Abstract
Background
In selected patients with a desire to maintain activity levels greater than those recommended after reverse total shoulder arthroplasty, hemiarthroplasty remains an option for treatment of cuff tear arthropathy (CTA). However, given the relatively small case series that have been reported to date, little is known regarding which patients will show functional improvement after this surgery.
Questions/purposes
We asked: What factors are associated with achieving the minimum clinically important difference in the simple shoulder test (SST) after hemiarthroplasty for cuff tear arthropathy?
Patients and Methods
Between 1991 and 2007, two surgeons at one academic center performed 48 shoulder hemiarthroplasties for CTA. No patients were known to have died before data collection, and of those not known to have died, 42 (88%) were available for followup at a mean of 48 months (range, 24–132 months). During that time, the general indications for this approach were glenohumeral arthritis with superior decentering of the humeral head. The majority of the patients with CTA were treated nonoperatively with patient-directed physical therapy and other modalities. A total of 42 patients (42 shoulders; 24 males and 18 females) with CTA were treated with hemiarthroplasty and followed for a mean of 48 months (range, 24–132 months). This is a retrospective study that made use of a longitudinally maintained database, which included physical examination of ROM, the SST, VAS, and standardized radiographs. At latest followup, 33 of 42 patients achieved a clinically important percentage of maximum possible improvement (%MPI) in SST score, defined as an improvement of 30% of the total possible improvement on the 12-point scale (with higher scores representing better results).
Results
Intraoperative findings of a rotator cuff tear limited to the supraspinatus and infraspinatus (odds ratio [OR], ∞; 95% CI, 2.01 to ∞; p = 0.020) and limited preoperative external rotation (15° [range, −40° to 45°] vs 35° [range, 20°–45°], OR, 0.71; 95% CI, 0.38–0.90; p < 0.001) were associated with achieving the defined minimum functional improvement (30% of MPI) on multivariate analysis. Preoperative active elevation (p = 0.679) and use of a CTA-specific implant (p = 0.707) were not significantly associated with achievement of 30% of MPI.
Conclusion
Patients with intact teres minor and subscapularis tendons and patients with lower preoperative external rotation had a better prognosis for achieving a clinically important percentage of MPI at short-term followup. Although some patients were followed for more than 10 years, the majority were followed for fewer than 5 years; future studies will need to determine whether these early functional results are maintained for longer periods.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reverse total shoulder arthroplasty (RTSA) has been shown to provide good results for pain control and functional outcome for cuff tear arthropathy (CTA), a condition characterized by glenohumeral arthritis in the context of rotator cuff insufficiency [5, 14, 19, 22]. Yet long-term studies have shown declining functional outcome scores with time, a high risk of complications, and a lower likelihood of satisfaction in young patients [2, 3, 13]. As an alternative, hemiarthroplasty can be considered for patients with painful CTA without instability and for whom conservative treatment has failed.
Published series of hemiarthroplasty for CTA have shown mixed results regarding functional outcome, with unpredictable forward elevation and moderate patient satisfaction rates [1, 4, 7, 10, 18, 20, 24, 25]. Preoperative forward elevation greater than 90° has been reported as a positive prognostic indicator [7]. Aside from this, little is known regarding how to predict which patients might achieve satisfactory results. Prior studies generally have used the limited goals criteria of Neer et al. [15] or postoperative outcome scores alone without preoperative data, rather than minimum clinically important improvement in a functional outcome score. The Simple Shoulder Test (SST) [11] is a patient-reported outcome score with shown responsiveness and construct validity for shoulder arthritis [17]. A clinically important percentage of maximum possible improvement (%MPI) has been defined as an improvement of 30% of the total possible improvement on the 12-point scale (with higher scores representing better results) [6, 12].
Therefore, we asked: What factors are associated with achieving a clinically important percentage of maximum possible improvement in the SST after hemiarthroplasty for CTA?
Patients and Methods
Between 1991 and 2007, two surgeons (MAW, CAR) at one academic center performed 48 consecutive shoulder hemiarthroplasties for CTA. No patients were known to have died before data collection, and of those not known to have died, 42 (88%) were available for followup at a mean of 48 months (range, 24–132 months). The risks and potential benefits of treatment were discussed interactively and in detail with each patient. All patients gave written and oral consent to treatment and for inclusion in an institutional database. Study approval was granted for this study by our institutional review board. This is a retrospective study that made use of a longitudinally maintained database. A complete consecutive series was analyzed to limit selection bias. Data collection was completed in 2011, and subsequent data analysis and drafting of the manuscript began in 2013.
