Abstract
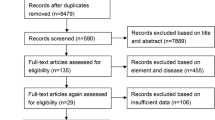
Trace elements are essentially required for various physiological and metabolic functions, and any disturbance in the trace elements homeostasis may result in the development of chronic diseases including breast cancer. Breast cancer is the most prevalent cancer type reported in women equally affecting both the high-income and low-income countries. This review therefore aimed to evaluate the impact of dietary trace element intake in relation to the incidence of breast cancer. We focused on five trace elements, thus emphasizing dietary selenium, zinc, iron, copper, and cadmium intake and risk of breast cancer. A systematic approach was applied to perform this review through entering a search term in PubMed and Scopus databases. A total of 24 articles were included after meeting the inclusion and exclusion criteria. Most of the studies regarding dietary iron intake showed a detrimental effect of increased dietary heme iron on breast cancer incidence risk. In addition, there is a limited evidence of high dietary intake of selenium and zinc to reduce the risk of breast cancer. Also, a few studies showed a relationship between high cadmium consumption and risk of breast cancer. More studies related to cadmium and copper exposure are needed to confirm this relationship. As a result, the findings of this review suggested that high dietary heme iron is a potential risk factor for breast cancer.

Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Malvezzi M, Carioli G, Bertuccio P et al (2019) European cancer mortality predictions for the year 2019 with focus on breast cancer. Ann Oncol 30:781–787. https://doi.org/10.1093/annonc/mdz051
Akram M, Iqbal M, Daniyal M, Khan AU (2017) Awareness and current knowledge of breast cancer. Biol Res 50:33. https://doi.org/10.1186/s40659-017-0140-9
MacMahon B (2006) Epidemiology and the causes of breast cancer. Int J Cancer 118:2373–2378. https://doi.org/10.1002/ijc.21404
Cabré N, Luciano-Mateo F, Arenas M et al (2018) Trace element concentrations in breast cancer patients. Breast 42:142–149. https://doi.org/10.1016/j.breast.2018.09.005
Choi R, Kim MJ, Sohn I et al (2019) Serum trace elements and their associations with breast cancer subgroups in Korean breast cancer patients. Nutrients 11:1–15. https://doi.org/10.3390/nu11010037
Lossow K, Schwarz M, Kipp AP (2021) Are trace element concentrations suitable biomarkers for the diagnosis of cancer? Redox Biol 42:101900. https://doi.org/10.1016/j.redox.2021.101900
Tehrani SS, Hosseini MH, Yousefi T et al (2019) The crosstalk between trace elements with DNA damage response, repair, and oxidative stress in cancer. J Cell Biochem 120:1080–1105. https://doi.org/10.1002/jcb.27617
Wadhwa SK, Kazi TG, Afridi HI, Talpur FN (2015) Interaction between carcinogenic and anti-carcinogenic trace elements in the scalp hair samples of different types of Pakistani female cancer patients. Clin Chim Acta 439:178–184. https://doi.org/10.1016/j.cca.2014.10.007
Grattan BJ, Freake HC (2012) Zinc and cancer: implications for LIV-1 in breast cancer. Nutrients 4:648–675. https://doi.org/10.3390/nu4070648
Maret W, Sandstead HH (2006) Zinc requirements and the risks and benefits of zinc supplementation. J Trace Elem Med Biol 20:3–18. https://doi.org/10.1016/j.jtemb.2006.01.006
Otten JJ, Hellwig JP, Linda D (2006) Dietary DRI reference intakes: the essential guide to nutrient requirements. THE NATIONAL ACADEMIES PRESS, Washington, DC
EFSA Nda Panel (2014) Scientific opinion on dietary reference values for zinc. EFSA J 12:1–76. https://doi.org/10.2903/j.efsa.2014.3844
