Abstract
Purpose of the Review
Chronic tinnitus affects millions of people worldwide, but it remains an unmet clinical problem, particularly from a therapeutic perspective.
Recent Findings
Neuroimaging and neurophysiological investigations have consistently unveiled that tinnitus can be considered as a form of maladaptive plasticity taking place not only in primary and associative auditory areas but also involving large-scale brain networks. Based on these premises, treatment strategies that aim to manipulate in a controllable way plastic capabilities of the brain are being under investigation as emerging treatments.
Summary
here, we review the rationale for using so called Non-Invasive Brain stimulation (NiBS) techniques, such as navigated repetitive transcranial magnetic stimulation (rTMS) and other forms of transcranial electrical stimulation (tES) or peripheral stimulations, to alleviate tinnitus. We also provide an overview of available clinical results of these various non-invasive neuromodulatory approaches, trying to identify how to translate their unquestionable therapeutic potential into real-life contexts, beyond the lab boundaries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Definition, Classification, Epidemiology, Etiology, Pathophysiology
Today, tinnitus is still an unsolved scientific and clinical problem and an unmet clinical need from many perspectives: etiology, physiopathology and, most importantly, treatment. Probably the only true statement regarding tinnitus today is that it is not a single entity but a symptom resulting from a rather complex association and interplay of disorders of the inner ear, brain and psyche.
The term tinnitus is derived from the Latin verb tinnire (to ring), and it describes the subjective perception of an auditory sensation in the absence of a corresponding external sound [1]. In most cases the patient describes a subjective tinnitus (hissing, sizzling, and ringing) and only very rarely the tinnitus can be objectified (i.e., perceived also by the examiner). When this occurs, objective tinnitus can be heard by the examiner using a stethoscope or recorded with high sensitivity microphones. It can be caused by anomalies of vascular structures [2] or muscular spasm [3] in anatomical regions close to the ear.
The scientific definition of tinnitus is also controversial, and this is a major problem in studies. In a recent review, the most commonly used terminology was “tinnitus lasting for more than 5 min” [4]. The American Academy of Otolaryngology guidelines has defined tinnitus as “the perception of sound in the absence of an external source”. They also classified the symptom from different perspectives: i) etiology: primary (idiopathic, which may or may not be associated with sensorineural hearing loss) or secondary (associated with a specific underlying cause other than sensorineural hearing loss or to an identifiable organic condition); ii) duration: recent onset tinnitus (less than 6 months in duration, as reported by the patient), persistent tinnitus (6 months or longer in duration); iii) induced discomfort: bothersome tinnitus (distressed patient, impaired quality of life and/or functional health status; patient is seeking active therapy and management strategies to alleviate tinnitus), non-bothersome tinnitus (does not have a significant effect on a patient’s quality of life but may lead to curiosity of the cause or concern about the natural history and how it may progress or change) [5].
Tinnitus is a common symptom with an overall prevalence ranging from 5.1% to 42.7%. It is more common in adults and older people. Tinnitus can be mild (not noticeably interfering with daily life), moderate (causing some annoyance and described as unpleasant) or severe (disabling, significantly affecting daily life). The prevalence of disabling/bothersome tinnitus ranges from 3.0% to 30.9% [6].
Severe tinnitus is often associated with altered sound perception: sounds are distorted with reduced speech perception, reduced tolerance to sound (hyperacusis) and phonophobia. Recently, a straightforward classification of tinnitus has been proposed based on suspected etiology: type A (the treatable causes of tinnitus), type B (tinnitus with no medical explanation; idiopathic), and type C (tinnitus caused by diagnosable and treatable conditions, as listed in tinnitus type A, but the tinnitus persists after the successful treatment of the other symptoms) [7].
Little is known about the causes of tinnitus, if not that there are several well-known risk factors and disorders that can lead to tinnitus [8]. Among these, oto-neurological disorders must always be excluded: impacted wax, otitis media and external, paraganglioma, mastoiditis, labyrinthitis, sudden sensorineural hearing loss, Meniere’s disease, otosclerosis, presbyacusis, noise exposure, vestibular schwannoma, cerebellopontine angle tumors (meningioma), neurovascular compression syndrome, superior canal dehiscence syndrome, perylimphatic fistula, vestibular migraine, and use of ototoxic medications (aminoglycosides antibiotics, diuretics, chemotherapeutics). Many other, mostly but not exclusively neurological, factors that may play a role in tinnitus have been described: meningitis, multiple sclerosis, epilepsy, head injuries, temporomandibular joint disorders, hypertension, immunomediated disorders, diabetes, hypertension, hypotyroidism, anxiety and depression.
Although damage of the cochlea (inner and outer hair cells) has been considered a common cause of tinnitus for many years, the pathophysiology of tinnitus appears to be more complex [9]. It is known that even when the vestibulocochlear nerve is completely removed (for example after vestibular schwannoma surgery) the tinnitus often persists, mimicking a phantom sensation [10]. Although inner ear or auditory nerve conditions may often be the trigger to develop tinnitus, there is now strong evidence that tinnitus is a disorder of neural plasticity [9, 11]. As we will see more in detail later in the article, this pathophysiological concept has recently opened the possibility to manipulate these changes through neuromodulatory techniques aimed to restore more physiological firing patterns of cortical neurons’ activity. Reduced peripheral auditory neurons firing associated with transient (noise exposure) or permanent hearing loss could trigger a compensatory phenomenon that leads to increased activity of central auditory system neurons causing tinnitus. Also, neural synchrony may play an important role in tinnitus both in term of tonotopicity and neural temporal dynamics. Most of these scientific deductions come from animal model studies on noise induced hearing loss [12]. However, since tinnitus is a subjective symptom the validity of the animal model could be limited, although it has been demonstrated that in patients who underwent a cochlear implant and partly recovered hearing function, the tinnitus associated with the previous hearing loss was frequently reduced if not eliminated [13].
