Abstract
Excessive exposure of iodine over a time is well known to cause thyroid dysfunction, which may be followed by different effects on body organs. The present study aimed to illustrate the impacts of exposure of rats to excess iodine (above the tolerable range) and the reversibility of any negative impacts on hormonal profile related to thyroid besides cortisol and the hematological and biochemical parameters along with the histopathological alterations in the thyroid gland, liver, kidneys, and heart. Seventy-five rats were divided equally into three groups: Group 1 was control animals. Groups 2 and 3 received sodium iodide (NaI) orally at a dose of (35 and 70 mg/kg BW), which corresponded to (500 and 1000) times excess iodine from the physiological dose, respectively for 30 days, then the NaI administration stopped in the treated groups for 15 consecutive days. Blood and tissue samples were collected twice for various experimental tests after 30 and 15 days of exposure to excess iodine and stopping the exposure, respectively. Overall results revealed that excess iodine in both tested groups developed a hyperthyroid condition, hypercortisolism, relative polycythemia, neutropenia, elevation in serum liver and cardiac enzymes activities, hyperprotenemia, hyperglobulinemia, elevation in serum urea, and cardiac troponin I concentrations (p < 0.05). It was concluded that the excess iodine caused hyperthyroidism, which was associated with significant changes in erythrogram and leukogram and alterations in hepatic, renal, and cardiac functions in an iodine dose-dependent damage relationship and the most of negative impacts continued after stopping the administration.








Similar content being viewed by others
References
Heyland A, Moroz LL (2005) Cross-kingdom hormonal signaling: an insight from thyroid hormone functions in marine larvae. J Exp Biol 208:4355–4361. https://doi.org/10.1242/jeb.01877
Patrick L (2008) Iodine: deficiency and therapeutic considerations. Altern Med Rev 13:116–127
Laurberg P, Pedersen IB, Knudsen N, Ovesen L, Andersen S (2001) Environmental iodine intake affects the type of non-malignant thyroid disease. Thyroid 11(5):457–469. https://doi.org/10.1089/105072501300176417
Delange F, Lecomte P (2000) Iodine supplementation: benefits outweigh risks. Drug Saf 22:89–95. https://doi.org/10.2165/00002018-200022020-00001
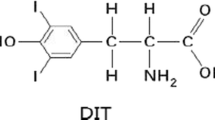
Liu D, Lin X, Yu F, Zhang M, Chen H, Bao W, Wang X (2015) Effects of 3,5-diiodotyrosine and potassium iodide on thyroid function and oxidative stress in iodine-excess Wistar rats. Biol Trace Elem Res 168(2):44752. https://doi.org/10.1007/s12011-015-0371-y
Luo Y, Kawashima A, Ishido Y, Yoshihara A, Oda K, Hiroi N, Ito T, Ishii N, Suzuki K (2014) Iodine excess as an environmental risk factor for autoimmune thyroid disease. Int J Mol Sci 15:12895–12912. https://doi.org/10.3390/ijms150712895
Georgitis WJ, McDermott MT, Kidd GS (1993) An iodine load from water-purification tablets alters thyroid function in humans. Mil Med 158:794–797. https://doi.org/10.1093/milmed/158.12.794
Zhao J, Chen Z, Maberly G (1998) Iodine-rich drinking water of natural origin in China. Lancet 352:2024. https://doi.org/10.1016/S0140-6736(05)61375-X
Franke K, Meyer U, Wagner H, Flachowsky G (2009) Influence of various iodine supplementation levels and two different iodine species on the iodine content of the milk of cows fed rapeseed meal or distillers dried grains with solubles as the protein source. J Dairy Sci 92:4514–4523. https://doi.org/10.3168/jds.2009-2027
Paulíková I, Kováč G, Bíreš J, Paulík Š, Seidel H, Nagy O (2002) Iodine toxicity in ruminants. Vet Med -Czech 47(12):343–350. https://doi.org/10.17221/5845-VETMED
William W (2008) Mineral tolerances of Animals. Tri-State Dairy Nutr Conf
Soetan K, Olaiya CO, Oyewole OE (2009) The importance of mineral elements for humans, domestic animals and plants: a review. Afr J Food Sci 4(5):200–222
Goa TS, Hu FN, Teng WP (2003) Effect of mild and moderate excessive iodine supplementation on thyroid function and morphology in non-iodine deficiency rat model. Zhonghua Nei Ke Za Zhi 42(10):705–708
Food Standards Australia New Zealand (FSANZ) (2008) Final assessment report-proposal P230: consideration of mandatory fortification with iodine for New Zealand. Food Standards Australia New Zealand, Wellington
Burgi H (2010) Iodine excess. Best Pract Res Clin Endocrinal 24:107–115. https://doi.org/10.1016/j.beem.2009.08.010
Rose HR, Zulfiqar H (2021) Jod Basedow syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing.
