Abstract
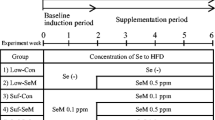
The purpose of this study is to explore the glycolytic remodeling under high-selenium (Se) stress. Three groups of male C57BL/6J mice were fed on diets with different Se contents (0.03, 0.15, and 0.30 mg Se/kg). Glucose tolerance test (GTT) and insulin tolerance test (ITT) were measured at the third month. Mice were killed at the fourth month. Plasma, liver, and muscle tissues were fetched for biochemistry and Se analysis. The expressions of insulin signaling pathway (PI3K-AKT-mTOR), glutathione peroxidase 1 (GPX1), selenoprotein N (SELENON), 3-phosphoglycerate dehydrogenase (PHGDH), serine hydroxymethyltransferases 1 (SHMT1), 5,10-methylenetetrahydrofolate reductase (MTHFR), and methionine synthase (MS) were analyzed by western blotting (WB) in liver and muscle tissues. The results of GTT and ITT showed that glucose tolerance and insulin tolerance were both abnormal in the 0.03 mg Se/kg and 0.3 mg Se/kg groups. Se concentrations in plasma, liver, and muscle of 0.03 mg Se/kg group were significantly lower than that of 0.15 mg Se/kg and 0.30 mg Se/kg groups (p < 0.05 or p < 0.01). The expressions of P-Akt (Thr-308) in muscle (p < 0.05) and PI3K and mTOR in liver (p < 0.001) of 0.30 mg Se/kg group were downregulated. The expressions of GPX1 in liver and muscle (p < 0.05 and p < 0.001), SELENON in muscle (p < 0.05), PHGDH in liver and muscle (p < 0.05), and SHMT1 (p < 0.05), MTHFR (p < 0.001), and MS (p < 0.001) in muscle of 0.3 mg Se/kg group were upregulated. The de novo serine synthesis pathway (SSP) was found to be activated in liver and muscle tissues of mice with a high-Se diet for the first time.








Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Stranges S, Marshall JR, Natarajan R, Donahue RP, Trevisan M, Combs GF et al (2007) Effects of long-term selenium supplementation on the incidence of type 2 diabetes: a randomized trial. Ann Intern Med 147(4):217–223. https://doi.org/10.7326/0003-4819-147-4-200708210-00175
Lippman SM, Klein EA, Goodman PJ, Lucia MS, Thompson IM, Ford LG et al (2009) Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA 301(1):39–51. https://doi.org/10.1001/jama.2008.864. (Epub 2008 Dec 9)
Vinceti M, Filippini T, Rothman KJ (2018) Selenium exposure and the risk of type 2 diabetes: a systematic review and meta-analysis. Eur J Epidemiol 33(9):789–810. https://doi.org/10.1007/s10654-018-0422-8
Kim J, Chung HS, Choi MK, Roh YK, Yoo HJ, Park JH, Kim DS, Yu JM, Moon S (2019) Association between serum selenium level and the presence of diabetes mellitus: a meta-analysis of observational studies. Diabetes Metab J 43(4):447–460. https://doi.org/10.4093/dmj.2018.0123
Vinceti M, Filippini T, Wise LA, Rothman KJ (2021) A systematic review and dose-response meta-analysis of exposure to environmental selenium and the risk of type 2 diabetes in nonexperimental studies. Environ Res 197:111210. https://doi.org/10.1016/j.envres.2021.111210
Hoque B, Shi Z (2022) Association between selenium intake, diabetes and mortality in adults: findings from National Health and Nutrition Examination Survey (NHANES) 2003–2014. Br J Nutr 127(7):1098–1105. https://doi.org/10.1017/S000711452100177X
Moon S, Chung HS, Yu JM, Yoo HJ, Park JH, Kim DS et al (2019) Association between serum selenium level and the prevalence of diabetes mellitus in U.S. population. J Trace Elem Med Biol 52:83–88. https://doi.org/10.1016/j.jtemb.2018.12.005
Cardoso BR, Braat S, Graham RM (2021) Selenium status is associated with insulin resistance markers in adults: findings from the 2013 to 2018 National Health and Nutrition Examination Survey (NHANES). Front Nutr 8:696024. https://doi.org/10.3389/fnut.2021.696024
McClung JP, Roneker CA, Mu W, Lisk DJ, Langlais P, Liu F, Lei XG (2004) Development of insulin resistance and obesity in mice overexpressing cellular glutathione peroxidase. Proc Natl Acad Sci U S A 101(24):8852–7. https://doi.org/10.1073/pnas.0308096101