Diagnostic Evaluation
The diagnosis of tinnitus is primarily based on the identification of underlying risk factors/etiologies, triggers for symptom exacerbation and associated comorbidities [14]. The American Academy of Otolaryngology guidelines recommend that: Clinicians should (a) perform a focused history and physical examination at the initial evaluation of a patient with suspected primary tinnitus to identify conditions that, if promptly identified and treated, may relieve tinnitus; (b) obtain a prompt, comprehensive audiological evaluation in patients with tinnitus that is unilateral, persistent (≥ 6 months), or associated with hearing difficulties; (c) distinguish patients with bothersome tinnitus of recent onset from those with persistent symptoms (≥ 6 months) to prioritise intervention [5, 6].
Detailed anamnesis with particular attention to the onset, duration, laterality of tinnitus, audiological characteristics (pitch, intensity, pulsatility), triggers for exacerbation or modulation, associated hearing loss, hyperacusis, dizziness and vertigo, focal neurological symptoms and associated comorbidities is of paramount importance.
An otological microscopic evaluation is mandatory especially in the case of long lasting unilateral tinnitus, pulsatile tinnitus and when associated with hearing loss. Nevertheless, all tinnitus sufferers should undergo an otolaryngology consultation with audiological laboratory tests including pure tone audiometry, tympanometry and stapedial reflex testing. Imaging studies such as magnetic resonance imaging and computed tomography of the head are recommended only in patients with unilateral tinnitus, pulsatile tinnitus, associated asymmetric hearing loss, dizziness or vertigo and neurological abnormalities [15].
Psychological and psychiatric evaluation should be performed in patients with bothersome/disabling tinnitus or associated psychiatric disorders.
Tinnitus should be measured both in terms of its audiological characteristics and quality of life using questionnaires. Although audiological techniques to measure tinnitus (tinnitus sound matching, minimum masking level, loudness discomfort level) have not been validated from a diagnostic or prognostic perspective, they play an important role in patient follow-up [16]. Questionnaires are widely adopted to measure the disability associated with tinnitus and as an outcome of treatment. The Tinnitus Handicap Inventory is the most standardized and validated worldwide questionnaire of quality of life in subjects suffering from tinnitus [17].
Briefly, it consists of 25 questions aimed to identify, quantify, and evaluate the difficulties that a patient may be experiencing because of tinnitus. Answers may be “yes” (4 points), “sometimes” (2 points) or “no” (0 points). The resulting sum gives rise to a 5-degree of tinnitus subjective impact: Grade 1, slight or no handicap (0–17 points); grade 2, mild handicap (18–37 points); grade 3, moderate handicap (38–57 points); grade 4, severe handicap (58–77 points); grade 5, catastrophic handicap (78–100 points).
Current Treatments
Perhaps, the first attempt to treat tinnitus pharmacologically dates back to 1866, when Joseph Toynbee, an eminent otolarlyngologist at St Mary’s Hospital in London, was found dead on the couch in his consulting room. He had tried to alleviate his tinnitus by placing a cotton pad in his ear and face immersed into chloroform, but something went wrong [18].
The Treatment of tinnitus is still a controversial topic and although there are few otological and neuro-otological disorders that deserve their validated and definite treatment, it mainly relies on cognitive behavioural therapy and tinnitus retraining therapy [19].
Among the otological and neuro-otological disorders that cause tinnitus, otosclerosis, superior canal dehiscence syndrome, perilymphatic fistula, Meniere’s disease, vestibular schwannoma, sudden sensorineural hearing loss, chronic profound sensorineural hearing loss and presbycusis all of them have their specific and recommended treatments (either surgical or medical). However, all these treatments (steroids, stapedioplasty, cochlear implant, transtympanic gentamicin, hearing aids etc.) have the primary aim of improving hearing or vertigo/dizziness and their outcome on tinnitus is often unpredictable and generally unsatisfactory.
At the present time, the gold standard for the treatment of idiopathic chronic tinnitus is represented by cognitive behavioral therapy (CBT) [20]. A recent multidisciplinary systematic review concluded: “As the need for patient counselling is self-evident, specific tinnitus counselling should be provided. Due to the high level of evidence, validated tinnitus-specific, CBT is strongly recommended. In addition, auditory therapeutic measures can be recommended for the treatment of concomitant hearing loss and comorbidities; those should also be treated with drugs whenever appropriate. In particular, depression should be treated, with pharmacological support if necessary. If needed, psychiatric treatment should also be given on a case-by-case basis” [21].
Another commonly used therapeutic option is the Tinnitus Retraining Therapy (TRT), which is based on two main neurophysiological principles: (1) counseling, which is aimed to reclassify tinnitus to a category of a neutral signals and (2) sound therapy, which aims to attenuate tinnitus-related neuronal activity. A recent meta-analysis and systematic review of the literature on TRT concluded that “Analysis of limited studies low-quality evidence with a high risk of bias showed that the TRT was an effective treatment for tinnitus, which could improve the response rate of tinnitus and reduce the THI scale” [22].
Many other treatment options have been proposed for tinnitus: sound therapy (“masking”, [23]), acupuncture [24], ketamine (https://classic.clinicaltrials.gov/ct2/show/NCT03336398), ginko biloba [25], conservative temporomandibular disorder treatment [26], cervico-mandibular manual therapy [27], neurofeedback therapy [28], antidepressant and pain treatments [29], caffeine [30]. All of these treatments are, at the present time, not validated, and none of them have been shown to be superior to CBT in large meta-analysis/double blind, placebo-controlled trials or literature reviews and, therefore, cannot be recommended.
Neuroimaging and Neurophysiological Findings in Tinnitus
Neuroimaging and neurophysiological studies in tinnitus sufferers provide the background for using neuromodulation in an attempt to treat this symptom. However, a necessary premise is required: it should be kept in mind that either neuroimaging or neurophysiological studies only provide correlational evidence between a given finding (i.e., cortical reorganization, change in brain oscillations or tonotopy, etc.) and its behavioral counterpart (i.e., the tinnitus). Therefore, no direct causal conclusions can be drawn from the interpretation of these results. Nevertheless, they represent a necessary step to inform the targeting of neuromodulatory interventions (and sometimes follow up) that will be discussed in the next section.
