (1984) Partial immunochemical characterization of the Ro and La proteins using antibodies from patients with the sicca syndrome and lupus erythematosus. J Immunol 132:2350
de Rooij DJ, van de Putte LB, Habets WJ, Verbeek AL, van Venrooij WJ (1988) The use of immunoblotting to detect antibodies to nuclear and cytoplasmic antigens. Clinical and serological associations in rheumatic diseases. Scand J Rheumatol 17:353–364
Abuaf N, Johanet C, Chretien P, Absalon BI, Homberg JC, Buri JF (1990) Detection of autoantibodies to Sm antigen in systemic lupus erythematosus by immunodiffusion, ELISA and immunoblotting: variability of incidence related to assays and ethnic origin of patients. Eur J Clin Invest 20:354–359
Brahms H, Raker VA, van Venrooij WJ, Luhrmann R (1997) A major, novel systemic lupus erythematosus autoantibody class recognizes the E, F, and G Sm snRNP proteins as an E-F-G complex but not in their denatured states. Arthritis Rheum 40:672–682
Chan EK, Francoeur AM, Tan EM (1986) Epitopes, structural domains, and asymmetry of amino acid residues in SS-B/La nuclear protein. J Immunol 136:3744–3749
Chan EK, Hamel JC, Buyon JP, Tan EM (1991) Molecular definition and sequence motifs of the 52-kD component of human SS-A/Ro autoantigen. J Clin Invest 87:68–76
Ghillani P, Andre C, Toly C et al (2011) Clinical significance of anti-Ro52 (TRIM21) antibodies non-associated with anti-SSA 60kDa antibodies: results of a multicentric study. Autoimmun Rev 10:509–513
Fritzler MJ, Wiik A, Tan EM et al (2003) A critical evaluation of enzyme immunoassay kits for detection of antinuclear autoantibodies of defined specificities. III. Comparative performance characteristics of academic and manufacturers’ laboratories. J Rheumatol 30:2374–2381
Op de Beeck K, Vermeersch P, Verschueren P et al (2011) Detection of antinuclear antibodies by indirect immunofluorescence and by solid phase assay. Autoimmun Rev 10:801–808
Rondeel JM, van Gelder W, van der Leeden H, Dinkelaar RB (1999) Different strategies in the laboratory diagnosis of autoimmune disease: immunofluorescence, enzyme-linked immunosorbent assay or both? Ann Clin Biochem 36:189–195
Landberg G, Tan EM (1994) Characterization of a DNA-binding nuclear autoantigen mainly associated with S phase and G2 cells. Exp Cell Res 212:255–261
Chan EK, Tan EM (1989) Epitopic targets for autoantibodies in systemic lupus erythematosus and Sjogren’s syndrome. Curr Opin Rheumatol 1:376–381
Wieser M, Pohla-Gubo G, Hintner H (2001) Antinuclear antibodies (ANA) Diagnostic value of different methods for screening and differentiation. Clin Appl Immunol Rev 9:201–206
Gonzalez C, Guevara P, Alarcon I, Hernando M, Navajo JA, Gonzalez-Buitrago JM (2002) Antinuclear antibodies (ANA) screening by enzyme immunoassay with nuclear HEp-2 cell extract and recombinant antigens: analytical and clinical evaluation. Clin Biochem 35:463–469
Scholz J, Grossmann K, Knütter I et al (2015) Second generation analysis of antinuclear antibody (ANA) by combination of screening and confirmatory testing. Clin Chem Lab Med 53:1991–2002
Tanaka N, Muro Y, Sugiura K, Tomita Y (2008) Anti-SS-A/Ro antibody determination by indirect immunofluorescence and comparison of different methods of anti-nuclear antibody screening: evaluation of the utility of HEp-2 cells transfected with the 60 kDa SS-A/Ro as a substrate. Mod Rheumatol 18:585–592
James K, Carpenter AB, Cook L, Marchand R, Nakamura RM (2000) Development of the antinuclear and anticytoplasmic antibody consensus panel by the Association of Medical Laboratory Immunologists. Clin Diagn Lab Immunol 7:436–443