Yan X, Pepper MP, Vatamaniuk MZ, Roneker CA, Li L, Lei XG (2012) Dietary selenium deficiency partially rescues type 2 diabetes-like phenotypes of glutathione peroxidase-1-overexpressing male mice. J Nutr 142(11):1975–82. https://doi.org/10.3945/jn.112.164764
Takeshita Y, Ota T, Sakurai M, Yamashita T, Mizukoshi E, Yamashita T et al (2010) A liver-derived secretory protein, selenoprotein P, causes insulin resistance. Cell Metab 12(5):483–495. https://doi.org/10.1016/j.cmet.2010.09.015
Mita Y, Nakayama K, Inari S, Nishito Y, Yoshioka Y, Sakai N et al (2017) Selenoprotein P-neutralizing antibodies improve insulin secretion and glucose sensitivity in type 2 diabetes mouse models. Nat Commun 8(1):1658. https://doi.org/10.1038/s41467-017-01863-z
Labunskyy VM, Lee BC, Handy DE, Loscalzo J, Hatfield DL, Gladyshev VN (2011) Both maximal expression of selenoproteins and selenoprotein deficiency can promote development of type 2 diabetes-like phenotype in mice. Antioxid Redox Signal 14(12):2327–2336. https://doi.org/10.1089/ars.2010.3526
Zeng MS, Li X, Liu Y, Zhao H, Zhou JC, Li K et al (2012) A high-selenium diet induces insulin resistance in gestating rats and their offspring. Free Radic Biol Med 52(8):1335–42. https://doi.org/10.1016/j.freeradbiomed
Wang XD, Vatamaniuk MZ, Wang SK, Roneker CA, Simmons RA, Lei XG (2008) Molecular mechanisms for hyperinsulinaemia induced by overproduction of selenium-dependent glutathione peroxidase-1 in mice. Diabetologia 51(8):1515–24. https://doi.org/10.1007/s00125-008-1055-3
Huang JQ, Zhou JC, Wu YY, Ren FZ, Lei XG (2018) Role of glutathione peroxidase 1 in glucose and lipid metabolism- related diseases. Free Radic Biol Med 127:108–115. https://doi.org/10.1016/j.freeradbiomed.2018.05.077
Yun JW, Zhao Z, Yan X, Vatamaniuk MZ, Lei XG (2019) Glutathione peroxidase-1 inhibits transcription of regenerating islet-derived protein-2 in pancreatic islets. Free Radic Biol Med 134:385–393. https://doi.org/10.1016/j.freeradbiomed.2019.01.024
Steinbrenner H, Duntas LH, Rayman MP (2022) The role of selenium in type-2 diabetes mellitus and its metabolic comorbidities. Redox Biol 50:102236. https://doi.org/10.1016/j.redox.2022.102236
Zhan S (2021) The preliminary study of glycolytic remodeling in different cells under high-selenium stress. Dissertation, Chinese Center for Disease Control and Prevention, China
Yan X, Pepper MP, Vatamaniuk MZ, Roneker CA, Li L, Lei XG (2012) Dietary selenium deficiency partially rescues type 2 diabetes-like phenotypes of glutathione peroxidase-1-overexpressing male mice. J Nutr 142(11):1975–1982. https://doi.org/10.3945/jn.112.164764
Misu H, Takamura T, Takayama H, Hayashi H, Matsuzawa-Nagata N, Kurita S et al (2010) A liver-derived secretory protein, selenoprotein P, causes insulin resistance. Cell Metab 12(5):483–495. https://doi.org/10.1016/j.cmet.2010.09.015
Chaudière J (2023) Biological and catalytic properties of selenoproteins. Int J Mol Sci 24(12):10109. https://doi.org/10.3390/ijms241210109
Zhao J, Zou H, Huo Y, Wei X, Li Y (2022) Emerging roles of selenium on metabolism and type 2 diabetes. Front Nutr 9:1027629. https://doi.org/10.3389/fnut.2022.1027629
Lennicke C, Cochemé HM (2021) Redox regulation of the insulin signalling pathway. Redox Biol 42:101964. https://doi.org/10.1016/j.redox.2021.101964
Xirouchaki CE, Jia YY, McGrath MJ, Greatorex S, Tran M, Merry TL et al (2021) Skeletal muscle NOX4 is required for adaptive responses that prevent insulin resistance. Sci Adv 7(51):eabl4988. https://doi.org/10.1126/sciadv.abl4988
Fonseca TL, Werneck-De-Castro JP, Castillo M et al (2014) Tissue-specific inactivation of type 2 deiodinase reveals multilevel control of fatty acid oxidation by thyroid hormone in the mouse. Diabetes 63(5):1594–1604. https://doi.org/10.2337/db13-1768