Following the pioneering observation carried out via magnetoencephalography (MEG), that the auditory cortex contralateral to tinnitus shifts its tonotopic map representation [31], much evidence has accumulated that tinnitus, regardless of its initial cause and even when is idiopathic, could be a consequence of a dysfunctional plastic reorganization of local and distributed brain networks [9, 11, 12].
Early functional neuroimaging investigations of brain changes associated with tinnitus showed hyperactivation of discrete temporoparietal regions, including either the primary auditory cortex (AC) [32, 33] or the secondary, associative AC [32,33,34,35]. Causal evidence that the AC actively participates in tinnitus generation comes from studies in which brief trains of repetitive transcranial magnetic stimulation (rTMS) targeting the hyperactive left AC and interfering with local neural processing induced a transient suppression of the tinnitus itself [36,37,38].
There is general agreement that, by a phenomenological point of view, chronic tinnitus can be compared to the sensory deafferentation of phantom pain syndromes as a consequence of distorted sensory inputs at the cortical level [39]: however, in the case of chronic tinnitus, these maladaptive plasticity phenomena would take place at multiple brain levels, involving not only central auditory pathways, but also associated regions beyond the primary and associative AC [40]. Such a widespread cortical involvement, which may explain the wide range of symptoms associated with tinnitus (such as depression and anxiety, sleep disorders, emotional exhaustion and cognitive dysfunctions), has been highlighted in a recent review showing changes in many resting-state networks in tinnitus sufferers [41].
In these studies, the resting-state blood-oxygen-level dependent (BOLD) signal, which covaries with the neural activity, has been used to quantify regional brain function during magnetic resonance imaging (MRI) scans. In this way, resting-state (rs-fMRI) can be obtained, which quantifies the temporal dependence of neural activity patterns between brain regions that are anatomically segregated when the subject is not engaged in a task, so that the BOLD signal fluctuations can be used to infer functional connectivity between these regions [42]. In the case of tinnitus, not only the auditory network, but also the default mode network, as well as the visual, attentional and limbic networks, have been found to be involved. Due to the correlational nature of neuroimaging investigations, while these findings may partly explain the variety of symptoms complained by patients with tinnitus, it is still unclear whether these functional changes are primary or secondary to the tinnitus itself.
Neurophysiological studies in animal with behavioral models of tinnitus (usually triggered by prolonged exposure to noise) are not the topic of the present chapter, but certainly have helped to unveil three main types of neural changes accompanying tinnitus, that collectively point to a regional state of hyperexcitability in the auditory network: i) increases in the spontaneous activity of auditory neurons in subcortical and cortical structures; ii) increased burst firing in these structures; iii) increased synchronous activity among neurons affected by threshold shifts or suprathreshold hearing impairments [see 38 for detailed animal findings].
Similar patterns of neural hyperactivity at multiple levels of the central nervous system can be found in humans with tinnitus. Of interest is the hypothesis of the so called thalamo-cortical dysrhythmia, that postulates the tinnitus generation as a consequence of changes occurring in oscillatory brain activity (as revealed by MEG) when thalamic neurons enter a hyperpolarization state due to the (partial) deafferentation of auditory pathways [43]. Other MEG studies have reported increased delta and gamma oscillations in the auditory cortex of patients with chronic tinnitus, as well as reduction of alpha oscillatory activity [44,45,46,47]. While gamma oscillations reflects local communication within auditory regions, delta activity seems to be related to long-range functional connectivity between the AC and other non-auditory regions that contribute to tinnitus maintenance, as parietal, temporal, limbic and sensorimotor regions [48].
In summary, neuroimaging and neurophysiological findings converge on the notion that local hyperexcitability and hypermetabolism in the auditory network could be a hallmark of chronic tinnitus, but these abnormalities extend to other functionally connected cortical regions outside the primary and associative AC.
Non-Invasive Brain Stimulation (NIBS) Techniques and Rationale for Their Use in the Treatment of Tinnitus
NIBS encompasses techniques able to modify brain activity employing controlled, high-resolution transcranial delivery of electric field stimuli. Specifically, two main classes of NiBS are currently applied for rehabilitative/therapeutic applications in neurological and psychiatric disorders: repetitive transcranial magnetic stimulation (rTMS) and transcranial electrical stimulation (tES). In case of application of NiBS for tinnitus treatment, the rationale is to restore more physiological levels of altered local excitability in the auditory areas or in other functionally connected cortical regions outside the primary and associative AC. NiBS effects in this sense capitalize from their long-lasting after effects after the stimulation period which are sustained by different mechanisms according to the applied modality of stimulation, as explained in the following paragraphs.
Repetitive Transcranial Magnetic Stimulation (rTMS)
Transcranial Magnetic Stimulation (TMS) is based on Faraday's principle of electromagnetic induction: pulses of electrical current flow through loops of wire (forming the coil) and generate a time-varying magnetic field that in turn creates an electric field into the brain. The induced electric field alters ions' disposition and depolarizes neurons transynaptically [49] to the point of triggering an action potential. Different electric field strengths and forms can be generated by TMS through the modification of physical and biological parameters, such as magnetic pulse waveform, coil shape, orientation, intensity, frequency, and patterns of stimulation [50, 51].
When applied repetitively (rTMS) these train of pulses can change and modulate cortical activity well beyond the stimulation period. The physiological bases of rTMS after-effects are thought to rely on the induction of long-term potentiation (LTP) and long-term depression (LTD) mechanisms at synaptic level: LTP is defined as an increase in synaptic strength, whereas LTD reflects a decrease [52]. Accordingly, rTMS protocols affect the excitability and neuroplasticity of a stimulated area outlasting TMS duration per se, depending on inter-individual variability [53] as well as on the stimulation parameters, leading to a decreased cortical excitability when low-frequency rTMS (≤ 1 Hz) is applied, whereas an increase is seen following high-frequency rTMS (≥ 5 Hz) protocols [50]. Therefore, rTMS allows to control the level of inhibition and excitation of the stimulated regions in a predictable way. Daily sessions of stimulation may increase the duration of after effects, leading to a therapeutic effect.