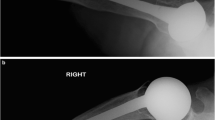
During the study period, the general indication for this approach was CTA (defined as superior translation on plain radiographs of the humeral head with respect to the glenoid, loss of articular surface of the humeral head, bone loss of the superior glenoid, and erosion of the greater tuberosity and undersurface of the acromion). This generally corresponds to Grades 3, 4, and 5 of the Hamada classification [9]. Exclusion criteria included glenohumeral arthritis with reparable cuff tears in shoulders without the radiographic findings noted above, instability of the shoulder with attempted forward elevation (anterosuperior escape), active infection, and inflammatory arthritis. The majority of patients with CTA treated during this time were managed nonoperatively with patient-directed physical therapy, antiinflammatory medications, moist heat, and activity modification; the number of patients treated without surgery was not recorded. Patients were selected for surgical treatment if they experienced severe limitations in quality of life owing to pain and loss of function after a trial of nonoperative management.
From this cohort, 42 of 48 patients (88%) were available for followup at a mean of 4 years (range, 2–11 years) (Fig. 1). All of these patients had preoperative SST scores, measurements for external rotation and active elevation, and postoperative SST scores at a minimum of 2 years. Preoperative radiographs were available for all but one patient. There were 24 males and 18 females. Their mean age at the time of surgery was 68 years (range, 46–84 years). Complete tearing of the supraspinatus and infraspinatus was present in 16 shoulders; three-tendon tears (complete tears of the supraspinatus and infraspinatus with partial tearing of the subscapularis or teres minor) were present in 24 shoulders; and four tendon tears (complete tears of the supraspinatus and infraspinatus with partial tearing of the subscapularis and teres minor) were present in two shoulders.
Twenty-one shoulders were treated with a conventional humeral head replacement (Global®; DePuy Orthopaedics, Warsaw, IN, USA) and 21 were treated with a CTA-specific head (Global® CTA head; DePuy Orthopaedics) during the time specified above. Prior procedures in the CTA group included 17 rotator cuff repairs in 16 patients, two distal clavicle excisions, one pectoralis major transfer, two rotator cuff débridements, and one subacromial decompression. The conventional hemiarthroplasty head tended to be used earlier in the series, while the CTA head was used more commonly after it became available between 2001 and 2007. All operations were performed by the senior authors (MAW, CAR).
Operative Technique
Surgical technique was performed as described previously [21]. A beach-chair position was used for all patients. A deltopectoral approach was used with careful attention to preservation of the deltoid. Degenerative, retracted rotator cuff tissue was débrided. The articular surface of the humeral head was resected in 20° to 30° retroversion. The humeral shaft was prepared and a conventional stem was placed in anatomic position. A head size equal to the resected head was selected, using either a CTA-specific prosthesis or a conventional prosthesis at the surgeon’s discretion. The glenoid was contoured with a burr or reamer if gross incongruency was noted. Additional capsular contractures were released in an effort to optimize motion and soft tissue balancing. The soft tissue balancing was thought to be ideal when the following criteria were achieved: (1) posterior drawer testing with 40% to 60% translation of the center of the prosthetic head relative to the center of the glenoid, (2) 60° internal rotation was present with the arm positioned in 90° abduction, (3) the hand on the involved side could be placed on the superior aspect of the contralateral shoulder without protraction of the scapula, and (4) there was 45° external rotation with the subscapularis approximated to the proximal humeral osteotomy site.
Postoperative Protocol
A physician-directed postoperative rehabilitation program, as described by Wirth et al. [23], was used for all patients regardless of subscapularis presence. On the afternoon of the day of surgery, the physician performed passive forward flexion of the arm up to 90°, or as far as was comfortable, for each patient. On the first postoperative day, the patient performed passive forward flexion with a pulley attached to an overhead frame, passive external rotation with a meter stick, and pendulum exercises. Each exercise involved five repetitions and was performed three to four times a day, seven days a week. The patients were encouraged to use the arm for gentle activities of daily living and they usually were discharged on the second postoperative day. Passive ROM exercises were continued until forward flexion of 120° to 140° had been obtained, at which point strengthening exercises were added.
Radiographic Analysis
Preoperative radiographs were evaluated with an axillary view and a true AP view perpendicular to the plane of the scapula with the humerus externally rotated 30°. The acromiohumeral interval was measured on true AP views as the shortest distance between the cortical undersurface of the acromion and the most proximal articular cortex of the humeral head [8]. Medial glenoid erosion and glenohumeral subluxation were measured according to the method of Rispoli et al. [16]. Glenoid erosion was classified as mild (subchondral plate erosion, depth < 5 mm), moderate (5–10 mm erosion), or severe (erosion medial to the lateral aspect of the coracoid base; typically > 10 mm). Anterior subluxation was classified as mild (< 25% translation of the humeral head relative to the center of the glenoid), moderate (25%–50% translation of the humeral head), or severe (> 50% translation). Finally, shoulders were classified as Type 1A (centered, stable), 1B (centered, medialized), IIA (decentered limited stable), or IIB (decentered unstable) according to the Seebauer method described by Visotsky et al. [21].
Outcome Variable
Patients were divided in two groups based on whether 30% of MPI in the SST score was reached. The clinically important change in the SST score was calculated using the method of Gilmer et al. [6], in which the clinically important difference is a percentage of possible improvement rather than a predefined numeric value. As in previous studies, the %MPI required for a clinically important difference was established at 30% of the difference between the preoperative SST score and the maximum achievable SST score [6, 12]. There were nine patients who achieved less than 30% of MPI as thus defined, and 33 patients who achieved or exceeded this.
Statistical Methods
Univariate analysis was performed to determine factors associated with achieving the defined 30% of MPI. Factors included demographics (age, sex, history of prior surgery), preoperative clinical (active external rotation, active elevation, SST score, VAS pain score) and radiographic (acromiohumeral interval, glenoid erosion, anterior subluxation, Seebauer classification) factors, surgery characteristics (year of surgery, implant type), and intraoperative assessment of rotator cuff tears.
Factors reaching a probability of 0.2 or lower on multivariate analysis were considered potentially important and included in subsequent multivariate analysis. A nominal logistic regression was performed with the binary response variable of whether 30% MPI had been achieved. The fit of the model was evaluated by calculating area under the receiver operating curve (AUC). Individual factors reaching below the threshold of a probability of 0.05 on multivariate analysis were considered significant.
Results
From our multivariate model, achieving 30% of maximum possible improvement in the SST was associated with decreased preoperative external rotation ((median, 15° [range, −40° to 45°] vs 35° [20°–45°]; odds ratio [OR], 0.71; 95% CI, 0.38–0.90; p < 0.001) and having only supraspinatus and infraspinatus tears (OR, ∞; 95% CI, 2.01 to ∞; p = 0.020), but preoperative SST score (p = 0.068) and preoperative VAS score (p = 0.611) were not associated with achieving 30% MPI (Table 1). Based on univariate analysis for achievement of 30% of maximum possible improvement, age, sex, year of surgery, implant type (CTA-specific versus conventional hemiarthroplasty), followup length, preoperative active elevation, history of previous surgery, and all radiographic parameters did not meet the defined level of significance for inclusion in multivariate analysis (Table 2). Therefore, only preoperative active elevation, preoperative SST score, preoperative VAS pain score and presence of only a two-tendon rotator cuff tear (supraspinatus and infraspinatus only) were included in multivariate nominal logistic regression. The model for multivariate analysis showed an AUC of 0.976, indicating an excellent fit.
Discussion
Shoulder hemiarthroplasty has been shown to improve functional outcomes in patients with CTA, but results are inconsistent. Factors that may predict a better or worse outcome are largely unknown. This study was performed to assess which prognostic factors would result in achievement of clinically important functional improvement in patients with CTA. Patients with more limited active external rotation and patients with rotator cuff deficiency limited to the supraspinatus and infraspinatus were the most likely to achieve 30% of the maximum possible improvement in SST score.
The inferences that may be drawn from the current study are subject to limitations. This study is small and, accordingly, susceptible to no-difference findings from insufficient power. Factors that were not identified as statistically significant may prove important in future, larger studies. Followup is short term and many patients have not been seen in several years, therefore the conclusions of this study are limited to a minimum of 2 years followup. These results may not hold up for patients followed for the longer term. The study does not include results for patients with CTA who were treated nonoperatively, which made up the majority of patients treated during the study period. These outcomes are generalizable only to patients for whom nonoperative treatment failed and who underwent surgery. Data analysis was not performed immediately after completing data collection; accordingly, the results do not represent the longest possible followup and they are generalizable only to the short term. The results are taken from a regional-based shoulder practice at an academic, high-volume institution, therefore, they may be applicable only to similar practice types and may not apply to lower-volume institutions or institutions that primarily treat patients with a lower level of complexity. Patients were not randomized to different treatment groups between the two implant types that were used through the study. As the study period progressed, patients were more likely to be treated with the CTA-specific hemiarthroplasty implant compared with the conventional hemiarthroplasty implant. This resulted in a shorter length of followup, as this prosthesis was introduced later, and represents an important potential source of bias. The finding that length of followup did not significantly correlate with achievement of 30% MPI reduces the likelihood that this affected our results.
