Abstract
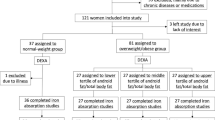
Iron overload is associated with type 2 diabetes and metabolic syndrome. However, little is known about the role of iron status on adipose tissue. We aimed to investigate the association of iron metabolism markers with adipose tissue dysfunction-related indices in obese individuals. A total of 226 obese adults with body mass index (BMI) ≥ 30 kg/m2 were recruited into the study. Hemoglobin, serum ferritin, iron, soluble transferrin receptor (sTfR), total iron-binding capacity (TIBC), transferrin saturation (TSAT), and other clinical parameters were measured. Adipose tissue dysfunction was assessed by adipose tissue insulin resistance (adipose-IR), visceral adiposity index (VAI), and lipid accumulation product (LAP) index. Serum ferritin levels, adipose-IR, and VAI progressively increased from class I to class III obesity and significantly higher in class III obesity. Correlation analysis suggested that only serum ferritin levels were positively correlated with adipose-IR (r = 0.284, P < 0.001), VAI (r = 0.209, P = 0.002), and LAP (r = 0.324, P < 0.001). Moreover, further logistic regression analysis revealed serum ferritin was significantly associated with elevated adipose-IR, VAI, and LAP. After adjustment for potential confounders, serum ferritin levels remained independently associated with elevated adipose-IR (OR = 1.004, 95% CI 1.000–1.009, P < 0.05) and VAI (OR = 1.005, 95% CI 1.001–1.009, P < 0.05). Serum ferritin was associated with elevated adipose-IR, VAI, and LAP, suggesting that ferritin could be an important early indicator for the risk of developing adipose tissue dysfunction in obese individuals.

Similar content being viewed by others
Data Availability
Some or all datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Flegal KM, Kit BK, Orpana H, Graubard BI (2013) Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 309:71–82. https://doi.org/10.1001/jama.2012.113905
Kahn SE, Hull RL, Utzschneider KM (2006) Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444:840–846. https://doi.org/10.1038/nature05482
Speakman JR, Hall KD (2021) Carbohydrates, insulin, and obesity. Science 372:577–578. https://doi.org/10.1126/science.aav0448
Scherer PE (2006) Adipose tissue: from lipid storage compartment to endocrine organ. Diabetes 55:1537–1545. https://doi.org/10.2337/db06-0263
Neeland IJ, Poirier P, Després JP (2018) Cardiovascular and metabolic heterogeneity of obesity: clinical challenges and implications for management. Circulation 137:1391–1406. https://doi.org/10.1161/circulationaha.117.029617
Jensen MD, Haymond MW, Rizza RA, Cryer PE, Miles JM (1989) Influence of body fat distribution on free fatty acid metabolism in obesity. J Clin Invest 83:1168–1173. https://doi.org/10.1172/jci113997
Burns SF, Kelsey SF, Arslanian SA (2009) Effects of an intravenous lipid challenge and free fatty acid elevation on in vivo insulin sensitivity in African American versus Caucasian adolescents. Diabetes Care 32:355–360. https://doi.org/10.2337/dc08-1102
Sharma RB, Alonso LC (2014) Lipotoxicity in the pancreatic beta cell: not just survival and function, but proliferation as well? Curr Diab Rep 14:492. https://doi.org/10.1007/s11892-014-0492-2
Prentki M, Peyot ML, Masiello P, Madiraju SRM (2020) Nutrient-induced metabolic stress, adaptation, detoxification, and toxicity in the pancreatic β-cell. Diabetes 69:279–290. https://doi.org/10.2337/dbi19-0014
Simcox JA, McClain DA (2013) Iron and diabetes risk. Cell Metab 17:329–341. https://doi.org/10.1016/j.cmet.2013.02.007
Yi KH, Hwang JS, Lim SW, Lee JA, Kim DH, Lim JS (2016) Ferritin level is associated with metabolic syndrome and elevated alanine aminotransferase in children and adolescents. J Pediatr Endocrinol Metab 29:1337–1344. https://doi.org/10.1515/jpem-2016-0045