More recent rTMS approaches involve the application of high-frequency bursts of stimuli at theta frequencies, known as theta-burst stimulation (TBS). Stimulus intensity required for TBS is lower compared to other rTMS protocols [54] and can be applied in a continuous (cTBS) or intermittent (iTBS) fashion depending on the purpose: cTBS tends to depress excitability of the primary motor cortex (where resulting excitability changes can be easily measured by looking at changes in the amplitude of motor evoked potentials), while iTBS has the opposite effect [54].
Because TMS has a spatial resolution of approximately 0.5–1 cm [55, 56], precise targeting of the area to stimulate is pivotal for the outcome. To finely target areas, navigated brain stimulation (NBS) has been developed. NBS devices consist of infrared camera detecting trackers placed on a headband worn by the subject and on the coil. Using Magnetic Resonance Imaging (MRI) brain data, NBS can rebuild the subject's head in 3-D and record coil position, ensuring better accuracy in targeting the chosen areas and as well as to have a finer estimation of the strength and direction of TMS-induced electrical field [57].
Transcranial Electrical Stimulation (tES)
tES uses low transcranial electrical currents (0.5–3 mA) that generate weak electric fields to target specific brain areas, allowing for the sub-threshold modulation of firing properties of cortical neurons and ongoing rhythmic brain activity. Various tES protocols can be implemented through different stimulation parameters, such as shape, position, number of electrodes, current waveform, frequency, and duration of stimulation. The electrical current is delivered through two or more surface electrodes placed on the scalp and connected to a current waveform generator. Transcranial direct current stimulation (tDCS), transcranial alternating current stimulation (tACS), and transcranial random noise stimulation (tRNS) are the most common protocols [58].
tDCS. tDCS induces a low-intensity direct current that modulates brain excitability eliciting neuronal membrane modifications depending on the direction of the generated electric field [59]. Current flows from the anodal electrode to the cathode, creating intracranial electric fields that alter cell membrane depolarization (i.e., increase of excitability) underneath the anode, and hyperpolarization (i.e., decrease of excitability) in the cathode, with lasting plastic effects that occur mainly after the stimulation rather than during it [60]: in particular, tDCS brings the underlying neurons closer or further from their firing threshold [61], leading to an increase in glutamine and glutamate levels and/or decreasing γ-aminobutyric acid (GABA) concentrations. N-methyl-D-aspartate (NMDA) receptor-dependent mechanisms as well as brain-derived neurotrophic factors (BDNF) [62] may also play a role to explain after effects. There is a non-linear relationship between dose of tDCS and after effects [63, 64] both for anodal and cathodal stimulations [65]; this relationship is currently assumed to reflect inter‐individual differences in anatomical (e.g. skull thickness, cortical morphology) and physiological (e.g. neurotransmitter availability and receptors distribution) factors, that similarly affect NIBS techniques both online [66] and after stimulation [67].
tACS uses alternating current that continuously shifts between positive and negative electric fields [58], thus inducing periodic shifts in the transmembrane potential, alternating depolarizing and hyperpolarizing effects, enabling the entrainment of intrinsic brain oscillations due to its sinusoidal waveform. In particular, tACS drives cortical populations to oscillate at the same natural frequency as the one delivered by the stimulation itself, with a greater amplitude as per the resonance phenomenon [58]. In this regard, tACS has been suggested as a very promising technique to safely and noninvasively modulate brain rhythms [68].
Most aspects of human brain functions and dysfunctions show corresponding patterns of brain oscillatory activity, determined by the synchronous neuronal firing across different spatial and temporal scales. Therefore, the chance to engage in oscillatory activity, rather than simply increase or decrease activity in a target region as with tDCS, could lead to a more powerful, finer control of brain activity and corresponding behavior. As with tDCS [69], tACS also allows stimulation over multiple brain regions at the same time, favouring network targeting rather than localized stimulations [70, 71].
The tRNS is another NiBS method that still uses alternating currents, but with random frequencies that can vary from low (0.1–100 Hz) to high-frequency (101–640 Hz) ranges [72] which resembles a “white noise” in its structure [58]. At a neural level, it is thought to induce repeated opening of sodium channels, with shortening of the hyperpolarization phase and causing an inward sodium current that results in a depolarization of the neural membrane [73]. Its potential application relays on the possibility to interfere with the tinnitus-related synchrony in the AC, thereby alleviating the tinnitus percept [74].
Overview of Nibs Clinical Results in Chronic Tinnitus
As the use of NiBS is growing up very rapidly, the International Federation of Clinical Neurophysiology has commissioned two expert groups for summarizing its evidence-based clinical utility in neurological and psychiatric disorders [75, 76]. In these reviews, the application of rTMS or tDCS in tinnitus did not reach an overall significant level of evidence in terms clinical efficacy, probably because the studies differed in terms of cortical targets, parameters of stimulation, number of sessions and follow up periods. This made impossible to pool them by a statistical point of view and, therefore, to obtain a meaningful evidence-based ranking.
However, more recent metanalyses have suggested some potential utility of NiBS in alleviating tinnitus, although with small/medium effects sizes and limited persistence in time [77,78,79]. We will briefly discuss the outcomes of these recent metanalyses.
Lefebvre-Demers and coworkers [78] performed a metanalysis (based on 28 rTMS studies and 9 tDCS studies after a careful selection for including or excluding them) and a modelling study by positing that NiBS methods (rTMS and tDCS) will modulate specific brain regions activity according with the neurobiological models of tinnitus. They compared outcomes of active stimulations with sham protocols, thus taking into account also placebo effects. Most of them were Randomized Controlled Trials (RCTs) with an average number of 33.8 ± 29.4 patients for rTMS and 28.1 ± 12.4 patients for tDCS. In the frame of considerable variability in terms of cortical targets, number and type of stimulations and follow up times, they conclude that while real rTMS was significantly superior to sham stimulation with a moderate effect size, active tDCS was not superior to sham stimulation.