Clinically important improvement in functional scores was more likely in patients with decreased preoperative active external rotation and rotator cuff tears limited to the supraspinatus and infraspinatus. One of the largest prior series of hemiarthroplasties in patients with CTA included 34 patients with a mean clinical followup of 3.7 years (range, 2–12 years) [7]. Potential prognostic factors including age, prior surgery, gender, preoperative forward elevation, and completeness of rotator cuff repair (“complete humeral head coverage”) were evaluated for correlation with postoperative outcome measures. Only preoperative forward elevation of 90° or greater was found to correlate with a higher mean postoperative American Shoulder and Elbow Surgeons score and a higher likelihood of achieving limited goals criteria. That study did not include preoperative self-assessed outcome measures, so it is not known whether a clinically important difference was achieved at latest followup. In contrast, we did not find greater preoperative forward elevation to be associated with improved likelihood of achieving a clinically important improvement in self-assessed outcome. It is possible that our exclusion of patients with frank instability and anterosuperior escape on attempted forward flexion was responsible for this difference. Urita et al. [20] reported on the results of surgical treatment of CTA with hemiarthroplasty and partial subscapularis transfer to the posterosuperior humeral head in 30 patients at 24 to 60 months followup. These patients achieved superior improvement in forward flexion (mean, 136°) compared with our study patients (mean, 113°) although the status of the rotator cuff was not reported. Long-term study is needed to determine whether these results remain durable with time. Comparisons between hemiarthroplasty and RTSA for patients with CTA have been reported in other studies [1, 10, 24]; generally superior results were obtained for RTSA although few prognostic factors were discussed. Young et al. [24] performed a case-matched registry study comparing 6-month results for hemiarthroplasty and RTSA. Although patients who underwent RTSA showed higher Oxford shoulder scores at 6 months, this difference was nonsignificant among patients 65 years old and younger. High-quality, large comparative studies between RTSA and hemiarthroplasty with adequate power for subgroup analyses are needed to determine which patient, surgeon, and procedural factors are important considerations.
In our small series, most patients experienced clinically important improvement in function after hemiarthroplasty at short term. Although a few of these patients were followed for more than 10 years, the majority were followed for fewer than 5 years; future studies will need to determine whether these early functional results are maintained during longer periods.
References
Coe MP, Greiwe RM, Joshi R, Snyder BM, Simpson L, Tosteson AN, Ahmad CS, Levine WN, Bell JE. The cost-effectiveness of reverse total shoulder arthroplasty compared with hemiarthroplasty for rotator cuff tear arthropathy. J Shoulder Elbow Surg. 2012;21:1278–1288.
Ek ET, Neukom L, Catanzaro S, Gerber C. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg. 2013;22:1199–1208.
Favard L, Levigne C, Nerot C, Gerber C, De Wilde L, Mole D. Reverse prostheses in arthropathies with cuff tear: are survivorship and function maintained over time? Clin Orthop Relat Res. 2011;469:2469–2475.
Field LD, Dines DM, Zabinski SJ, Warren RF. Hemiarthroplasty of the shoulder for rotator cuff arthropathy. J Shoulder Elbow Surg. 1997;6:18–23.
Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The Reverse Shoulder Prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency: a minuimum two-year follow-up study of 60 patients. J Bone Joint Surg Am. 2005;87:1697–1705.
Gilmer BB, Comstock BA, Jette JL, Warme WJ, Jackins SE, Matsen FA. The prognosis for improvement in comfort and function after the ream-and-run arthroplasty for glenohumeral arthritis: an analysis of 176 consecutive cases. J Bone Joint Surg Am. 2012;94:e102.
Goldberg SS, Bell JE, Kim HJ, Bak SF, Levine WN, Bigliani LU. Hemiarthroplasty for the rotator cuff-deficient shoulder. J Bone Joint Surg Am. 2008;90:554–559.
Gruber G, Bernhardt GA, Clar H, Zacherl M, Glehr M, Wurnig C. Measurement of the acromiohumeral interval on standardized anteroposterior radiographs: a prospective study of observer variability. J Shoulder Elbow Surg. 2010;19:10–13.
Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears: a long-term observation. Clin. Orthop Relat Res. 1990;254:92–96.