Shahid MA, Ashraf MA, Sharma S (2020) Physiology, thyroid hormone. In: StatPearls. Treasure Island (FL): StatPearls Publishing.
NRC (1995) Nutrient requirements of laboratory animals, 4th edn. National Academy Press, Washington DC
Lupachik SV, Nadol'nik LI, Netsetskaya ZV, Vinogradov VV (2006) Effects of chronic administration of high doses of potassium iodide on iodine metabolism in the rat thyroid gland. Biomed Khim 52(2):161–168
Clayton GD, Clayton FE (1981) In: Patty’s industrial toxicology and hygiene. Clayton GD and Clayton FE (eds.), 3rd edn. Vol 2B, p 2975
Chakraborty A, Mandal J, Mondal C, Sinha S, Chandra AK (2016) Effect of excess iodine on oxidative stress markers, steroidogenic-enzyme activities, testicular morphology, and functions in adult male rats. Biol Trace Elem Res 172(2):380–394. https://doi.org/10.1007/s12011-015-0581-3
Suvarna KS, Layton C, Bancroft JD (2013) Bancroft’s theory and practice of histological techniques, 7th edn. Churchill Livingstone Elsevier, China
Snedecor GW, Cochran WG (1994) Statistical method, 8th edn. Iowa State University Press, Ames
Norman AW, Litwack G (1996) Thyroid hormones. In: Norman AW, Litwack G (eds) Hormones, 2nd edn. Academic Press, pp 169–191. https://doi.org/10.1016/B978-012521441-4/50007-9
Sarkar D, Chakraborty A, Saha A, Chandra AK (2018) Iodine in excess in the alterations of carbohydrate and lipid metabolic pattern as well as histomorphometric changes in associated organs. J Basic Clin Physiol Pharmacol 29(6):631–643. https://doi.org/10.1515/jbcpp-2017-0204
Brent GA (2010) Thyroid function testing. Springer, NY. https://doi.org/10.1007/978-1-4419-1485-9
Fitzgerald SP, Bean NG (2018) Thyroid stimulating hormone (TSH) autoregulation reduces variation in the TSH response to thyroid hormones. Temperature 5(4):380–389. https://doi.org/10.1080/23328940.2018.1513110
Welsh KJ, Soldin SJ (2016) How reliable are free thyroid and total T3 hormone assays? Eur J Endocrinol 175(6):R255–R263. https://doi.org/10.1530/EJE-16-0193
Willis GC (2014) Endocrine and metabolic emergencies, an issue of emergency medicine clinics of North America. Volume 32, Number 2. Elsevier, Philadelphia. https://doi.org/10.1016/j.emc.2014.03.001
Fradkin JE, Wolff J (1983) Iodide induced thyrotoxicosis. Medicine 62:1. https://doi.org/10.1097/00005792-198301000-00001
Christiansen JJ, Djurhuus CB, Gravholt CH, Iversen P, Christiansen JS, Schmitz O, Weeke J, Jørgensen JOL, Møller N (2007) Effects of cortisol on carbohydrate, lipid and protein metabolism: studies of acute cortisol withdrawal in adrenocortical failure. J Clin Endocrinol Metab 92:3553–3559. https://doi.org/10.1210/jc.2007-0445
Samidurai M, Kang H, Ramasamy VS, Jo J (2018) Impact of electrical stimulation on cortisol secretion in rat adrenal gland. BioChip J 12(3):216–221. https://doi.org/10.1007/s13206-017-2303-8