More in detail, parameters of stimulation were generally inhibitory (rTMS at 1 Hz was applied in 20 studies and cTBS in 4), but in 3 studies excitatory rTMS was used. The number of neuromodulatory interventions ranged from 4 to 20 daily sessions and the follow up period ranged from 1 to 6 weeks. The cortical targets, all included in the networks of tinnitus generation and maintenance on the basis of previous neuroimaging investigations, were the primary AC (16, mostly on the left side), the temporo-parietal junction (8), but also both the associative AC (1), the dorsolateral prefrontal cortex (5, either left or right), the latter known to play a significant role in mood regulation: indeed, depression and anxiety may often accompany tinnitus discomfort.
Interestingly, the biophysical modelling suggested that the strongest electric field induced by rTMS applied over the AC was directed to the insula among all other region of interest (Amygdala, Anterior Cingulate Cortex, Cerebellum, Parahippocampus), thus supporting that beneficial effects on tinnuts were due impaired auditory information processing [80] rather than to impaired sensory and emotional processing that involve mainly the frontal regions and connections with the Amygdala [81, 82]. Despite some limitations due to the exclusion from the model of effects of network and dual stimulation sites, this seems and important information to inform more targeted future neuromodulatory treatments.
In the metanalysis [78], no significant effects were found for active tDCS versus sham, but few studies were considered (9), that used different cortical targets with bipolar montages, all included in tinnitus generation and maintenance based on previous neuroimaging investigations. The number of daily session ranged from 5 to 10 in two successive weeks, and the follow up ranged from two weeks to one month. Two studies of the same research group [83, 84] showed spectacular improvements of tinnitus scores (more than 20 points at THI), but all the remaining studies gave rise to very little or no clinical changes.
The most recently available review by Chen et al. [79] has included additional tDCS studies not considered by Lefebvre-Demers et al. [78] and also recent studies with tACS and tRNS that have become recently available. Regarding tDCS, they conclude that stimulation of AC and left temporoparietal area are basically not effective for tinnitus alleviation, differently from tDCS on the dorsolateral prefrontal cortex (DLPFC), for which 18 studies were reviewed: among studies investigating immediate effects of a single session of stimulation, therefore with no real-life clinical relevance but only pathophysiological relevance, a large study on 543 participants [85] showed a reduction of tinnitus severity and annoyance in 29.9% of patients who received anodal right/cathodal left tDCS, but not after inversion of the montage.
Traditional tDCS stimulations use large electrodes placed on the scalp, that result in non-focal distribution of induced electrical fields. Improvement of spatial resolution of tDCS is now possible thanks to High-Definition montages (HD-tDCS), in which the direct current is delivered through 4 × 1 electrode grid, with a maximal focus on the desired cortical target [86]. This approach has been shown promising results in 6 studies in terms of transient tinnitus alleviation in 31–77.8% of patients (see [79]), but only one or two session of HD-tDCS were run, so the clinical utility in the long term has still to be proven.
Currently, only three studies that used tACS in the upper theta/alpha bands (6–13 Hz) for 20 min in tinnitus are available, and all had negative outcomes regarding tinnitus alleviation, either when tACS was applied in a single session on AC or DLPFC [87, 88] or when multiple session on the AC were run [89]. However, considering pathological oscillations related to tinnitus generation and maintenance (see previous paragraph) and the potential of tACS to modify endogenous brain oscillations in a frequency specific manner [68] make tACS a suitable candidate for further clinical investigations aimed at alleviating tinnitus.
Finally, there are conflicting results regarding the effectiveness of tRNS for tinnitus alleviation: while Claes et al. [89] and Vanneste et al. [87] suggested that tRNS was superior to tDCS and tACS in this sense, particularly when multiple rather than single sessions of stimulation were run [90], two other studies showed negative outcomes [91, 92], at least when 100–640 Hz tRNS was applied. So, any conclusion on the utility of tRNS for tinnitus alleviation is currently precluded.
Non-Invasive Peripheral Stimulations for Treatment of Chronic Tinnitus
Brain neuromodulation can be achieved also by stimulation of peripheral afferents, rather than delivering currents from the scalp, either as a standalone therapy or temporally coupled with different kinds of acoustic stimulation in a bimodal way.
Vagus Nerve Stimulation (VNS)
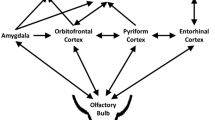
Among these techniques, VNS is an emerging treatment option for tinnitus. Although mechanisms of action of VNS have still to be fully elucidated, it is commonly accepted that VNS may target diverse and widespread brain regions through activation of diffuse afferent projections of the nucleus tractus solitarius [91] as well as promote the activation of noradrenergic and cholinergic modulatory afferent pathways in the forebrain, that play a central role in the modulation of cortical plasticity mechanisms [93, 94].
Here, we will consider only transcutaneous electrical stimulation of the sensory auricular branch of the vagus nerve, and not the application of stimulating wires along the nerve trunk, that requires an invasive surgical procedure.
A recent systematic review and metanalysis [95], that included five studies (3 of which were RCTs) for a total sample size of 234 tinnitus sufferers who received unilateral or bilateral transcutaneous VNS stimulation, has pointed out an overall small clinical effect. Said that heterogeneous modalities of stimulation (as frequency, wave pulse, electrode placement, interval time and total treatment time) were used across the five studies, the main findings were a significant effect on THI reduction post-treatment but not on Visual Analogue Scale (VAS) loudness of unilateral auricular stimulation versus controls and no significant differences between unilateral and bilateral stimulation at four weeks follow-up. The Authors [95] concluded their review and metanalysis hoping for future studies of better quality, with lower risk of bias.