Leung B, Horodyski M, Struk AM, Wright TW. Functional outcome of hemiarthroplasty compared with reverse total shoulder arthroplasty in the treatment of rotator cuff tear arthropathy. J Shoulder Elbow Surg. 2012;21:319–323.
Lippitt SB, Harryman DT 2nd, Matsen FA 3rd, Fu FH, Hawkins RJ. A practical tool for evaluating function: the Simple Shoulder Test. In Matsen FA 3rd, Fu FH, Hawkins RJ, eds. The Shoulder: A Balance of Mobility and Stability. Rosemont, IL: American Academy of Orthopaedic Surgeons. 1993:501–518.
Matsen FA 3rd, Russ SM, Vu PT, Hsu JE, Lucas RM, Comstock BA. What factors are predictive of patient-reported outcomes? A prospective study of 337 shoulder arthroplasties. Clin Orthop Relat Res. 2016 July 25. [Epub ahead of print]
Muh SJ, Streit JJ, Wanner JP, Lenarz CJ, Shishani Y, Rowland DY, Riley C, Nowinski RJ, Edwards TB, Gobezie R. Early follow-up of reverse total shoulder arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2013;95:1877–1883.
Naveed MA, Kitson J, Bunker TD. The Delta III reverse shoulder replacement for cuff tear arthropathy: a single-centre study of 50 consecutive procedures. J Bone Joint Surg Br. 2011;93:57–61.
Neer CS 2nd, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am. 1983;65:1232–1244.
Rispoli DM, Sperling JW, Athwal GS, Schleck CD, Cofield RH. Humeral head replacement for the treatment of osteoarthritis. J Bone Joint Surg Am. 2006;88:2637–2644.
Roy JS, Macdermid JC, Faber KJ, Drosdowech DS, Athwal GS. The simple shoulder test is responsive in assessing change following shoulder arthroplasty. J Orthop Sports Phys Ther. 2010;40:413–421.
Sanchez-Sotelo J, Cofield RH, Rowland CM. Shoulder hemiarthroplasty for glenohumeral arthritis associated with severe rotator cuff deficiency. J Bone Joint Surg Am. 2001;83:1814–1822.
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff: results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388–395.
Urita A, Funakoshi T, Suenaga N, Oizumi N, Iwasaki N. A combination of subscapularis tendon transfer and small-head hemiarthroplasty for cuff tear arthropathy: a pilot study. Bone Joint J. 2015;97:1090–1095.
Visotsky JL, Basamania C, Seebauer L, Rockwood CA, Jensen KL. Cuff tear arthropathy: pathogenesis, classification, and algorithm for treatment. J Bone Joint Surg Am. 2004;86(suppl 2):35–40.
Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–1485.
Wirth MA, Tapscott RS, Southworth C, Rockwood CA Jr. Treatment of glenohumeral arthritis with a hemiarthroplasty: a minimum five-year follow-up outcome study. J Bone Joint Surg Am. 2006;88:964–973.
Young SW, Zhu M, Walker CG, Poon PC. Comparison of functional outcomes of reverse shoulder arthroplasty with those of hemiarthroplasty in the treatment of cuff-tear arthropathy: a matched-pair analysis. J Bone Joint Surg Am. 2013;95:910–915.
Zuckerman JD, Scott AJ, Gallagher MA. Hemiarthroplasty for cuff tear arthropathy. J Shoulder Elbow Surg. 2000;9:169–172.
Author information
Authors and Affiliations
Corresponding author
Additional information
One of the authors certifies that he (KB), or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from Depuy-Synthes (Warsaw, IN, USA).
One of the authors certifies that he (CAR), has or may receive payments or benefits, during the study period, an amount of more than USD 1,000,001 from Depuy-Synthes (Warsaw, IN, USA).
One of the authors certifies that he (MAW), has or may receive payments or benefits, during the study period, an amount of USD 100,001-1,000,000 from Depuy-Synthes (Warsaw, IN, USA) and less than USD 10,000 from Tornier (Lyon, France), Saunders (Philadelphia, PA, USA) and Arthrex (Naples, FL, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at UT Health Science Center at San Antonio, San Antonio, TX, USA.
About this article
Cite this article
Somerson, J.S., Sander, P., Bohsali, K. et al. What Factors are Associated With Clinically Important Improvement After Shoulder Hemiarthroplasty for Cuff Tear Arthropathy?. Clin Orthop Relat Res 474, 2682–2688 (2016). https://doi.org/10.1007/s11999-016-5037-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-016-5037-3