Abstract
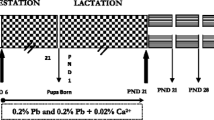
Early-life exposure to lead (Pb) can lead to health effects in later life. The neurotoxic effects of Pb have been well documented but its effects on the heart are poorly elucidated. We examined the late life cardiac impairments resulting from developmental exposure to Pb. Further, we investigated the protective effect of the nutrient metal mixture containing calcium (Ca), zinc (Zn) and iron (Fe) against Pb-induced long-term effects on cardiac functions.Male albino rats were lactationally exposed to 0.2% Pb-acetate or 0.2% Pb-acetate together nutrient metal mixture as 0.02% in drinking water of the mother from PND 1 to PND 21. The results showed increased levels of serum total cholesterol (TC), triglycerides (TG), low-density lipoproteins (LDLs) and lactate dehydrogenase (LDH) activity at postnatal day (PND) 28 [young], 4 months [adult] and 18 months [old] age group rats. Most notably, exposure to Pb decreased the activities of mitochondrial superoxide dismutase (SOD), thioredoxin reductase (TrxR), aconitase (Acon), isocitrate dehydrogenase (ICDH), xanthine oxidase (XO) and total antioxidant status while the MDA levels increased in all selected age groups of rats. The histological findings showed an age-dependent response to Pb exposure evidenced by extensive degeneration and necrosis in cardiac muscle, disruption in muscle connectivity, hemorrhage, and mononuclear cell infiltration. Co-administration of nutrient metal mixture reversed the Pb-induced cardiac impairments as reflected in the recovery of the chosen sensitive markers of oxidative stress, reduced Pb levels and cardiac tissue changes. In conclusion, the data demonstrate that early-life exposure to Pb continuously influence the cardiac mitochondrial functions from early life to older age and further suggesting that adequate intake of nutrient metals may be potential therapeutic treatment for Pb intoxication.










Similar content being viewed by others
References
Ettinger, A. S., Leonard, M. L., & Mason, J. (2019). CDC’s lead poisoning prevention program: A long-standing responsibility and commitment to protect children from lead exposure. Journal of Public Health Management and Practics,25, S5–S12.
Praveen, Sharma, Chambial, Shailja, & Shukla, Kamla Kant. (2015). Lead and neurotoxicity. Indian Journal of Clinical Biochemistry,30(1), 1–2.
Reddy, G. R., Devi, C. B., & Chetty, C. S. (2007). Developmental lead neurotoxicity: Alterations in brain cholinergic system. Neurotoxicology,28, 402–407.
Shvachiy, L., Geraldes, V., Amaro-Leal, Â., & Rocha, I. (2018). Intermittent low-level lead exposure provokes anxiety, hypertension, autonomic dysfunction and neuroinflammation. Neurotoxicology,69, 307–319.
Xu, X., Byles, J. E., Shi, Z., & Hall, J. J. (2018). Dietary patterns, dietary lead exposure and hypertension in the older Chinese population. Asia Pacific Journal of Clinical Nutrition,27(2), 451–459.
Vaziri, N. D., & Gonick, H. C. (2015). Cardiovascular effects of lead exposure. Indian Journal of Medical Research,128(4), 426–435.
Silva, M. A., de Oliveira, T. F., Almenara, C. C., Broseghini-Filho, G. B., Vassallo, D. V., Padilha, A. S., et al. (2015). Exposure to a low lead concentration impairs contractile machinery in rat cardiac muscle. Biological Trace Element Research,167(2), 280–287.
Ahmed, M. A., Khaled, M. A., & Hassanein, (2013). Cardio protective effects of Nigella sativa oil on lead induced cardio toxicity: Anti inflammatory and antioxidant mechanism. Journal of Physiol and Pathophysiol,4(5), 72–80.
Roshan, V. D., Assali, M., Moghaddam, A. H., Hosseinzadeh, M., & Myers, J. (2011). Exercise training and antioxidants: Effects on rat heart tissue exposed to lead acetate. International Journal of Toxicology,30(2), 190–196.