Bimodal Stimulation
Another line of research is to combine electrical somatosensory stimulation with sound and/or wideband background noise. Such a bimodal neuromodulation, in which sound is coupled either with stimulation of trigeminal, vagal, tongue and other somatosensory afferents, can drive neural plasticity beneficial for tinnitus symptoms reduction [96,97,98,99] and is grounded on relevant animal evidences.
The largest one of these clinical trials is that of Conlon et al. [100], in which a device delivering electrical stimulation of the tongue via 32 electrodes and sound through wireless headphones was tested in 326 tinnitus sufferers. The study was exploratory and double-blind, no placebo controlled, with patients randomized into three parallel arms with different stimulation settings: in the first two arms there was a strict, although different between arms, temporal synchronization between electrical tongue stimulation and sounds; in the third arm, there was no synchronization and tones delivered through ears were lower. Wideband background noise was always present.
All patients in the three groups significantly improved at THI (and Tinnitus Functional Index) within the first six weeks of treatment rather than in the later six weeks, likely because of habituation to the modality of stimulation. Only the patients of the first two “synchronized bimodal” arms showed unprecedented positive and long-lasting (12 months) tinnitus alleviation, with a percentage of improved patients at the end of the intervention (at least 36 h of bimodal stimulation over 12 weeks, at least two daily 30-min sessions) ranging 75–89%. Despite the possible discomfort of having to hold the lingual stimulator with the mouth closed for one hour/day, the patients’ compliance was high.
The conceptual framework of the study by Conlon et al. [99] capitalized from the notion that bimodal stimulation might induce extensive short- and long-term “paired plasticty” in the auditory system, as well as in emotional and attentional centers, thereby improving tinnitus. This hypothesis is however challenged by the improvement of tinnitus even in the third group of patients, in which the bimodal stimulation was not temporally synchronized within useful time intervals (i.e., tens of milliseconds) for inducing paired plasticity.
In a second, again open (i.e., without placebo) study on 191 patients, Conlon and coworkers [100] verified a couple of important questions raised by results of the previous study. The first one relates to the real necessity of background wideband noise for the effectiveness of bimodal stimulation: indeed, this was present in all the arms of the previous study. The second one relates to the minimization of habituation to stimulation parameters, given that in the previous study the largest improvements were seen during the first six weeks of treatment. Results showed a significant reduction in tinnitus symptoms during the first 6-weeks in both treatment arms, without differences, which was further reduced in the following six weeks by resetting the parameters of stimulation. Therefore, bimodal pure tone/electrical tongue stimulation without wideband background seems sufficient for reducing symptoms and changing parameters of stimulation may provide better clinical outcomes. A placebo-controlled investigation showing superiority of the active treatment would complete the picture on the real clinical utility of the proposed bimodal stimulation.
Conclusions
NiBS interventions for the treatment of tinnitus have shown and continue to show promising clinical results, but their real-life utility in the long term remains to be determined. NiBS treatments are generally long (i.e., weeks), and require, on one hand, the allocation of relevant human resources to perform daily stimulation sessions, and, on the other hand are demanding for patients because they have to be performed in a hospital or clinic setting. rTMS seems to be more effective than tDCS or tACS/tRNS (although there are few data available here), but electrical stimulation has the advantage that it could be theoretically performed at home, thus reducing the burden on patients, who no longer have to travel to the hospital every day for treatment, and thus to increase the number of daily neuromodulatory sessions. Other forms of neuromodulation based on peripheral stimulations (transcutaneous VNS; bimodal tongue/sound stimulation) are emerging as possible treatments for tinnitus, but further studies are warranted to verify their actual long-term clinical impact in real-life conditions.
Data Availability
No datasets were generated on analysed during the current study.
References
Baguley D, McFerran D, Hall D. Tinnitus Lancet. 2013;382(9904):1600–7.
Verde P, Marciano E, De Falco R, Testa R, Buonamassa S, Mariniello G. Objective pulsatile tinnitus: case report. Acta Otorhinolaryngol Ital. 2003;23(5):383–7.
Tan SHL, Lee GJC. Prevalence and management outcomes of tonic tensor tympani syndrome in an ENT audiology tinnitus clinic in Singapore. J Laryngol Otol. 2024;138(6):627–33.
McCormack A, Edmondson-Jones M, Somerset S, Hall D. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res. 2016;337:70–9.
Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham ER Jr, Archer SM, Blakley BW, Carter JM, Granieri EC, Henry JA, Hollingsworth D, Khan FA, Mitchell S, Monfared A, Newman CW, Omole FS, Phillips CD, Robinson SK, Taw MB, Tyler RS, Waguespack R, Whamond EJ. Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg. 2014;151(2 Suppl):S1–40.
Tunkel DE, Jones SL, Rosenfeld RM. Guidelines for Tinnitus. JAMA. 2016;316:1214–5.
Lee KJ, Liu K. Tinnitus: A Stepchild in Our Specialty. Otolaryngol Head Neck Surg. 2018;159:599–600.
Biswas R, Genitsaridi E, Trpchevska N, Lugo A, Schlee W, Cederroth CR, Gallus S, Hall DA. Low Evidence for Tinnitus Risk Factors: A Systematic Review and Meta-analysis. J Assoc Res Otolaryngol. 2023;24:81–94.
Møller AR. The role of neural plasticity in tinnitus. Prog Brain Res. 2007;166:37-45. An important article addressing the role of maladaptive neural plasticity for tinnitus generation and mantainance.
House JW, Brackmann DE. Tinnitus: surgical treatment. Ciba Found Symp. 1981;85:204–16.
Roberts LE. Neural plasticity and its initiating conditions in tinnitus. HNO. 2018;66:172–8.
Eggermont J, Roberts L. The neuroscience of tinnitus. Trends Neurosci. 2004;27:676–82.
Blasco MA, Redleaf MI. Cochlear implantation in unilateral sudden deafness improves tinnitus and speech comprehension: meta-analysis and systematic review. Otol Neurotol. 2014;35:1426–32.