Bossuyt X, Luyckx A (2005) Antibodies to extractable nuclear antigens in antinuclear antibody-negative samples. Clin Chem 51:2426–2427
Fritzler MJ, Miller BJ (1995) Detection of autoantibodies to SS-A/Ro by indirect immunofluorescence using a transfected and overexpressed human 60 kD Ro autoantigen in HEp-2 cells. J Clin Lab Anal 9:218–224
Scofield RH (2004) Autoantibodies as predictors of disease. Lancet 363:1544–1546
Conrad K, Ittenson A, Reinhold D, Fischer R, Roggenbuck D, Büttner T, Bosselmann HP, Steinbach J, Schössler W (2009) High sensitive detection of double-stranded DNA autoantibodies by a modified Crithidia luciliae immunofluorescence test. Ann N Y Acad Sci 1173:180–185
Roggenbuck D, Konig H, Niemann B, Schoenherr G, Jahn S, Porstmann T (1994) Real-time biospecific interaction analysis of a natural human polyreactive monoclonal IgM antibody and its Fab and scFv fragments with several antigens. Scand J Immunol 40:64–70
Sontheimer RD, Gilliam JN (1978) An immunofluorescence assay for double-stranded DNA antibodies using the Crithidia luciliae kinetoplast as a double-stranded DNA substrate. J Lab Clin Med 91:550–558
Munoz LE, Gaipl US, Herrmann M (2008) Predictive value of anti-dsDNA autoantibodies: importance of the assay. Autoimmun Rev 7:594–597
Hylkema MN, van Bruggen MC, ten Hove T et al (2000) Histone-containing immune complexes are to a large extent responsible for anti-dsDNA reactivity in the Farr assay of active SLE patients. J Autoimmun 14:159–168
Westgeest AA, van den Brink HG, de Jong J, Swaak AJ, Smeenk RJ (1988) Routine testing for antinuclear antibodies: a comparison of immunofluorescence, counterimmunoelectrophoresis and immunoblotting. J Autoimmun 1:159–170
Chiaro TR, Davis KW, Wilson A, Suh-Lailam B, Tebo AE (2011) Significant differences in the analytic concordance between anti-dsDNA IgG antibody assays for the diagnosis of systemic lupus erythematosus-Implications for inter-laboratory testing. Clin Chim Acta 412:1076–1080
Meheus L, van Venrooij WJ, Wiik A et al (1999) Multicenter validation of recombinant, natural and synthetic antigens used in a single multiparameter assay for the detection of specific anti-nuclear autoantibodies in connective tissue disorders. Clin Exp Rheumatol 17:205–214
Schmitt J, Papisch W (2002) Recombinant autoantigens. Autoimmun Rev 1:79–88
Brahms H, Raymackers J, Union A, De Keyser F, Meheus L, Luhrmann R (2000) The C-terminal RG dipeptide repeats of the spliceosomal Sm proteins D1 and D3 contain symmetrical dimethylarginines, which form a major B-cell epitope for anti-Sm autoantibodies. J Biol Chem 275:17122–17129
Schulte-Pelkum J, Fritzler M, Mahler M (2009) Latest update on the Ro/SS-A autoantibody system. Autoimmun Rev 8:632–637
Boulanger C, Chabot B, Menard HA, Boire G (1995) Autoantibodies in human anti-Ro sera specifically recognize deproteinized hY5 Ro RNA. Clin Exp Immunol 99:29–36
Csernok E, Ahlquist D, Ullrich S, Gross WL (2002) A critical evaluation of commercial immunoassays for antineutrophil cytoplasmic antibodies directed against proteinase 3 and myeloperoxidase in Wegener’s granulomatosis and microscopic polyangiitis. Rheumatology (Oxford) 41:1313–1317
Csernok E, Holle J, Hellmich B et al (2004) Evaluation of capture ELISA for detection of antineutrophil cytoplasmic antibodies directed against proteinase 3 in Wegener’s granulomatosis: first results from a multicentre study. Rheumatology (Oxford) 43:174–180
Roggenbuck D, Buettner T, Hoffmann L, Schmechta H, Reinhold D, Conrad K (2009) High-sensitivity detection of autoantibodies against proteinase-3 by a novel third-generation enzyme-linked immunosorbent assay. Ann N Y Acad Sci 1173:41–46