Wang Q, Zhan S, Han F, Liu YQ, Wu HY, Huang ZW (2022) The possible mechanism of physiological adaptation to the low-Se diet and its health risk in the traditional endemic areas of Keshan disease. Biol Trace Elem Res 200(5):2069–2083. https://doi.org/10.1007/s12011-021-02851-7
Wang Q, Sun LC, Liu YQ, Lu JX, Han F, Huang ZW (2016) The synergistic effect of serine with selenocompounds on the expression of SELENOP and GPX in HepG2 cells. Biol Trace Elem Res 173(2):291–6. https://doi.org/10.1007/s12011-016-0665-8
Zhan S, Liu YQ, Han F, Wang Q, Huang ZW (2021) Effects of selenomethionine on the expressions of selenoproteins in hepatocytes L02 and the synergistic effect of serine. J Hyg Res 50(1):100–103
Liu YQ, Wang JR, Wang Q, Han F, Shi LL, Chao Han C, Huang ZW, Xu L (2022) Effects of insufficient serine on health and selenoprotein expression in rats and their offspring. Front Nutr 14(9):1012362. https://doi.org/10.3389/fnut.2022.1012362
Long J, Liu Y, Zhou X, He L (2021) Dietary serine supplementation regulates selenoprotein transcription and selenoenzyme activity in pigs. Biol Trace Elem Res 199(1):148–153. https://doi.org/10.1007/s12011-020-02117-8
Zhou L, Feng Y, Liu Y, He L, Zhou X, Yin Y (2022) Serine supplementation in the diets of late gestating and lactating sows improves selenium nutritional status in sows and their offspring. Biol Trace Elem Res 200(2):609–614. https://doi.org/10.1007/s12011-021-02661-x
Han F, Pang X, Wang Q, Liu YQ, Liu LP, Chai YJ et al (2021) Dietary serine and sulfate-containing amino acids related to the nutritional status of selenium in lactating Chinese women. Biol Trace Elem Res 199(3):829–841. https://doi.org/10.1007/s12011-020-02204-w
Holeček M (2023) Role of impaired glycolysis in perturbations of amino acid metabolism in diabetes mellitus. Int J Mol Sci 24(2):1724. https://doi.org/10.3390/ijms24021724
Possemato R, Marks KM, Shaul YD, Pacold ME, Kim D, Birsoy K et al (2011) Functional genomics reveal that the serine synthesis pathway is essential in breast cancer. Nature 476(7360):346–50. https://doi.org/10.1038/nature10350
Furuya S (2008) An essential role for de novo biosynthesis of L-serine in CNS development. Asia Pac J Clin Nutr 17(Suppl 1):312–315
Zhang X, Wang J, Wang Q, Han F, Xiang X, Liu Y et al (2023) Study of high selenium interfering with glucose and one-carbon metabolism in hepatocytes in vitro. J Hyg Res 52(1):115–118 (in Chinese)
Tabatabaie L, Klomp LW, Berger R, de Koning TJ (2010) L-serine synthesis in the central nervous system: a review on serine deficiency disorders. Mol Genet Metab 99(3):256–262. https://doi.org/10.1016/j.ymgme
Wood PL, Hawkinson JE, Goodnough DB (1996) Formation of D-serine from L-phosphoserine in brain synaptosomes. J Neurochem 67(4):1485–1490. https://doi.org/10.1046/j.1471-4159
Fan TWM, Bruntz RC, Yang Y, Song H, Chernyavskaya Y, Deng P (2019) De novo synthesis of serine and glycine fuels purine nucleotide biosynthesis in human lung cancer tissues. J Biol Chem 294(36):13464–13477. https://doi.org/10.1074/jbc.RA119.008743
Nakamizo A, Miyamatsu Y, Hirose H, Amano T, Matsuo S, Fujiwara M et al (2022) Metabolic remodeling of pyrimidine synthesis pathway and serine synthesis pathway in human glioblastoma. Sci Rep 12(1):16277. https://doi.org/10.1038/s41598-022-20613-w
Truman JP, Ruiz CF, Montal E, Garcia-Barros M, Mileva I, Snider AJ et al (2022) 1-Deoxysphinganine initiates adaptive responses to serine and glycine starvation in cancer cells via proteolysis of sphingosine kinase. J Lipid Res 63(1):100154. https://doi.org/10.1016/j.jlr.2021.100154
Muthusamy T, Cordes T, Handzlik MK, You L, Lim EW, Gengatharan J et al (2020) Serine restriction alters sphingolipid diversity to constrain tumor growth. Nature 586(7831):790–795. https://doi.org/10.1038/s41586-020-2609-x