Dalrymple SN, Lewis SH, Philman S. Tinnitus: Diagnosis and Management. Am Fam Physician. 2021;103:663–71.
Adams ME, Huang TC, Nagarajan S, Cheung SW. Tinnitus Neuroimaging. Otolaryngol Clin North Am. 2020;53:583–603.
Henry JA. Otol Neurotol Measurement of Tinnitus. 2016;37:e276-85.
Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1996;122:143-148. The original paper that introduced the Tinnitus Handicap Inventory, still the most used scale for measuring tinnitus.
Simpson JF. Joseph Toynbee His contribution to Otology. Proc Royal Society Med. 1963;56:1–9.
Langguth B, Kreuzer PM, Kleinjung T, De Ridder D. Tinnitus: causes and clinical management. Lancet Neurol. 2013;12:920–30.
Czornik M, Malekshahi A, Mahmoud W, Wolpert S, Birbaumer N. Psychophysiological treatment of chronic tinnitus: A review. Clin Psychol Psychother. 2022;29:1236–53.
Zenner HP, Delb W, Kröner-Herwig B, Jäger B, Peroz I, Hesse G, Mazurek B, Goebel G, Gerloff C, Trollmann R, Biesinger E, Seidler H, Langguth B. A multidisciplinary systematic review of the treatment for chronic idiopathic tinnitus. Eur Arch Otorhinolaryngol. 2017;274:2079–91.
Han M, Yang X, Lv J. Efficacy of tinnitus retraining therapy in the treatment of tinnitus: A meta-analysis and systematic review. Am J Otolaryngol. 2021;42: 103151.
Sereda M, Xia J, El Refaie A, Hall DA, Hoare DJ. Sound therapy using amplification devices and or sound generators for tinnitus. Cochrane Database Syst Rev. 2018;12:CD013094.
Liu F, Han X, Li Y, Yu S. Acupuncture in the treatment of tinnitus: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2016;273:285–94.
Mahmoudian-Sani MR, Hashemzadeh-Chaleshtori M, Asadi-Samani M, Yang Q. Ginkgo biloba in the treatment of tinnitus: An updated literature review. Int Tinnitus J. 2017;21:58–62.
Michiels S, van der Wal AC, Nieste E, Van de Heyning P, Braem M, Visscher C, Topsakal V, Gilles A, Jacquemin L, Hesters M, De Hertogh W. Conservative therapy for the treatment of patients with somatic tinnitus attributed to temporomandibular dysfunction: study protocol of a randomised controlled trial. Trials. 2018;19:554.
Delgado de la Serna P, Plaza-Manzano G, Cleland J, Fernández-de-Las-Peñas C, Martín-Casas P, Díaz-Arribas MJ. Effects of Cervico-Mandibular Manual Therapy in Patients with Temporomandibular Pain Disorders and Associated Somatic Tinnitus A Randomized Clinical Trial. Pain Med. 2020;21:613–24.
Kleinjung T, Meyer M, Neff P. Neurofeedback for tinnitus treatment an innovative method with promising potential. Brain Commun. 2023;5:fcad209.
Beebe Palumbo D, Joos K, De Ridder D, Vanneste S. The Management and Outcomes of Pharmacological Treatments for Tinnitus. Curr Neuropharmacol. 2015;13:692–700.
Ledesma ALL, Leite Rodrigues D, Monteiro de Castro Silva I, Oliveira CA, Bahmad F Jr. The effect of caffeine on tinnitus: Randomized triple-blind placebo-controlled clinical trial. PLoS One. 2021;16:e0256275.
Muhlnickel W, Elbert T, Taub E, Flor H. Reorganization of auditory cortex in tinnitus. Proc Natl Acad Sci U S A. 1998;95:10340–3.
Andersson G, Lyttkens L, Hirvelä C, Furmark T, Tillfors M, Fredrikson M. Regional cerebral blood flow during tinnitus: a PET case study with lidocaine and auditory stimulation. Acta Otolaryngol. 2000;120:967–72.
Mirz F, Gjedde A, Ishizu K, Pedersen C. Cortical networks subserving the perception of tinnitus a PET study. Acta Otolaryngol Suppl. 2000;120:241e3.
Giraud AL, Chéry-Croze S, Fischer G, Fischer C, Vighetto A, Grégoire MC, Lavenne F, Collet L. A selective imaging of tinnitus. NeuroReport. 1999;10:1–5.
Plewnia C, Reimold M, Najib A, Brehm B, Reischl G, Plontke SK, Gerloff C. Dose-dependent attenuation of auditory phantom perception (tinnitus) by PET-guided repetitive transcranial magnetic stimulation. Hum Brain Mapp. 2007;28:238–46.
Plewnia C, Bartels M, Gerloff C. Transient suppression of tinnitus by transcranial magnetic stimulation. Ann Neurol. 2003;53:263–6. The first study addressing causality of the auditory cortex in tinnitus generation.
De Ridder D, De Mulder G, Walsh V, Muggleton N, Sunaert S, Møller A. Magnetic and electrical stimulation of the auditory cortex for intractable tinnitus. Case report J Neurosurg. 2004;100:560–4. The first report showing the possibility to alleviate tinnitus with noninvasive brain stimulation.
Fregni F, Marcondes R, Boggio PS, Marcolin MA, Rigonatti SP, Sanchez TG, Nitsche MA, Pascual-Leone A. Transient tinnitus suppression induced by repetitive transcranial magnetic stimulation and transcranial direct current stimulation. Eur J Neurol. 2006;13:996–1001.
Møller AR. Tinnitus and pain. Prog Brain Res. 2007;166:47–53.
Shore SE, Roberts LE, Langguth B. Maladaptive plasticity in tinnitus Triggers mechanisms and treatment. Nat Rev Neurol. 2016;12(3):150–60.