Rayman MP (2005) Selenium in cancer prevention: a review of the evidence and mechanism of action. Proc Nutr Soc 64:527–542. https://doi.org/10.1079/pns2005467
Evans SO, Khairuddin PF, Jameson MB (2017) Optimising selenium for modulation of cancer treatments. Anticancer Res 37:6497–6509. https://doi.org/10.21873/anticanres.12106
Fairweather-Tait SJ, Bao Y, Broadley MR et al (2011) Selenium in human health and disease: an overview. Antioxid Redox Signal 14:3–26. https://doi.org/10.1007/978-3-319-95390-8_1
Vinceti M, Filippini T, Wise LA, Rothman KJ (2021) A systematic review and dose-response meta-analysis of exposure to environmental selenium and the risk of type 2 diabetes in nonexperimental studies. Environ Res 197:111210. https://doi.org/10.1016/j.envres.2021.111210
Urbano T, Filippini T, Lasagni D et al (2021) Associations between urinary and dietary selenium and blood metabolic parameters in a healthy northern italy population. Antioxidants 10:1–17. https://doi.org/10.3390/antiox10081193
Iqbal S, Ekmekcioglu C (2019) Maternal and neonatal outcomes related to iron supplementation or iron status: a summary of meta-analyses. J Matern Neonatal Med 32:1528–1540. https://doi.org/10.1080/14767058.2017.1406915
Cuenca-Micó O, Aceves C (2020) Micronutrients and breast cancer progression: a systematic review. Nutrients 12:1–18. https://doi.org/10.3390/nu12123613
Diallo A, Deschasaux M, Partula V, et al (2016) Dietary iron intake and breast cancer risk: modulation by an antioxidant supplementation. Oncotarget 7:79008–79016. https://doi.org/10.18632/oncotarget.12592
Collins JF, Knutson MD (2013) Metabolic crossroads of iron and copper. Nutr Rev 68:133–147. https://doi.org/10.1111/j.1753-4887.2010.00271.x.Metabolic
Blockhuys S, Wittung-Stafshede P (2017) Roles of copper-binding proteins in breast cancer. Int J Mol Sci 18:1–10. https://doi.org/10.3390/ijms18040871
Gaudet MM, Deubler EL, Kelly RS et al (2019) Blood levels of cadmium and lead in relation to breast cancer risk in three prospective cohorts. Int J Cancer 144:1010–1016. https://doi.org/10.1002/ijc.31805
Filippini T, Torres D, Lopes C et al (2020) Cadmium exposure and risk of breast cancer: a dose-response meta-analysis of cohort studies. Environ Int 142:105879. https://doi.org/10.1016/j.envint.2020.105879
Kabat GC, Cross AJ, Park Y et al (2010) Intakes of dietary iron and heme-iron and risk of postmenopausal breast cancer in the National Institutes of Health-AARP diet and health study. Am J Clin Nutr 92:1478–1483. https://doi.org/10.3945/ajcn.111.017947
Shamseer L, Moher D, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: Elaboration and explanation. BMJ 349:1–25. https://doi.org/10.1136/bmj.g7647
Fernandez-Lazaro CI, Martínez-González MÁ, Aguilera-Buenosvinos I et al (2021) Dietary antioxidant vitamins and minerals and breast cancer risk: prospective results from the sun cohort. Antioxidants 10:340. https://doi.org/10.3390/antiox10030340
Pantavos A, Ruiter R, Feskens EF et al (2015) Total dietary antioxidant capacity, individual antioxidant intake and breast cancer risk: the Rotterdam study. Int J Cancer 136:2178–2186. https://doi.org/10.1002/ijc.29249
Pan SY, Zhou J, Gibbons L et al (2011) Antioxidants and breast cancer risk- a population-based case-control study in Canada. BMC Cancer 11:372. https://doi.org/10.1186/1471-2407-11-372
Adzersen K, Jess P, Freivogel KW et al (2003) Raw and cooked vegetables, fruits, selected micronutrients, and breast cancer risk : a case-control study in Germany. Nutr Cancer 46:131–137. https://doi.org/10.1207/S15327914NC4602
Guo D, Hendryx M, Liang X et al (2020) Association between selenium intake and breast cancer risk: results from the Women’s Health Initiative. Breast Cancer Res Treat 183:217–226. https://doi.org/10.1007/s10549-020-05764-6