Damoiseaux J, Dahnrich C, Rosemann A et al (2009) A novel enzyme-linked immunosorbent assay using a mixture of human native and recombinant proteinase-3 significantly improves the diagnostic potential for antineutrophil cytoplasmic antibody-associated vasculitis. Ann Rheum Dis 68:228–233
Masuda M, Powell M, Chen S et al (2000) Autoantibodies to IA-2 in insulin-dependent diabetes mellitus. Measurements with a new immunoprecipitation assay. Clin Chim Acta 291:53–66
Kawasaki E, Yano M, Abiru N, Akazawa S, Nagataki S (1996) Detection of recombinant GAD65 and GAD67 antibodies using a simple radioimmunoassay. Diabetes Res Clin Pract 32:61–69
Bottazzo GF, Florin-Christensen A, Doniach D (1974) Islet-cell antibodies in diabetes mellitus with autoimmune polyendocrine deficiencies. Lancet 2:1279–1283
Bingley PJ, Bonifacio E, Mueller PW (2003) Diabetes Antibody Standardization Program: first assay proficiency evaluation. Diabetes 52:1128–1136
Dieterich W, Ehnis T, Bauer M et al (1997) Identification of tissue transglutaminase as the autoantigen of celiac disease. Nat Med 3:797–801
Seissler J, Wohlrab U, Wuensche C, Scherbaum WA, Boehm BO (2001) Autoantibodies from patients with coeliac disease recognize distinct functional domains of the autoantigen tissue transglutaminase. Clin Exp Immunol 125:216–221
Boire G, Lopez-Longo FJ, Lapointe S, Menard HA (1991) Sera from patients with autoimmune disease recognize conformational determinants on the 60-kd Ro/SS-A protein. Arthritis Rheum 34:722–730
Phan TG, Wong RC, Adelstein S (2002) Autoantibodies to extractable nuclear antigens: making detection and interpretation more meaningful. Clin Diagn Lab Immunol 9:1–7
Vermeersch P, Bossuyt X (2013) Prevalence and clinical significance of rare antinuclear antibody patterns. Autoimmun Rev 12:998–1003
Solomon DH, Kavanaugh AJ, Schur PH (2002) Evidence-based guidelines for the use of immunologic tests: antinuclear antibody testing. Arthritis Rheum 47:434–444
Plebani M, Pittoni M, Celadin M, Bernardi D, Mion MM (2009) Recent advances in diagnostic technologies for autoimmune diseases. Autoimmun Rev 8:238–243
Sherer Y, Gorstein A, Fritzler MJ, Shoenfeld Y (2004) Autoantibody explosion in systemic lupus erythematosus: more than 100 different antibodies found in SLE patients. Semin Arthritis Rheum 34:501–537
Van Praet JT, Van der Cruyssen B, Bonroy C, Smith V, Delanghe J, De Keyser F (2009) Validation of a new screening strategy for anti-extractable nuclear antigen antibodies. Clin Exp Rheumatol 27:971–976
Infantino M, Meacci F, Bentow C et al (2015) Clinical comparison of QUANTA Flash dsDNA chemiluminescent immunoassay with four current assays for the detection of anti-dsDNA autoantibodies. J Immunol Res 2015:902821
Mahler M, Radice A, Yang W et al (2012) Development and performance evaluation of novel chemiluminescence assays for detection of anti-PR3 and anti-MPO antibodies. Clin Chim Acta 413:719–726
Bentow C, Swart A, Wu J et al (2013) Clinical performance evaluation of a novel rapid response chemiluminescent immunoassay for the detection of autoantibodies to extractable nuclear antigens. Clin Chim Acta 424:141–147
Damoiseaux J, Boesten K, Giesen J, Austen J, Tervaert JW (2005) Evaluation of a novel line-blot immunoassay for the detection of antibodies to extractable nuclear antigens. Ann N Y Acad Sci 1050:340–347
Fritzler MJ, Fritzler ML (2006) The emergence of multiplexed technologies as diagnostic platforms in systemic autoimmune diseases. Curr Med Chem 13:2503–2512