Johnson EO, Kamilaris TC, Calogero AE, Gold PW, Chrousos GP (2005) Experimentally induced hyperthyroidism is associated with activation of the rat hypothalamic-pituitary-adrenal axis. Eur J Endocrinol 153(1):177–185. https://doi.org/10.1530/eje.1.01923
Yashchenko A, Lutsyk S (2018) The influence of hypo- and hyperthyroidism on morphogenesis and histophysiology of adrenal glands. J Embryol Stem Cell Res 2(1):000107. https://doi.org/10.23880/JES-16000107
Suckow MA, Stevens KA, Wilson RP (2012) The laboratory rabbit, guinea pig, hamster, and other rodents, 1st edn. Academic press, Elsevier, San Diego, USA
Kandir S, Keskin E (2016) Effects of hypothyroidism and hyperthyroidism on hematological parameters in rats. Ankara Üniv Vet Fak Derg 63:371–376. https://doi.org/10.1501/Vetfak_0000002755
Díaz-Soto G (2014) Thyroid disorders: focus on hyperthyroidism. Rijeka, Croatia
Braverman LE, Cooper DS (2013) Werner and ingbar’s the thyroid: a fundamental and clinical text, 10th edn. Lippincott Williams and Wilkins, Philadelphia. https://doi.org/10.5772/57001
Eakin DL, Peake RL, Weiss GB (1983) Effect of therapy on the neutropenia of hyperthyroidism. South Med J 76(3):335–337. https://doi.org/10.1097/00007611-198303000-00017
Burrow GN, Oppenheimer JH, Volpe R (1990) Thyroid function and disease. W.B. Saunders Company, Philadelphia
Malik R, Hodgson H (2002) The relationship between the thyroid gland and the liver. QJM-Int J Med 95(9):559–569. https://doi.org/10.1093/qjmed/95.9.559
Ajayi AF, Akhigbe RE (2012) Implication of altered thyroid state on liver function. Thyroid Res Pract 9:84–87. https://doi.org/10.4103/0973-0354.99649
Arika WM, Nyamai DW, Osano KO, Ngugi MP, Njagi ENM (2016) Biochemical markers of in vivo hepatotoxicity. J Clin Toxicol 6:297
Upadhyay G, Singh R, Kumar A, Kumar S, Kapoor A, Godbole M (2004) Severe hyperthyroidism induces mitochondria-mediated apoptosis in rat liver. Hepatology 39:1120–1130. https://doi.org/10.1002/hep.20085
Kumar A, Sinha RA, Tiwari M, Singh R, Koji T, Manhas N, Rastogi L, Pal L, Shrivastava A, Sahu RP, Godbole M (2007) Hyperthyroidism induces apoptosis in rat liver through activation of death receptor-mediated pathways. Mayo Clin 46(5):888–898. https://doi.org/10.1016/j.jhep.2006.12.015
Kim SM, Kim SC, Chung IK, Cheon WH, Ku SK (2012) Antioxidant and protective effects of bupleurum falcatum on the l-thyroxine-induced hyperthyroidism in rats. Evid Based Complement Alternat Med 2012:1–12. https://doi.org/10.1155/2012/578497
Suckow MA, Weisbroth SH, Franklin CL (2006) The laboratory rat, 2nd edn. Elsevier, Boston
Tothova C, Nagy O, Kovac G (2016) Serum proteins and their diagnostic utility in veterinary medicine: a review. Vet Med 61(9):475–496. https://doi.org/10.17221/19/2016-VETMED
Eckersall PD (2008) Proteins, proteomics, and the dysproteinemias. In: Kaneko JJ, Harvey JW, Bruss ML (eds) Clinical biochemistry of domestic animals, 6th edn. Elsevier Academic Press, California. https://doi.org/10.1016/B978-0-12-370491-7.00005-2