Bengtsson Y, Sandsveden M, Manjer J (2021) Risk of breast cancer in relation to dietary intake of selenium and serum selenium as a marker of dietary intake: a prospective cohort study within the Malmö diet and cancer study. Cancer Causes Control 32:815–826. https://doi.org/10.1007/s10552-021-01433-1
Suzana S, Cham BG, Ahmad Rohi G et al (2009) Relationship between selenium and breast cancer: a case-control study in the Klang Valley. Singapore Med J 50:265–269
Harris HR, Bergkvist L, Wolk A (2012) Selenium intake and breast cancer mortality in a cohort of Swedish women. Breast Cancer Res Treat 134:1269–1277. https://doi.org/10.1007/s10549-012-2139-9
Bengtsson Y, Sandsveden M, Borgquist S, Manjer J (2021) Serum zinc and dietary intake of zinc in relation to risk of different breast cancer subgroups and serum levels as a marker of intake: a prospective nested case-control study. Breast Cancer Res Treat 189:571–583. https://doi.org/10.1007/s10549-021-06318-0
Chang VC, Cotterchio M, Bondy SJ, Kotsopoulos J (2020) Iron intake, oxidative stress-related genes and breast cancer risk. Int J Cancer 147:1354–1373. https://doi.org/10.1002/ijc.32906
Kallianpur AR, Lee SA, Gao YT et al (2008) Dietary animal-derived iron and fat intake and breast cancer risk in the Shanghai breast cancer study. Breast Cancer Res Treat 107:123–132. https://doi.org/10.1007/s10549-007-9538-3
Ferrucci LM, Cross AJ, Graubard BI et al (2009) Intake of meat, meat mutagens, and iron and the risk of breast cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. Br J Cancer 101:178–184. https://doi.org/10.1038/sj.bjc.6605118
Moore AB, Shannon J, Chen C et al (2009) Dietary and stored iron as predictors of breast cancer risk: a nested case-control study in Shanghai. Int J Cancer 125:1110–1117. https://doi.org/10.1002/ijc.24404
Kabat GC, Miller AB, Jain M, Rohan TE (2007) Dietary iron and heme iron intake and risk of breast cancer: a prospective cohort study. Cancer Epidemiol Biomarkers Prev 16:1306–1308. https://doi.org/10.1158/1055-9965.EPI-07-0086
Lo JJ, Park Y-MM, Sinha R, Sandler DP (2020) Association between meat consumption and risk of breast cancer: findings from the Sister Study. Int J Cancer 146:2156–2165. https://doi.org/10.1002/ijc.32547.Association
Inoue-Choi M, Sinha R, Gierach GL, Ward MH (2016) Red and processed meat, nitrite, and heme iron intakes and postmenopausal breast cancer risk in the NIH-AARP diet and health study. Int J Cancer 138:1609–1618. https://doi.org/10.1002/ijc.29901.Red
Grioni S, Agnoli C, Krogh V et al (2019) Dietary cadmium and risk of breast cancer subtypes defined by hormone receptor status: a prospective cohort study. Int J Cancer 144:2153–2160. https://doi.org/10.1002/ijc.32039
Adams SV, Quraishi SM, Shafer MM et al (2014) Dietary cadmium exposure and risk of breast, endometrial, and ovarian cancer in the women’s health initiative. Environ Health Perspect 122:594–600. https://doi.org/10.1289/ehp.1307054
Adams SV, Newcomb PA, White E (2012) Dietary cadmium and risk of invasive postmenopausal breast cancer in the VITAL cohort. Cancer Causes Control 23:845–854. https://doi.org/10.1007/s10552-012-9953-6
Julin B, Wolk A, Bergkvist L et al (2012) Dietary cadmium exposure and risk of postmenopausal breast cancer: a population-based prospective cohort study. Cancer Res 72:1459–1466. https://doi.org/10.1158/0008-5472.CAN-11-0735
Itoh H, Iwasaki M, Sawada N et al (2014) Dietary cadmium intake and breast cancer risk in Japanese women: a case-control study. Int J Hyg Environ Health 217:70–77. https://doi.org/10.1016/j.ijheh.2013.03.010
