Abstract
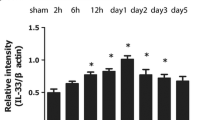
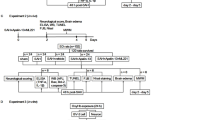
Intracerebral hemorrhage (ICH) is bleeding in brain caused by the rupture of brain blood vessel, which may lead to patient unconsciousness or death. In this study, we measured the expression of matrix metalloproteinase-9 (MMP-9) and its relevant inflammatory factors in the brain of rat with ICH. The effect of propofol on the expression of MMP-9 and inflammatory factors was investigated. We found the water content in the brain of ICH rats was significantly higher when compared with normal brain. Expression of MMP-9 and inflammatory factors IL-1β and TNF-α were up-regulated in ICH rats. Medium or high concentration of propofol can alleviate ICH in rats by inhibition of the inflammatory factor release and up-regulation of MMP-9 in brain. Our study suggests the inflammatory response after reduction of ICH through promotion of MMP-9 expression and neurite regeneration.



Similar content being viewed by others
References
van Muiswinkel, F. L., & Kuiperij, H. B. (2005). The Nrf2-ARE signalling pathway: Promising drug target to combat oxidative stress in neurodegenerative disorders. Current Drug Targets-CNS and Neurological Disorders, 4(3), 267–281.
Yang, Y. I., Estrada, E. Y., Thompson, J. F., et al. (2006). Matrix metalloproteinase-mediated disruption of tight junction proteins in cerebral vessels is reversed by synthetic matrix metalloproteinase inhibitor in focal ischemia in rat. Journal of Cerebral Blood Flow and Metabolism, 27(4), 697–709.
Carriel, V., Garzon, I., Campos, A., et al. (2014). Differential expression of MMP-9 and neurofilament during peripheral nerve regeneration through bio-artificial conduits. Journal of Tissue Engineering and Regenerative Medicine,. doi:10.1002/term.1949.
Mahajan, C., Chouhan, R. S., Rath, G. P., et al. (2014). Effect of intraoperative brain protection with propofol on postoperative cognition in patients undergoing temporary clipping during intracranial aneurysm surgery. Neurology India, 62(3), 262–268.
Chen, G., Feng, D., Zhang, L., et al. (2013). Expression of nemo-like kinase (NLK) in the brain in a rat experimental subarachnoid hemorrhage model. Cell Biochemistry and Biophysics, 66(3), 671–680.
Wu, J., Chen, J., Guo, H., et al. (2014). Effects of high-pressure oxygen therapy on brain tissue water content and AQP4 expression in rabbits with cerebral hemorrhage. Cell Biochemistry and Biophysics, 70, 1–6.
Sloan, T. B., Mongan, P., Lyda, C., et al. (2014). Lidocaine infusion adjunct to total intravenous anesthesia reduces the total dose of propofol during intraoperative neurophysiological monitoring. Journal of Clinical Monitoring and Computing, 28(2), 139–147.
Lee, K. R., Colon, G. P., Betz, A. L., et al. (1996). Edema from intracerebral hemorrhage: the role of thrombin. Journal of Neurosurgery, 84(1), 91–96.
Tanskanen, P. E., Kyttä, J. V., Randell, T. T., et al. (2006). Dexmedetomidine as an anaesthetic adjuvant in patients undergoing intracranial tumour surgery: A double-blind, randomized and placebo-controlled study. British Journal of Anaesthesia, 97(5), 658–665.
Broderick, J. P., Adams, H. P., Barsan, W., et al. (1999). Guidelines for the management of spontaneous intracerebral hemorrhage a statement for healthcare professionals from a special writing group of the Stroke council, American Heart Association. Stroke, 30(4), 905–915.
Pinaud, M., Lelausque, J. N., Chetanneau, A., et al. (1990). Effects of propofol on cerebral hemodynamics and metabolism in patients with brain trauma. Anesthesiology, 73(3), 404–409.
Karwacki, Z., Kowianski, P., Dziewiatowski, J., et al. (2006). The effect of propofol on astro- and microglial reactivity in the course of experimental intracerebral haemorrhage in rats. Folia Neuropathologica, 44(1), 50–58.
Qing, Y. U. (2013). Effect of propofol and sevoflurane anesthesia on postoperatively cognitive function of aged patients in orthopedics. Journal of Bengbu Medical College, 8, 024.
Wagner, K. R. (2014). White matter injury after experimental intracerebral hemorrhage. White matter injury in Stroke and CNS disease (pp. 219–256). New York: Springer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Han, D., Li, S., Xiong, Q. et al. Effect of Propofol on the Expression of MMP-9 and Its Relevant Inflammatory Factors in Brain of Rat with Intracerebral Hemorrhage. Cell Biochem Biophys 72, 675–679 (2015). https://doi.org/10.1007/s12013-015-0516-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-015-0516-9