Wudeveld PGAB, Jansen AP (1960) Renal concentrating and water-excreting capacity in hyperthyroidism. Clinica Chimica Acta 5:618–621. https://doi.org/10.1016/0009-8981(60)90002-4
Mariotti S, Caturegli P, Barbesino G, Del Prete GF, Chiovato L, Pinchera A (1991) Circulating soluble interleukin 2 receptor concentration is increased in both immunogenic and nonimmunogenic hyperthyroidism. J Endocrinol Invest 14:777–781. https://doi.org/10.1007/BF03347915
Nandakumara DN, Konera BC, Vinayagamoorthia R, Nandaa N, Negib VS, Goswamia K, Bobbya Z, Hamide A (2008) Activation of NF-jB in lymphocytes and increase in serum immunoglobulin in hyperthyroidism: possible role of oxidative stress. Immunobiology 213:409–415. https://doi.org/10.1016/j.imbio.2007.10.005
Müller MJ, Seitz H (1984) Thyroid hormone action on intermediary metabolism. Part III. Protein metabolism in hyper-and hypothyroidism. Klin Wochenschr 62:97–102. https://doi.org/10.1007/BF01738699
Thrall MA, Weiser G, Allison RW, Campbell TW (2012) Veterinary hematology and clinical chemistry, 2nd edn. John Wiley & Sons, Iowa
Birchard SJ, Sherding RG (2006) Saunders manual of small animal practice, 3rd edn. Saunders, Elsevier, Missouri, USA
Basu G, Mohapatra A (2013) Interactions between thyroid disorders and kidney disease. Indian J Endocrinol Metab 16(2):204–213. https://doi.org/10.4103/2230-8210.93737
Turakulov Ya K (1975) Thyroid hormones: biosynthesis, physiological effects, and mechanisms of action, 1st edn. Springer, NY
Loeb JN (1978) Metabolic changes: vitamin metabolism, renal function, body water and electrolytes. In: Werner SC, Ingbar SH (eds) The thyroid. Harper and Row Publishers Inc., Hagerstown, pp 705–715
Burtis CA, Ashwood ER, Bruns DE (2012) Tietz textbook of clinical chemistry and molecular diagnostics, 5th edn. Saunders, Elsevier
Joanta AE, Filip A, Clichici S, Andrei S, Cluj-Napoca Romania CN (2006) Iodide excess exerts oxidative stress in some target tissues of the thyroid hormones. Acta Physiol Hung 293:347–359. https://doi.org/10.1556/APhysiol.93.2006.4.11
Osuna PM, Udovcic M, Sharma MD (2017) Hyperthyroidism and the heart. MDCVJ XIII(2):60–63. https://doi.org/10.14797/mdcj-13-2-60
Ilker S, Demet S, Anton P (2020) Iodine-induced hyperthyroidism: do you mind? SANAMED 15(2):215–217. https://doi.org/10.24125/sanamed.v15i2.458
Acknowledgements
The author would like to thank Prof. Dr. Al-Sayed Al-Attar, Professor of Pathology, Faculty of Veterinary Medicine, Zagazig University, Egypt, for his generous help in examining and reading of histopathological slides.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ismail, H.T.H. The Impact of Iodine Exposure in Excess on Hormonal Aspects and Hemato-Biochemical Profile in Rats. Biol Trace Elem Res 200, 706–719 (2022). https://doi.org/10.1007/s12011-021-02681-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-02681-7