Eriksen KT, Halkjær J, Sørensen M et al (2014) Dietary cadmium intake and risk of breast, endometrial and ovarian cancer in danish postmenopausal women: a prospective cohort study. PLoS ONE 9:12–13. https://doi.org/10.1371/journal.pone.0100815
Chang VC, Cotterchio M, Khoo E (2019) Iron intake, body iron status, and risk of breast cancer: a systematic review and meta-analysis. BMC Cancer 19:543. https://doi.org/10.1186/s12885-019-5642-0
Gozzelino R, Arosio P (2016) Iron homeostasis in health and disease. Int J Mol Sci 17:1–14. https://doi.org/10.3390/ijms17010130
Tappel A (2007) Heme of consumed red meat can act as a catalyst of oxidative damage and could initiate colon, breast and prostate cancers, heart disease and other diseases. Med Hypotheses 68:562–564. https://doi.org/10.1016/j.mehy.2006.08.025
Ekmekcioglu C, Wallner P, Kundi M et al (2018) Red meat, diseases, and healthy alternatives: a critical review. Crit Rev Food Sci Nutr 58:247–261. https://doi.org/10.1080/10408398.2016.1158148
American Institute for Cancer Research (2018) Recommendations and public health and policy implications. https://www.wcrf.org/wp-content/uploads/2021/01/Recommendations.pdf
Zhu X, Pan D, Wang N et al (2021) Relationship between selenium in human tissues and breast cancer: a meta-analysis based on case-control studies. Biol Trace Elem Res. https://doi.org/10.1007/s12011-021-02574-9
Benderli Cihan Y, Sözen S, Öztürk Yıldırım S (2011) Trace elements and heavy metals in hair of stage III breast cancer patients. Biol Trace Elem Res 144:360–379. https://doi.org/10.1007/s12011-011-9104-z
Lopez-Saez JB, Senra-Varela A, Pousa-Estevez L (2003) Selenium in breast cancer. Oncology 64:227–231. https://doi.org/10.1159/000069312
Wallenberg M, Misra S, Björnstedt M (2014) Selenium cytotoxicity in cancer. Basic Clin Pharmacol Toxicol 114:377–386. https://doi.org/10.1111/bcpt.12207
Zhang S, Li F, Younes M et al (2013) Reduced selenium-binding protein 1 in breast cancer correlates with poor survival and resistance to the anti-proliferative effects of selenium. PLoS ONE 8:1–11. https://doi.org/10.1371/journal.pone.0063702
Lee KH, Jeong D (2012) Bimodal actions of selenium essential for antioxidant and toxic pro-oxidant activities: the selenium paradox (Review). Mol Med Rep 5:299–304. https://doi.org/10.3892/mmr.2011.651
Maraldi T, Riccio M, Zambonin L et al (2011) Low levels of selenium compounds are selectively toxic for a human neuron cell line through ROS/RNS increase and apoptotic process activation. Neurotoxicology 32:180–187. https://doi.org/10.1016/j.neuro.2010.10.008
Stewart MS, Spallholz JE, Neldner KH, Pence BC (1999) Selenium compounds have disparate abilities to impose oxidative stress and induce apoptosis. Free Radic Biol Med 26:42–48. https://doi.org/10.1016/S0891-5849(98)00147-6
Skrajnowska D, Tokarz A, Makowska J, Bobrowska-Korczak B (2021) Changes in the mineral composition of rat tissues induced by breast cancer and dietary supplementation. In Vivo (Brooklyn) 35:259–266. https://doi.org/10.21873/INVIVO.12254
Gulbahçe-Mutlu E, Baltaci SB, Menevse E, et al (2021) The effect of zinc and melatonin administration on lipid peroxidation, IL-6 levels, and element metabolism in DMBA-induced breast cancer in rats. Biol Trace Elem Res 199:1044–1051. https://doi.org/10.33263/BRIAC111.75807588
Baltaci SB, Mogulkoc R, Baltaci AK et al (2017) The effect of zinc and melatonin supplementation on immunity parameters in breast cancer induced by DMBA in rats. Arch Physiol Biochem 124:247–252. https://doi.org/10.1080/13813455.2017.1392580
Bobrowska-Korczak B, Gatarek P, Skrajnowska D et al (2020) Effect of zinc supplementation on the serum metabolites profile at the early stage of breast cancer in rats. Nutrients 12:3457. https://doi.org/10.3390/nu12113457