Akter S, Nanri A, Kuwahara K, Matsushita Y, Nakagawa T, Konishi M, Honda T, Yamamoto S, Hayashi T, Noda M, Mizoue T (2017) Circulating ferritin concentrations and risk of type 2 diabetes in Japanese individuals. J Diabetes Investig 8:462–470. https://doi.org/10.1111/jdi.12617
Zhang J, Cao J, Xu H, Dong G, Huang K, Wu W, Ye J, Fu J (2021) Ferritin as a key risk factor for nonalcoholic fatty liver disease in children with obesity. J Clin Lab Anal 35:e23602. https://doi.org/10.1002/jcla.23602
Başar Gökcen B, Akdevelioğlu Y, Canan S, Bozkurt N (2021) Evaluation of the relationship between serum ferritin and insulin resistance and visceral adiposity index (VAI) in women with polycystic ovary syndrome. Eat Weight Disord 26:1581–1593. https://doi.org/10.1007/s40519-020-00980-x
Chakraborty B, Vishnoi G, Goswami B, Gowda SH, Chowdhury D, Agarwal S (2013) Lipoprotein(a), ferritin, and albumin in acute phase reaction predicts severity and mortality of acute ischemic stroke in North Indian Patients. J Stroke Cerebrovasc Dis 22:e159-167. https://doi.org/10.1016/j.jstrokecerebrovasdis.2012.10.013
Zhang Z, Funcke JB, Zi Z, Zhao S, Straub LG, Zhu Y, Zhu Q, Crewe C, An YA, Chen S, Li N, Wang MY, Ghaben AL, Lee C, Gautron L, Engelking LJ, Raj P, Deng Y, Gordillo R, Kusminski CM, Scherer PE (2021) Adipocyte iron levels impinge on a fat-gut crosstalk to regulate intestinal lipid absorption and mediate protection from obesity. Cell Metab 33:1624-1639.e1629. https://doi.org/10.1016/j.cmet.2021.06.001
World Heath Organisation (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:i-xii, 1–253.
Groop LC, Bonadonna RC, DelPrato S, Ratheiser K, Zyck K, Ferrannini E, DeFronzo RA (1989) Glucose and free fatty acid metabolism in non-insulin-dependent diabetes mellitus. Evidence for multiple sites of insulin resistance. J Clin Invest 84:205–213. https://doi.org/10.1172/jci114142
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419. https://doi.org/10.1007/bf00280883
Simental-Mendía L, Rodríguez-Morán M, Guerrero-Romero F (2008) The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord 6:299–304. https://doi.org/10.1089/met.2008.0034
Amato MC, Giordano C (2014) Visceral adiposity index: an indicator of adipose tissue dysfunction. Int J Endocrinol 2014:730827. https://doi.org/10.1155/2014/730827
Kahn HS (2005) The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disord 5:26. https://doi.org/10.1186/1471-2261-5-26
Koenen M, Hill MA, Cohen P, Sowers JR (2021) Obesity, adipose tissue and vascular dysfunction. Circ Res 128:951–968. https://doi.org/10.1161/circresaha.121.318093
Funcke JB, Scherer PE (2019) Beyond adiponectin and leptin: adipose tissue-derived mediators of inter-organ communication. J Lipid Res 60:1648–1684. https://doi.org/10.1194/jlr.R094060
Semnani-Azad Z, Connelly PW, Bazinet RP, Retnakaran R, Jenkins DJA, Harris SB, Zinman B, Hanley AJ (2021) Adipose tissue insulin resistance is longitudinally associated with adipose tissue dysfunction, circulating lipids, and dysglycemia: the PROMISE cohort. Diabetes Care 44:1682–1691. https://doi.org/10.2337/dc20-1918
Gao Y, Li Z, Gabrielsen JS, Simcox JA, Lee SH, Jones D, Cooksey B, Stoddard G, Cefalu WT, McClain DA (2015) Adipocyte iron regulates leptin and food intake. J Clin Invest 125:3681–3691. https://doi.org/10.1172/jci81860
Gabrielsen JS, Gao Y, Simcox JA, Huang J, Thorup D, Jones D, Cooksey RC, Gabrielsen D, Adams TD, Hunt SC, Hopkins PN, Cefalu WT, McClain DA (2012) Adipocyte iron regulates adiponectin and insulin sensitivity. J Clin Invest 122:3529–3540. https://doi.org/10.1172/jci44421