Fritzler MJ (2006) Advances and applications of multiplexed diagnostic technologies in autoimmune diseases. Lupus 15:422–427
Hiemann R, Roggenbuck D, Sack U, Anderer U, Conrad K (2011) Die Hep-2-Zelle als Target für multiparametrische Autoantikörperanalytik - Automatisierung und Standardisierung. J Lab Med 35(6):351–361
Damoiseaux J, von Muhlen CA, Garcia-De La Torre I et al (2016) International consensus on ANA patterns (ICAP): the bumpy road towards a consensus on reporting ANA results. Auto Immun Highlights 7:1
Mahler M, Mierau R, Bluthner M (2000) Fine-specificity of the anti-CENP-A B-cell autoimmune response. J Mol Med 78:460–467
Mahler M, You D, Baron M, Taillefer SS, Hudson M, Fritzler MJ (2011) Anti-centromere antibodies in a large cohort of systemic sclerosis patients: comparison between immunofluorescence, CENP-A and CENP-B ELISA. Clin Chim Acta 412:1937–1943
Chan EKL, Damoiseaux J, Carballo OG et al (2015) Report of the first international consensus on standardized nomenclature of antinuclear antibody HEp-2 cell patterns 2014-2015. Hypothesis and Theory 6:1–13
Lee SL, Tsay GJ, Tsai RT (1993) Anticentromere antibodies in subjects with no apparent connective tissue disease. Ann Rheum Dis 52:586–589
Tozzoli R (2007) Recent advances in diagnostic technologies and their impact in autoimmune diseases. Autoimmun Rev 6:334–340
Brouwer R, Hengstman GJ, Vree EW et al (2001) Autoantibody profiles in the sera of European patients with myositis. Ann Rheum Dis 60:116–123
Caro PA, Kumble S, Kumble KD et al (2014) Evaluation of a multiplex ELISA for autoantibody profiling in patients with autoimmune connective tissue diseases. Autoimmune Dis 2014:896787
Rutgers A, Damoiseaux J, Roozendaal C, Limburg PC, Stegeman CA, Tervaert JW (2004) ANCA-GBM dot-blot: evaluation of an assay in the differential diagnosis of patients presenting with rapidly progressive glomerulonephritis. J Clin Immunol 24:435–440
Villalta D, Imbastaro T, Di GS et al (2012) Diagnostic accuracy and predictive value of extended autoantibody profile in systemic sclerosis. Autoimmun Rev 12:114–120
Bonroy C, Van Praet J, Smith V et al (2012) Optimization and diagnostic performance of a single multiparameter lineblot in the serological workup of systemic sclerosis. J Immunol Methods 379:53–60
Conrad K, Roggenbuck D, Ittenson A, Reinhold D, Buettner T, Laass MW (2012) A new dot immunoassay for simultaneous detection of celiac specific antibodies and IgA-deficiency. Clin Chem Lab Med 50:337–343
Conrad K, Schneider H, Ziemssen T et al (2007) A new line immunoassay for the multiparametric detection of antiganglioside autoantibodies in patients with autoimmune peripheral neuropathies. Ann N Y Acad Sci 1109:256–264
Roggenbuck D, Egerer K, von Landenberg P et al (2012) Antiphospholipid antibody profiling - Time for a new technical approach. Autoimmun Rev 11:821–826
Eissfeller P, Sticherling M, Scholz D et al (2005) Comparison of different test systems for simultaneous autoantibody detection in connective tissue diseases. Ann N Y Acad Sci 1050:327–339
Infantino M, Bentow C, Seaman A et al (2013) Highlights on novel technologies for the detection of antibodies to Ro60, Ro52, and SS-B. Clin Dev Immunol 2013:978202
Keijzers M, Damoiseaux J, Vigneron A et al (2015) Do associated auto-antibodies influence the outcome of myasthenia gravis after thymectomy? Autoimmunity 48:552–555
Hiemann R, Hilger N, Michel J et al (2007) Automatic analysis of immunofluorescence patterns of HEp-2 cells. Ann N Y Acad Sci 1109:358–371