Basha, D. C., Basha, S. S., & Reddy, G. R. (2012). Lead-induced cardiac and hematological alterations in aging Wistar male rats: Alleviating effects of nutrient metal mixture. Biogerontology,13(4), 359–368.
Silveira, E. A., Siman, F. D., de Oliveira, F. T., Vescovi, M. V., Furieri, L. B., Lizardo, J. H., et al. (2014). Low-dose chronic lead exposure increases systolic arterial pressure and vascular reactivity of rat aortas. Free Radical Biology and Medicine,67, 366–376.
Carmignani, M., Volpe, A. R., Boscolo, P., Qiao, N., Di Gioacchino, M., Grilli, A., et al. (2000). Catcholamine and nitric oxide systems as targets of chronic lead exposure in inducing selective functional impairment. Life Sciences,68, 401–415.
Ferreira de Mattos, G., Costa, C., Savio, F., Alonso, M., & Nicolson, G. L. (2017). Lead poisoning: Acute exposure of the heart to lead ions promotes changes in cardiac function and Cav1.2 ion channels. Biophysics Reviews,9(5), 807–825.
Lanphear, B. P., Rauch, S., Auinger, P., Allen, R. W., & Hornung, R. W. (2018). Low-level lead exposure and mortality in US adults: A population-based cohort study. Lancet Public Health.,S2468–2667(18), 30025–30027.
Park, S. K., Schwartz, J., Weisskopf, M., Sparrow, D., Vokonas, P. S., Wright, R. O., et al. (2006). Low-level lead exposure, metabolic syndrome, and heart rate variability: The VA Normative Aging Study. Environmental Health Perspectives,114(11), 1718–1724.
Prasanthi, R. P., Devi, C. B., Basha, D. C., Reddy, N. S., & Reddy, G. R. (2010). Calcium and zinc supplementation protects lead (Pb)-induced perturbations in antioxidant enzymes and lipid peroxidation in developing mouse brain. International Journal of Developmental Neuroscience,28(2), 161–167.
Park, S. K., Hu, H., Wright, R. O., Schwartz, J., Cheng, Y., Sparrow, D., et al. (2009). Iron metabolism genes, low-level lead exposure, and QT interval. Environmental Health Perspectives,117(1), 80–85.
Srikanthan, T. N., & Krishnamurthi, C. R. (1955). Tetrazolium test for dehydrogenases. Journal of Scientific & Industrial Research,14, 206.
Gottipolu, R. R., Wallenborn, J. G., Karoly, E. D., Schladweiler, M. C., Ledbetter, A. D., Krantz, T., et al. (2009). One-month diesel exhaust inhalation produces hypertensive gene expression pattern in healthy rats. Environmental Health Perspectives,17, 39–46.
Manual, Worthington. (2004). Xanthine Oxidase Assay (pp. 399–401). USA: Worthington Biochemical Corporation.
Korenberg, A., & Pricer, W. E., Jr. (1951). Triphosphate pyridine nucleotide isocitric dehydrogenase in yeast. Journal of Biological Chemistry,1951(189), 123–136.
Mastanaiah, S., Chengal Raju, D., & Swami, K. S. (1978). Circadian rhythmic activity of lipase in the scorpion. Heterometrus fulvipes (C Koch). Current Science,47, 130–131.
Ohkawa, H., Ohishim, N., & Yagi, K. (1979). Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Analytical Biochemistry,95(2), 351–358.
Lowry, O. H., Rosenbrough, N. J., Farr, A. L., & Randall, R. J. (1951). Protein measurement with Folin-phenol reagent. Journal of Biological Chemistry,193, 265–275.
Chen, C., Li, Q., Nie, X., Han, B., Chen, Y., Xia, F., et al. (2017). Association of lead exposure with cardiovascular risk factors and diseases in Chinese adults. Environmental Science and Pollution Research International,24(28), 22275–22283.
An, H. C., Sung, J. H., Lee, J., Sim, C. S., Kim, S. H., & Kim, Y. (2017). The association between cadmium and lead exposure and blood pressure among workers of a smelting industry: A cross-sectional study. Annals of Occupational and Environmental Medicine,29, 47.