Feng Y, Zeng JW, Ma Q et al (2020) Serum copper and zinc levels in breast cancer: a meta-analysis. J Trace Elem Med Biol 62:126629. https://doi.org/10.1016/j.jtemb.2020.126629
Wu X, Tang J, Xie M (2015) Serum and hair zinc levels in breast cancer: a meta-analysis. Sci Rep 5:1–8. https://doi.org/10.1038/srep12249
Tapiero H, Townsend DM, Tew KD (2003) Trace elements in human physiology and pathology. Copper Biomed Pharmacother 57:386–398. https://doi.org/10.1016/S0753-3322(03)00012-X
Antoniades V, Sioga A, Dietrich EM et al (2013) Is copper chelation an effective anti-angiogenic strategy for cancer treatment? Med Hypotheses 81:1159–1163. https://doi.org/10.1016/j.mehy.2013.09.035
Cavallo F, Gerber M, Marubini E et al (1991) Zinc and copper in breast cancer. A joint study in northern Italy and southern France. Cancer 67:738–745. https://doi.org/10.1002/1097-0142(19910201)67:3%3c738::aid-cncr2820670335%3e3.0.co;2-#
Wu X, Zhu X, Xie M (2015) Association between dietary cadmium exposure and breast cancer risk: an updated meta-analysis of observational studies. Med Sci Monit 21:769–775. https://doi.org/10.12659/MSM.892743
Peng L, Huang Y, Zhang J et al (2015) Cadmium exposure and the risk of breast cancer in Chaoshan population of southeast China. Environ Sci Pollut Res 22:19870–19878. https://doi.org/10.1007/s11356-015-5212-1
Rahim F, Jalali A, Tangestani R (2013) Breast cancer frequency and exposure to cadmium: a meta-analysis and systematic review. Asian Pacific J Cancer Prev 14:4283–4287. https://doi.org/10.7314/APJCP.2013.14.7.4283
Luevano J, Damodaran C (2014) A review of molecular events of cadmium-induced carcinogenesis. J Environ Pathol Toxicol Oncol 33:183–194. https://doi.org/10.1615/JEnvironPatholToxicolOncol.2014011075
Lin J, Zhang F, Lei Y (2016) Dietary intake and urinary level of cadmium and breast cancer risk: a meta-analysis. Cancer Epidemiol 42:101–107. https://doi.org/10.1016/j.canep.2016.04.002
Gammoh NZ, Rink L (2017) Zinc in infection and inflammation. Nutrients 9:624. https://doi.org/10.3390/nu9060624
Lonnerdal B (2000) Dietary factors influencing zinc absorption. J Nutr 130:1344S-1349S
Gunnar F. Nordberg, Bruce A, Fowler MN (2015) Cadmium. In: Handbook on the Toxicology of Metals, Fourth Edi. Academic press, Cambridge, Massachusetts, US, pp 667–716
Urbano T, Filippini T, Lasagni D, et al (2021) Association of urinary and dietary selenium and of serum selenium species with serum alanine aminotransferase in a healthy italian population. Antioxidants 10: https://doi.org/10.3390/antiox10101516
Vinceti M, Grill P, Malagoli C et al (2015) Selenium speciation in human serum and its implications for epidemiologic research: a cross-sectional study. J Trace Elem Med Biol 31:1–10. https://doi.org/10.1016/j.jtemb.2015.02.001
Acknowledgements
The authors acknowledge Dr. Cem Ekmekcioglu, Dr. Michael Poteser, and Dr. Hanns Moshammer for their support and suggestions to improve the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization, SI; literature search, SI and IA; data compilation, SI and IA; writing—original draft, SI; review and validity, SI and IA; and editing, IA.
Corresponding author
Ethics declarations
The authors do not reflect any views, opinions, or positions of any government, organization, employer, or institution.
Conflicts of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iqbal, S., Ali, I. Dietary Trace Element Intake and Risk of Breast Cancer: A Mini Review. Biol Trace Elem Res 200, 4936–4948 (2022). https://doi.org/10.1007/s12011-021-03089-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-03089-z