Hiemann R, Buettner T, Krieger T, Roggenbuck D, Sack U, Conrad K (2009) Challenges of automated screening and differentiation of non-organ specific autoantibodies on HEp-2 cells. Autoimmun Rev 9:17–22
Rigon A, Buzzulini F, Soda P et al (2011) Novel opportunities in automated classification of antinuclear antibodies on HEp-2 cells. Autoimmun Rev 10:647–652
Nifli AP, Notas G, Mamoulaki M et al (2006) Comparison of a multiplex, bead-based fluorescent assay and immunofluorescence methods for the detection of ANA and ANCA autoantibodies in human serum. J Immunol Methods 311:189–197
Binder SR, Hixson C, Glossenger J (2006) Protein arrays and pattern recognition: new tools to assist in the identification and management of autoimmune disease. Autoimmun Rev 5:234–241
Binder SR, Genovese MC, Merrill JT, Morris RI, Metzger AL (2005) Computer-assisted pattern recognition of autoantibody results. Clin Diagn Lab Immunol 12:1353–1357
Binder SR (2006) Autoantibody detection using multiplex technologies. Lupus 15:412–421
Robinson WH, DiGennaro C, Hueber W et al (2002) Autoantigen microarrays for multiplex characterization of autoantibody responses. Nat Med 8:295–301
Fulton RJ, McDade RL, Smith PL, Kienker LJ, Kettman JR Jr (1997) Advanced multiplexed analysis with the FlowMetrix system. Clin Chem 43:1749–1756
Fritzler MJ, Fritzler ML (2009) Microbead-based technologies in diagnostic autoantibody detection. Expert Opin Med Diagn 3:81–89
Gilburd B, Abu-Shakra M, Shoenfeld Y et al (2004) Autoantibodies profile in the sera of patients with Sjogren’s syndrome: the ANA evaluation—a homogeneous, multiplexed system. Clin Dev Immunol 11:53–56
Rouquette AM, Desgruelles C, Laroche P (2003) Evaluation of the new multiplexed immunoassay, FIDIS, for simultaneous quantitative determination of antinuclear antibodies and comparison with conventional methods. Am J Clin Pathol 120:676–681
Damoiseaux J, Steller U, Buschtez M et al (2009) EUROPLUS ANCA BIOCHIP mosaic: PR3 and MPO antigen microdots improve the laboratory diagnostics of ANCA-associated vasculitis. J Immunol Methods 348:67–73
Granieri L, Marnetto F, Valentino P et al (2012) Evaluation of a multiparametric immunofluorescence assay for standardization of neuromyelitis optica serology. PLoS One 7:e38896
Russo I, Saponeri A, Peserico A, Alaibac M (2014) The use of biochip immunofluorescence microscopy for the diagnosis of Pemphigus vulgaris. Acta Histochem 116:713–716
Hanly JG, Su L, Farewell V, Fritzler MJ (2010) Comparison between multiplex assays for autoantibody detection in systemic lupus erythematosus. J Immunol Methods 358:75–80
Shovman O, Gilburd B, Barzilai O et al (2005) Evaluation of the BioPlex 2200 ANA screen: analysis of 510 healthy subjects: incidence of natural/predictive autoantibodies. Ann N Y Acad Sci 1050:380–388
Kaul R, Johnson K, Scholz H, Marr G (2009) Performance of the BioPlex 2200 Autoimmune Vasculitis kit. Autoimmun Rev 8:224–227
Zandman-Goddard G, Gilburd B, Shovman O et al (2005) The homogeneous multiplexed system - a new method for autoantibody profile in systemic lupus erythematosus. Clin Dev Immunol 12:107–111
Tozzoli R, Bonaguri C, Melegari A, Antico A, Bassetti D, Bizzaro N (2012) Current state of diagnostic technologies in the autoimmunology laboratory. Clin Chem Lab Med 51(1):1–10
Tozzoli R, Bizzaro N, Tonutti E et al (2002) Guidelines for the laboratory use of autoantibody tests in the diagnosis and monitoring of autoimmune rheumatic diseases. Am J Clin Pathol 117:316–324
Bonaguri C, Melegari A, Ballabio A et al (2011) Italian multicentre study for application of a diagnostic algorithm in autoantibody testing for autoimmune rheumatic disease: conclusive results. Autoimmun Rev 11:1–5