Steinberg, D. (2009). The LDL modification of atherogenesis: An update. Journal of Lipid Research,50, S376–S381.
Meredith, P. A., Campbell, B. C., Moore, M. R., & Goldberg, A. (1977). The effects of industrial lead poisoning on cytochrome P450 mediated phenazone (antipyrine) hydroxylation. European Journal of Clinical Pharmacology,12(3), 235–239.
Kojima, M., Masui, T., Nemoto, K., & Degawa, M. (2004). Lead nitrate-induced development of hypercholesterolemia in rats: Sterol-independent gene regulation of hepatic enzymes responsible for cholesterol homeostasis. Toxicology Letters,154(1–2), 35–44.
Ademuyiwa, O., Ugbaja, R. N., Idumebor, F., & Adebawo, O. (2005). Plasma lipid profiles and risk of cardiovascular disease in occupational lead exposure in Abeokuta, Nigeria. Lipids in Health and Diseases,4, 19.
Ranasinghe, P., Wathurapatha, W. S., Ishara, M. H., Jayawardana, R., Galappatthy, P., Katulanda, P., et al. (2015). Effects of Zinc supplementation on serum lipids: A systematic review and meta-analysis. Nutrition & Metabolism (London).,12, 26.
Ece, A., Yiğitoğlu, M. R., Vurgun, N., Güven, H., & Işcan, A. (1999). Serum lipid and lipoprotein profile in children with iron deficiency anemia. Pediatrics International,41(2), 168–173.
McIntyre, T. M., & Hazen, S. L. (2010). Lipid oxidation and cardiovascular disease: Introduction to a review series. Circulation Research,107(10), 1167–1169.
Dewanjee, S., Sahu, R., Karmakar, S., & Gangopadhyay, M. (2013). Toxic effects of lead exposure in Wistar rats: Involvement of oxidative stress and the beneficial role of edible jute (Corchorus olitorius) leaves. Food and Chemical Toxicology,55, 78–91.
Madamanchi, N. R., & Runge, M. S. (2013). Redox signaling in cardiovascular health and disease. Free Radical Biology Medicine,61, 473–501.
Raghuvanshi, R., Aikim, K., Pushpa, B., Aparna, M., & Misra, K. (2007). Xanthine oxidase as a marker of myocardial infarction. Indian Journal of Clinical Biochemistry,22(2), 90–92.
Kilikdar, D., Mukherjee, D., Mitra, E., Ghosh, A. K., Basu, A., Chandra, A. M., et al. (2011). Protective effect of aqueous garlic extract against lead-induced hepatic injury in rats. Indian Journal of Experimental Biology,49(7), 498–510.
Arif Tasleem, J., Mudsser, A., Kehkashan, S., Arif, A., Inho, C., Qazi, M., et al. (2015). Heavy metals and human health: Mechanistic insight into toxicity and counter defense system of antioxidants. International Journal of Molecular Sciences,16(12), 29592–29630.
Holmgren, A., & Lu, J. (2010). Thioredoxin and thioredoxin reductase: Current research with special reference to human disease. Biochemical and Biophysical Research Communications,396(1), 120–124.
Horstkotte, J., Perisic, T., Schneider, M., Lange, P., Schroeder, M., Kiermayer, C., et al. (2011). Mitochondrial thioredoxin reductase is essential for early postischemic myocardial protection. Circulation,124(25), 2892–2902.
Conterato, G. M., Quatrin, A., Somacal, S., Ruviaro, A. R., Vicentini, J., Augusti, P. R., et al. (2014). Acute exposure to low lead levels and its implications on the activity and expression of cytosolic thioredoxin reductase in the kidney. Basic & Clinical Pharmacology & Toxicology,114(6), 476–484.
Parildar, H., Dogru-Abbasoglu, S., Mehmetçik, G., Ozdemirler, G., Koçak-Toker, N., & Uysal, M. (2008). Lipid peroxidation potential and antioxidants in the heart tissue of beta-alanine- or taurine-treated old rats. Journal of Nutritional Science and Vitaminology (Tokyo).,54(1), 61–65.