Kok TE, Domingo D, Hassan J, Vuong A, Hordacre B, Clark C, Katrakazas P, Shekhawat GS. Resting-state Networks in Tinnitus: A Scoping Review. Clin Neuroradiol. 2022;32:903–22.
Van den Heuvel MP, Pol HHE. Exploring the brain network: a review on resting-state fMRI functional connectivity. Eur Neuropsychopharmacol. 2010;20:519–34.
Llinás RR, Ribary U, Jeanmonod D, Kronberg E, Mitra PP. Thalamocortical dysrhythmia A neurological and neuropsychiatric syndrome characterized by magnetoencephalography. Proc Natl Acad Sci. 1999;96:15222–7.
Adjamian P, Sereda M, Zobay O, Hall DA, Palmer AR. Neuromagnetic indicators of tinnitus and tinnitus masking in patients with and without hearing loss. J Assoc Res Otolaryngol. 2012;13:715–31.
Wienbruch C, Paul I, Weisz N, Elbert T, Roberts LE. Frequency organization of the 40-Hz auditory steady-state response in normal hearing and in tinnitus. Neuroimage. 2006;33:180–94.
Weisz N, Moratti S, Meinzer M, Dohrmann K, Elbert T. Tinnitus perception and distress is related to abnormal spontaneous brain activity as measured by magnetoencephalography. PLoS Med. 2005;2: e153.
Weisz N, Müller S, Schlee W, Dohrmann K, Hartmann T, Elbert T. The neural code of auditory phantom perception. J Neurosci. 2007;27:1479–84.
Sedley W, Gander PE, Kumar S, Oya H, Kovach CK, Nourski KV, Kawasaki H, Howard MA 3rd, Griffiths TD. Intracranial Mapping of a Cortical Tinnitus System using Residual Inhibition. Curr Biol. 2015;25:1208–14.
Caliandro P, Padua L, Rossi A, Rossini PM, Stalberg E, Feurra M, Ulivelli M, Bartalini S, Giannini F, Rossi S. Jitter of corticospinal neurons during repetitive transcranial magnetic stimulation. Method and possible clinical implications. Brain Stimul. 2014;7:580–6.
Rossi S, Hallett M, Rossini PM, Pascual-Leone A Safety of TMS Consensus Group. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120:2008–39.
Rossi S, Antal A, Bestmann S, Bikson M, Brewer C, Brockmöller J, Carpenter LL, Cincotta M, Chen R, Daskalakis JD, Di Lazzaro V, Fox MD, George MS, Gilbert D, Kimiskidis VK, Koch G, Ilmoniemi RJ, Lefaucheur JP, Leocani L, Lisanby SH, Miniussi C, Padberg F, Pascual-Leone A, Paulus W, Peterchev AV, Quartarone A, Rotenberg A, Rothwell J, Rossini PM, Santarnecchi E, Shafi MM, Siebner HR, Ugawa Y, Wassermann EM, Zangen A, Ziemann U, Hallett M. basis of this article began with a Consensus Statement from the IFCN Workshop on “Present, Future of TMS: Safety, Ethical Guidelines”, Siena, October 17–20, 2018, updating through, April 2020 Safety and recommendations for TMS use in healthy subjects and patient populations, with updates on training, ethical and regulatory issues: Expert Guidelines. Clin Neurophysiol. 2021;132:269–306.
Klomjai W, Katz R, Lackmy-Vallée A. Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS). Ann Phys Rehabil Med. 2015;58:208–13.
Maeda F, Keenan JP, Tormos JM, Topka H, Pascual-Leone A. Interindividual variability of the modulatory effects of repetitive transcranial magnetic stimulation on cortical excitability. Exp Brain Res. 2000;133:425–30.
Huang YZ, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron. 2005;45:201–6.
Thielscher A, Kammer T. Linking physics with physiology in TMS: a sphere field model to determine the cortical stimulation site in TMS. Neuroimage. 2002;17:1117–30.
Toschi N, Welt T, Guerrisi M, Keck ME. A reconstruction of the conductive phenomena elicited by transcranial magnetic stimulation in heterogeneous brain tissue. Phys Med. 2008;24:80–6.
Cincotta M, Giovannelli F, Borgheresi A, Balestrieri F, Toscani L, Zaccara G, Carducci F, Viggiano MP, Rossi S. Optically tracked neuronavigation increases the stability of hand-held focal coil positioning: evidence from “transcranial” magnetic stimulation-induced electrical field measurements. Brain Stimul. 2010;3:119–23.
Paulus W. Transcranial electrical stimulation (tES - tDCS; tRNS, tACS) methods. Neuropsychol Rehabil. 2011;21:602–17.
Ruffini G, Wendling F, Merlet I, Molaee-Ardekani B, Mekonnen A, Salvador R, Soria-Frisch A, Grau C, Dunne S, Miranda PC. Transcranial current brain stimulation (tCS): models and technologies. IEEE Trans Neural Syst Rehabil Eng. 2013;21:333–45.
Santarnecchi E, Feurra M, Barneschi F, Acampa M, Bianco G, Cioncoloni D, Rossi A, Rossi S. Time Course of Corticospinal Excitability and Autonomic Function Interplay during and Following Monopolar tDCS. Front Psychiatry. 2014;5:86.
Bikson M, Inoue M, Akiyama H, Deans JK, Fox JE, Miyakawa H, Jefferys JG. Effects of uniform extracellular DC electric fields on excitability in rat hippocampal slices in vitro. J Physiol. 2004;557(Pt 1):175–90.
Fritsch B, Reis J, Martinowich K, Schambra HM, Ji Y, Cohen LG, Lu B. Direct current stimulation promotes BDNF-dependent synaptic plasticity: potential implications for motor learning. Neuron. 2010;66:198–204.
Batsikadze G, Moliadze V, Paulus W, Kuo MF, Nitsche MA. Partially non-linear stimulation intensity-dependent effects of direct current stimulation on motor cortex excitability in humans. J Physiol. 2013;591:1987–2000.
Monte-Silva K, