Abstract
Background
Prior studies of nonoperative treatment for lumbosacral radiculopathy have identified potential predictors of treatment failure, defined by persistent pain, persistent disability, lack of recovery, or subsequent surgery. However, few predictors have been replicated, with the exception of higher leg pain intensity, as a predictor of subsequent surgery.
Questions/purposes
We asked two research questions: (1) Does higher baseline leg pain intensity predict subsequent lumbar surgery? (2) Can other previously identified “candidate” predictors of nonoperative treatment failure be replicated?
Methods
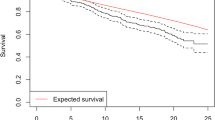
Between January 2008 and March 2009, 154 participants with acute lumbosacral radicular pain were enrolled in a prospective database; 128 participants (83%) received nonoperative treatment and 26 (17%) received surgery over 2-year followup. Ninety-four nonoperative participants (73%) responded to followup questionnaires. We examined associations between previously identified “candidate” predictors and treatment failure defined as (1) subsequent surgery; (2) persistent leg pain on a visual analog scale; (3) persistent disability on the Oswestry Disability Index; or (4) participant-reported lack of recovery over 2-year followup. Confounding variables including sociodemographics, clinical factors, and imaging characteristics were evaluated using an exploratory bivariate analysis followed by a multivariate analysis.
Results
With the numbers available, higher baseline leg pain intensity was not an independent predictor of subsequent surgery (adjusted odds ratio [aOR], 1.22 per point of baseline leg pain; 95% confidence interval [CI], 0.98–1.53; p = 0.08). Prior low back pain (aOR, 4.79; 95% CI, 1.01–22.7; p = 0.05) and a positive straight leg raise test (aOR, 4.38; 95% CI, 1.60–11.9; p = 0.004) predicted subsequent surgery. Workers compensation claims predicted persistent leg pain (aOR, 9.04; 95% CI, 1.01–81; p = 0.05) and disability (aOR, 5.99; 95% CI, 1.09–32.7; p = 0.04). Female sex predicted persistent disability (aOR, 3.16; 95% CI, 1.03–9.69; p = 0.05) and perceived lack of recovery (aOR, 2.44; 95% CI, 1.02–5.84; p = 0.05).
Conclusions
Higher baseline leg pain intensity was not confirmed as a predictor of subsequent surgery. However, the directionality of the association seen was consistent with prior reports, suggesting Type II error as a possible explanation; larger studies are needed to further examine this relationship. Clinicians should be aware of potential factors that may predict nonoperative treatment failure, including prior low back pain or a positive straight leg raise test as predictors of subsequent surgery, workers compensation claims as predictors of persistent leg pain and disability, and female sex as a predictor of persistent disability and lack of recovery.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.

Similar content being viewed by others
References
AAOS. Herniated Disk in the Lower Back (Outcomes). 2012. American Academy of Orthopaedic Surgeons. Available at: http://orthoinfo.aaos.org/topic.cfm?topic=a00534. Accessed April 19, 2004.
Atlas SJ, Chang Y, Kammann E, Keller RB, Deyo RA, Singer DE. Long-term disability and return to work among patients who have a herniated lumbar disc: the effect of disability compensation. J Bone Joint Surg Am. 2000;82:4–15.
Atlas SJ, Chang Y, Keller RB, Singer DE, Wu YA, Deyo RA. The impact of disability compensation on long-term treatment outcomes of patients with sciatica due to a lumbar disc herniation. Spine (Phila Pa 1976). 2006;31:3061–3069.
Atlas SJ, Tosteson TD, Blood EA, Skinner JS, Pransky GS, Weinstein JN. The impact of workers’ compensation on outcomes of surgical and nonoperative therapy for patients with a lumbar disc herniation: SPORT. Spine (Phila Pa 1976). 2010;35:89–97.
Breitenseher MJ, Eyb RP, Matzner MP, Trattnig S, Kainberger FM, Imhof H. MRI of unfused lumbar segments after spondylodesis. J Comput Assist Tomogr. 1996;20:583–587.
Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. 1997;72:95–97.
Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res. 2006;443:139–146.
Dionne CE, Dunn KM, Croft PR, Nachemson AL, Buchbinder R, Walker BF, Wyatt M, Cassidy JD, Rossignol M, Leboeuf-Yde C, Hartvigsen J, Leino-Arjas P, Latza U, Reis S, Gil Del Real MT, Kovacs FM, Oberg B, Cedraschi C, Bouter LM, Koes BW, Picavet HS, van Tulder MW, Burton K, Foster NE, Macfarlane GJ, Thomas E, Underwood M, Waddell G, Shekelle P, Volinn E, Von Korff M. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine (Phila Pa 1976). 2008;33:95–103.
Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25:2940–2952; discussion 2952.
Fardon DF. Nomenclature and classification of lumbar disc pathology. Spine (Phila Pa 1976). 2001;26:461–462.
Haugen AJ, Brox JI, Grovle L, Keller A, Natvig B, Soldal D, Grotle M. Prognostic factors for non-success in patients with sciatica and disc herniation. BMC Musculoskelet Disord. 2012;13:183.