Possamai, F. P., Júnior, S. Á., Parisotto, E. B., Moratelli, A. M., Inácio, D. B., Garlet, T. R., et al. (2010). Antioxidant intervention compensates oxidative stress in blood of subjects exposed to emissions from a coal electric-power plant in South Brazil. Environmental Toxicology and Pharmacology,30, 175–180.
Rendón-Ramírez, A. L., Maldonado-Vega, M., Quintanar-Escorza, M. A., Hernández, G., Arévalo-Rivas, B. I., Zentella-Dehesa, A., et al. (2014). Effect of vitamin E and C supplementation on oxidative damage and total antioxidant capacity in lead-exposed workers. Environmental Toxicology and Pharmacology,37(1), 45–54.
Tocchi, A., Quarles, E. K., Basisty, N., Gitari, L., & Rabinovitch, P. S. (2015). Mitochondrial dysfunction in cardiac aging. Biochimica et Biophysica Acta,1847(11), 1424–1433.
Cantu, D., Fulton, R. E., Drechsel, D. A., & Patel, M. (2011). Mitochondrial aconitase knockdown attenuates paraquat-induced dopaminergic cell death via decreased cellular metabolism and release of iron and H2O2. Journal of Neurochemistry,118(1), 79–92.
Vasquez-Vivar, J., Kalyanaraman, B., & Kennedy, M. C. (2000). Mitochondrial aconitase is a source of hydroxyl radical. An electron spin resonance investigation. Journal of Biological Chemistry,275(19), 14064–14069.
Yarian, S. C., Dikran, T., & Rajindar, S. S. (2006). Aconitase is the main functional target of aging in the citric acid cycle of kidney mitochondria from mice. Mechanisms of Ageing and Development,127(1), 79–84.
Ahamed, M., & Siddiqui, M. K. (2007). Environmental lead toxicity and nutritional factors. Clinical Nutrition,26(4), 400–408.
De Caterina, R., Zampolli, A., Del Turco, S., Madonna, R., & Massaro, M. (2006). Nutritional mechanisms that influence cardiovascular disease. American Journal of Clinical Nutrition,83(2), 421S–426S.
Mythili, Sabesan, & Malathi, Narasimhan. (2015). Diagnostic markers of acute myocardial infarction. Biomedical Reports,3(6), 743–748.
Ghosh, D., Mitra, E., Firdaus, S. B., Ghosh, K. B., Chattopadhyay, A., Pattari, K. S., et al. (2013). Melatonin protects against lead-induced cardio toxicity: Involvement of antioxidant mechanism. International Journal of Pharmacy and Pharmaceutical Sciences,5(3), 806–813.
Navas-Acien, A., Guallar, E., Silbergeld, E. K., & Rothenberg, S. J. (2007). Lead exposure and cardiovascular disease—A systematic review. Environmental Health Perspectives,115(3), 472–482.
D’Souza, H. S., Menezes, G., & Venkatesh, T. (2003). Role of essential trace minerals on the absorption of heavy metals with special reference to lead. Indian Journal of Clinical Biochemistry,18(2), 154–160.
Dorea, J. G., & Donangelo, C. M. (2006). Early (in uterus and infant) exposure to mercury and lead. Clinical Nutrition,25(3), 369–376.
Nie, H., Sánchez, B. N., Wilker, E., Weisskopf, M. G., Schwartz, J., Sparrow, D., et al. (2009). Bone lead and endogenous exposure in an environmentally exposed elderly population: thenormative aging study. Journal of Occupational and Environmental Medicine,51(7), 848–857.
Acknowledgements
This study was supported by Council of Scientific and Industrial Research (CSIR), Grant No. 37 (1349)/08/EMR-II.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Additional information
Communicated by Y. James Kang.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Davuljigari, C.B., Gottipolu, R.R. Late-life Cardiac Injury in Rats following Early Life Exposure to Lead: Reversal Effect of Nutrient Metal Mixture. Cardiovasc Toxicol 20, 249–260 (2020). https://doi.org/10.1007/s12012-019-09549-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-019-09549-2