Wlazlo N, van Greevenbroek MM, Ferreira I, Jansen EH, Feskens EJ, van der Kallen CJ, Schalkwijk CG, Bravenboer B, Stehouwer CD (2013) Iron metabolism is associated with adipocyte insulin resistance and plasma adiponectin: the Cohort on Diabetes and Atherosclerosis Maastricht (CODAM) study. Diabetes Care 36:309–315. https://doi.org/10.2337/dc12-0505
Hitha H, Gowda D, Mirajkar A (2018) Serum ferritin level as an early indicator of metabolic dysregulation in young obese adults - a cross-sectional study. Can J Physiol Pharmacol 96:1255–1260. https://doi.org/10.1139/cjpp-2018-0433
Tajima S, Ikeda Y, Sawada K, Yamano N, Horinouchi Y, Kihira Y, Ishizawa K, Izawa-Ishizawa Y, Kawazoe K, Tomita S, Minakuchi K, Tsuchiya K, Tamaki T (2012) Iron reduction by deferoxamine leads to amelioration of adiposity via the regulation of oxidative stress and inflammation in obese and type 2 diabetes KKAy mice. Am J Physiol Endocrinol Metab 302:E77-86. https://doi.org/10.1152/ajpendo.00033.2011
Rumberger JM, Peters T Jr, Burrington C, Green A (2004) Transferrin and iron contribute to the lipolytic effect of serum in isolated adipocytes. Diabetes 53:2535–2541. https://doi.org/10.2337/diabetes.53.10.2535
Homko CJ, Cheung P, Boden G (2003) Effects of free fatty acids on glucose uptake and utilization in healthy women. Diabetes 52:487–491. https://doi.org/10.2337/diabetes.52.2.487
Pihan-Le Bars F, Bonnet F, Loréal O, Le Loupp AG, Ropert M, Letessier E, Prieur X, Bach K, Deugnier Y, Fromenty B, Cariou B (2016) Indicators of iron status are correlated with adiponectin expression in adipose tissue of patients with morbid obesity. Diabetes Metab 42:105–111. https://doi.org/10.1016/j.diabet.2015.10.007
Schrover IM, Spiering W, Leiner T, Visseren FL (2016) Adipose tissue dysfunction: clinical relevance and diagnostic possibilities. Horm Metab Res 48:213–225. https://doi.org/10.1055/s-0042-103243
Moore Heslin A, O’Donnell A, Buffini M, Nugent AP, Walton J, Flynn A, McNulty BA (2021) Risk of iron overload in obesity and implications in metabolic health. Nutrients 13:1539. https://doi.org/10.3390/nu13051539
Skikne BS, Flowers CH, Cook JD (1990) Serum transferrin receptor: a quantitative measure of tissue iron deficiency. Blood 75:1870–1876. https://doi.org/10.1182/blood.V75.9.1870.1870
Abumrad NA, Davidson NO (2012) Role of the gut in lipid homeostasis. Physiol Rev 92:1061–1085. https://doi.org/10.1152/physrev.00019.2011
Mayneris-Perxachs J, Cardellini M, Hoyles L, Latorre J, Davato F, Moreno-Navarrete JM, Arnoriaga-Rodríguez M, Serino M, Abbott J, Barton RH, Puig J, Fernández-Real X, Ricart W, Tomlinson C, Woodbridge M, Gentileschi P, Butcher SA, Holmes E, Nicholson JK, Pérez-Brocal V, Moya A, Clain DM, Burcelin R, Dumas ME, Federici M, Fernández-Real JM (2021) Iron status influences non-alcoholic fatty liver disease in obesity through the gut microbiome. Microbiome 9:104. https://doi.org/10.1186/s40168-021-01052-7
Acknowledgements
We thank the staff and colleagues at the Endocrinology Department of Beijing Chao-yang Hospital.
Funding
This work was supported by grants from Beijing Natural Science Foundation (Z200019) to Jia Liu.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Xiaoyu Ding performed formal analysis and wrote the manuscript. Study design, material preparation, and data collection were performed by Xiaoyu Ding, Nannan Bian, Jiaxuan Wang, Xiaona Chang, and Yu An. The paper was revised by Jia Liu and Guang Wang. All authors read and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki and approved by the Medical Ethics Committee of Beijing Chao-yang Hospital of Capital Medical University.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ding, X., Bian, N., Wang, J. et al. Serum Ferritin Levels Are Associated with Adipose Tissue Dysfunction-Related Indices in Obese Adults. Biol Trace Elem Res 201, 636–643 (2023). https://doi.org/10.1007/s12011-022-03198-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-022-03198-3