Jensen TS, Albert HB, Sorensen JS, Manniche C, Leboeuf-Yde C. Magnetic resonance imaging findings as predictors of clinical outcome in patients with sciatica receiving active conservative treatment. J Manipulative Physiol Ther. 2007;30:98–108.
Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84.
Lequin MB, Verbaan D, Jacobs WC, Brand R, Bouma GJ, Vandertop WP, Peul WC. Surgery versus prolonged conservative treatment for sciatica: 5-year results of a randomised controlled trial. BMJ Open. 2013;3.
Luoto S, Hupli M, Alaranta H, Hurri H. Isokinetic performance capacity of trunk muscles. Part II: Coefficient of variation in isokinetic measurement in maximal effort and in submaximal effort. Scand J Rehabil Med. 1996;28:207–210.
Luoto S, Taimela S, Hurri H, Aalto H, Pyykko I, Alaranta H. Psychomotor speed and postural control in chronic low back pain patients: a controlled follow-up study. Spine. 1996;21:2621–2627.
Miranda H, Viikari-Juntura E, Martikainen R, Takala EP, Riihimaki H. Individual factors, occupational loading, and physical exercise as predictors of sciatic pain. Spine. 2002;27:1102–1109.
Ostelo RW, de Vet HC. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. 2005;19:593–607.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–1379.
Peul WC, Brand R, Thomeer RT, Koes BW. Improving prediction of ‘inevitable’ surgery during non-surgical treatment of sciatica. Pain. 2008;138:571–576.
Peul WC, Brand R, Thomeer RT, Koes BW. Influence of gender and other prognostic factors on outcome of sciatica. Pain. 2008;138:180–191.
Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, Thomeer RT, Koes BW. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356:2245–2256.
Rihn JA, Hilibrand AS, Radcliff K, Kurd M, Lurie J, Blood E, Albert TJ, Weinstein JN. Duration of symptoms resulting from lumbar disc herniation: effect on treatment outcomes: analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Joint Surg Am. 2011;93:1906–1914.
Rihn JA, Kurd M, Hilibrand AS, Lurie J, Zhao W, Albert T, Weinstein J. The influence of obesity on the outcome of treatment of lumbar disc herniation: analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Joint Surg Am. 2013;95:1–8.
Suri P, Hunter DJ, Jouve C, Hartigan C, Limke J, Pena E, Li L, Luz J, Rainville J. Nonsurgical treatment of lumbar disk herniation: are outcomes different in older adults? J Am Geriatr Soc. 2011;59:423–429.
Suri P, Rainville J, Katz JN, Jouve C, Hartigan C, Limke J, Pena E, Li L, Swaim B, Hunter DJ. The accuracy of the physical examination for the diagnosis of midlumbar and low lumbar nerve root impingement. Spine (Phila Pa 1976). 2011;36:63–73.
Tubach F, Beaute J, Leclerc A. Natural history and prognostic indicators of sciatica. J Clin Epidemiol. 2004;57:174–179.
Valls I, Saraux A, Goupille P, Khoreichi A, Baron D, Le Goff P. Factors predicting radical treatment after in-hospital conservative management of disk-related sciatica. Joint Bone Spine. 2001;68:50–58.
Verwoerd AJ, Luijsterburg PA, Lin CW, Jacobs WC, Koes BW, Verhagen AP. Systematic review of prognostic factors predicting outcome in non-surgically treated patients with sciatica. Eur J Pain. 2013;17:1126–1137.
Vroomen PC, de Krom MC, Knottnerus JA. When does the patient with a disc herniation undergo lumbosacral discectomy? J Neurol Neurosurg Psychiatry. 2000;68:75–79.
Vroomen PC, de Krom MC, Knottnerus JA. Predicting the outcome of sciatica at short-term follow-up. Br J Gen Pract. 2002;52:119–123.
Vroomen PC, de Krom MC, Wilmink JT, Kester AD, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry. 2002;72:630–634.
Vroomen PC, Wilmink JT, de KM. Prognostic value of MRI findings in sciatica. Neuroradiology. 2002;44:59–63.
Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976). 1983;8:131–140.
Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson AN, Herkowitz H, Fischgrund J, Cammisa FP, Albert T, Deyo RA. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296:2451–2459.
Acknowledgments
We thank the study participants for their time and effort.
Author information
Authors and Affiliations
Corresponding author
Additional information
VA Puget Sound provided support for one of the author’s (PS) participation in this research. A portion of this research was conducted while this author was funded by the Rehabilitation Medicine Scientist Training K12 Program (RMSTP) and the National Institutes of Health (K12 HD 01097).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
This research was approved by the New England Baptist Hospital Institutional Review Board. Each author certifies that the New England Baptist Hospital Institutional Review Board approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at New England Baptist Hospital, Boston, MA, USA.
About this article
Cite this article
Suri, P., Carlson, M.J. & Rainville, J. Nonoperative Treatment for Lumbosacral Radiculopathy: What Factors Predict Treatment Failure?. Clin Orthop Relat Res 473, 1931–1939 (2015). https://doi.org/10.1007/s11999-014-3677-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3677-8