Copple SS, Martins TB, Masterson C, Joly E, Hill HR (2007) Comparison of three multiplex immunoassays for detection of antibodies to extractable nuclear antibodies using clinically defined sera. Ann N Y Acad Sci 1109:464–472
Copple SS, Sawitzke AD, Wilson AM, Tebo AE, Hill HR (2011) Enzyme-linked immunosorbent assay screening then indirect immunofluorescence confirmation of antinuclear antibodies: a statistical analysis. Am J Clin Pathol 135:678–684
Tozzoli R, Antico A, Porcelli B, Bassetti D (2012) Automation in indirect immunofluorescense testing: a new step in the evolution of the autoimmunology laboratory. Auto Immun Highlights 3:59–65
Villalta D, Tozzoli R, Tonutti E, Bizzaro N (2007) The laboratory approach to the diagnosis of autoimmune diseases: is it time to change? Autoimmun Rev 6:359–365
Soda P, Iannello G (2009) Aggregation of classifiers for staining pattern recognition in antinuclear autoantibodies analysis. IEEE Trans Inf Technol Biomed 13:322–329
Hiemann R, Hilger N, Sack U, Weigert M (2006) Objective quality evaluation of fluorescence images to optimize automatic image acquisition. Cytometry A 69:182–184
Willitzki A, Hiemann R, Peters V et al (2012) New platform technology for comprehensive serological diagnostics of autoimmune diseases. Clin Dev Immunol 2012:284740
Rödiger S, Schierack P, Bohm A et al (2013) A highly versatile microscope imaging technology platform for the multiplex real-time detection of biomolecules and autoimmune antibodies. Adv Biochem Eng Biotechnol 133:35–74
Roggenbuck D, Reinhold D, Hiemann R, Anderer U, Conrad K (2011) Standardized detection of anti-ds DNA antibodies by indirect immunofluorescence—a new age for confirmatory tests in SLE diagnostics. Clin Chim Acta 412:2011–2012
Roggenbuck D, Hiemann R, Bogdanos D, Reinhold D, Conrad K (2013) Standardization of automated interpretation of immunofluorescence tests. Clin Chim Acta 421C:168–169
Maenhout TM, Bonroy C, Verfaillie C, Stove V, Devreese K (2014) Automated indirect immunofluorescence microscopy enables the implementation of a quantitative internal quality control system for anti-nuclear antibody (ANA) analysis. Clin Chem Lab Med 52:989–998
Bizzaro N, Antico A, Platzgummer S et al (2014) Automated antinuclear immunofluorescence antibody screening: a comparative study of six computer-aided diagnostic systems. Autoimmun Rev 13:292–298
Voigt J, Krause C, Rohwader E et al (2012) Automated indirect immunofluorescence evaluation of antinuclear autoantibodies on HEp-2 cells. Clin Dev Immunol 2012:651058
Bonroy C, Verfaillie C, Smith V et al (2013) Automated indirect immunofluorescence antinuclear antibody analysis is a standardized alternative for visual microscope interpretation. Clin Chem Lab Med 51:1771–1779
Meroni PL, Bizzaro N, Cavazzana I, Borghi MO, Tincani A (2014) Automated tests of ANA immunofluorescence as throughput autoantibody detection technology: strengths and limitations. BMC Med 12:38
Bizzaro N, Tozzoli R, Villalta D (2015) Autoimmune diagnostics: the technology, the strategy and the clinical governance. Immunol Res 61:126–143
Egerer K, Roggenbuck D, Hiemann R et al (2010) Automated evaluation of autoantibodies on human epithelial-2 cells as an approach to standardize cell-based immunofluorescence tests. Arthritis Res Ther 12:R40
Kivity S, Gilburd B, Agmon-Levin N et al (2011) A novel automated indirect immunofluorescence autoantibody evaluation. Clin Rheumatol 31:503–9