Kang YP, Falzone A, Liu M, González-Sánchez P, Choi BH, Coloff JL et al (2020) PHGDH supports liver ceramide synthesis and sustains lipid homeostasis. Cancer Metab 15(8):6. https://doi.org/10.1186/s40170-020-00212-x
Cordes T, Kuna RS, McGregor GH, Khare SV, Gengatharan J, Muthusamy T et al (2022) 1-Deoxysphingolipid synthesis compromises anchorage-independent growth and plasma membrane endocytosis in cancer cells. J Lipid Res 63(10):100281. https://doi.org/10.1016/j.jlr.2022.100281
Nigdelioglu R, Hamanaka RB, Meliton AY, O’Leary E, Witt LJ, Cho T et al (2016) Transforming growth factor (TGF)-beta promotes de novo serine synthesis for collagen production. J Biol Chem 291(53):27239–27251. https://doi.org/10.1074/jbc.M116.756247
O’Leary EM, Tian Y, Nigdelioglu R, Witt LJ, Cetin-Atalay R, Meliton AY et al (2020) TGF-beta promotes metabolic reprogramming in lung fibroblasts via mTORC1-dependent ATF4 activation. Am J Respir Cell Mol Biol 63(5):601–612. https://doi.org/10.1165/rcmb.2020-0143OC
Ma EH, Bantug G, Griss T, Condotta S, Johnson RM, Samborska B et al (2017) Serine is an essential metabolite for effector T cell expansion. Cell Metab 25(2):345–357. https://doi.org/10.1016/j.cmet.2016.12.011
Ma EH, Verway MJ, Johnson RM, Roy DG, Steadman M, Hayes S et al (2019) Metabolic profiling using stable isotope tracing reveals distinct patterns of glucose utilization by physiologically activated CD8(+) T cells. Immunity 51(5):856–870. https://doi.org/10.1016/j.immuni.2019.09.003
Mak TW, Grusdat M, Duncan GS, Dostert C, Nonnenmacher Y, Cox M et al (2017) Glutathione primes T Cell metabolism for inflammation. Immunity 46(4):675–689. https://doi.org/10.1016/j.immuni.2017.03.019
Yu W, Wang Z, Zhang K, Chi Z, Xu T, Jiang DL et al (2019) One-carbon metabolism supports S-adenosylmethionine and histone methylation to drive inflammatory macrophages. Mol Cell 75(6):1147–1160. https://doi.org/10.1016/j.molcel.2019.06.039
Shen L, Hu P, Zhang Y, Ji Z, Shan X, Ni L et al (2021) Serine metabolism antagonizes antiviral innate immunity by preventing ATP6V0d2-mediated YAP lysosomal degradation. Cell Metab 33(5):971–987. https://doi.org/10.1016/j.cmet.2021.03.006
Shan X, Hu P, Ni L, Shen L, Zhang Y, Ji Z et al (2022) Serine metabolism orchestrates macrophage polarization by regulating the IGF1-p38 axis. Cell Mol Immunol 19(11):1263–1278. https://doi.org/10.1038/s41423-022-00925-7
Natoli G, Pileri F, Gualdrini F, Ghisletti S (2021) Integration of transcriptional and metabolic control in macrophage activation. EMBO Rep 22(9):e53251. https://doi.org/10.15252/embr.202153251
Forgione MA, Weiss N, Heydrick S, Cap A, Klings ES, Bierl C et al (2002) Cellular glutathione peroxidase deficiency and endothelial dysfunction. Am J Physiol Heart Circ Physiol 282(4):H1255-61. https://doi.org/10.1152/ajpheart.00598.2001
Fridman V, Zarini S, Sillau S, Harrison K, Bergman BC, Feldman EL et al (2021) Altered plasma serine and 1-deoxydihydroceramide profiles are associated with diabetic neuropathy in type 2 diabetes and obesity. J Diabetes Complicat 35(4):107852. https://doi.org/10.1016/j.jdiacomp.2021.107852
Funding
This work was supported by the National Natural Science Foundation of China under Grant No. 81973048.
Author information
Authors and Affiliations
Contributions
Zhenwu Huang and Qin Wang designed research; Qin Wang, Xue Zhang, and Jianrong Wang conducted laboratory works; Qin Wang, Yiqun Liu, and Feng Han analyzed data; Qin Wang wrote the original manuscript. Xuesong Xiang and Yanbin Guo gave helpful comments. Zhenwu Huang is responsible for the contents of the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Q., Wang, J., Zhang, X. et al. Increased Expression of PHGDH Under High-Selenium Stress In Vivo. Biol Trace Elem Res (2024). https://doi.org/10.1007/s12011-024-04079-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12011-024-04079-7