Melegari A, Bonaguri C, Russo A, Luisita B, Trenti T, Lippi G (2012) A comparative study on the reliability of an automated system for the evaluation of cell-based indirect immunofluorescence. Autoimmun Rev 11:713–716
Gerlach S, Affeldt K, Pototzki L et al (2015) Automated evaluation of Crithidia luciliae based indirect immunofluorescence tests: a novel application of the EUROPattern-Suite technology. J Immunol Res 2015:742402
Lakos G, Gonzalez M, Flaherty D et al (2016) Detection of anti-dsDNA antibodies by computer-aided automated immunofluorescence analysis. J Immunol Methods 16:30034–5
Knütter I, Hiemann R, Brumma T et al (2012) Automated interpretation of ANCA patterns—a new approach in the serology of ANCA-associated vasculitis. Arthritis Res Ther 14:R271
Mariz HA, Sato EI, Barbosa SH, Rodrigues SH, Dellavance A, Andrade LEC (2011) Pattern on the antinuclear antibody-HEp-2 test is a critical parameter for discriminating antinuclear antibody-positive healthy individuals and patients with autoimmune rheumatic diseases. Arthritis Rheum 63:191–200
Sowa M, Großmann K, Scholz J et al (2015) The CytoBead assay—a novel approach of multiparametric autoantibody analysis in the diagnostics of systemic autoimmune diseases. J Lab Med 38(6):309–317
Grossmann K, Roggenbuck D, Schröder C, Conrad K, Schierack P, Sack U (2011) Multiplex assessment of non-organ-specific autoantibodies with a novel microbead-based immunoassay. Cytometry A 79:118–125
Sowa M, Grossmann K, Knütter I et al (2014) Simultaneous automated screening and confirmatory testing for vasculitis-specific ANCA. PLoS One 9:e107743
Grossmann K, Rober N, Hiemann R et al (2016) Simultaneous detection of celiac disease-specific IgA antibodies and total IgA. Auto Immun Highlights 7:2
Roggenbuck D, Vermeire S, Hoffman I et al (2015) Evidence of Crohn’s disease-related anti-glycoprotein 2 antibodies in patients with celiac disease. Clin Chem Lab Med 53:1349–1357
Laass MW, Rober N, Range U, Noss L, Roggenbuck D, Conrad K (2015) Loss and gain of tolerance to pancreatic glycoprotein 2 in celiac disease. PLoS One 10:e0128104
Tozzoli R, D’Aurizio F, Villalta D, Bizzaro N (2015) Automation, consolidation, and integration in autoimmune diagnostics. Auto Immun Highlights 6(1-2):1–6
Runge R, Hiemann R, Wendisch M et al (2012) Fully automated interpretation of ionizing radiation-induced gammaH2AX foci by the novel pattern recognition system AKLIDES(R). Int J Radiat Biol 88:439–447
Willitzki A, Lorenz S, Hiemann R et al (2013) Fully automated analysis of chemically induced gammaH2AX foci in human peripheral blood mononuclear cells by indirect immunofluorescence. Cytometry A 83:1017–1026
Reddig A, Lorenz S, Hiemann R et al (2015) Assessment of modulated cytostatic drug resistance by automated gammaH2AX analysis. Cytometry A 87:724–732
Wolfe F (1991) The latex test revisited. Rheumatoid factor testing in 8,287 rheumatic disease patients. Arthritis Rheum 34(8):951–960
Spiritus T, Verschueren P, Westhovens R, Bossuyt X (2004) Diagnostic characteristics of a gelatin based Waaler-Rose assay (Serodia-RA) for the detection of rheumatoid factor. Ann Rheum Dis 63:1169–1171
Hicks MJ et al (1982) Rheumatoid factor activity by rate nephelometry correlated with clinical activity in rheumatoid arthritis. Am J Clin Pathol 78(3):342–5
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sowa, M., Hiemann, R., Schierack, P. et al. Next-Generation Autoantibody Testing by Combination of Screening and Confirmation—the CytoBead® Technology. Clinic Rev Allerg Immunol 53, 87–104 (2017). https://doi.org/10.1007/s12016-016-8574-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-016-8574-3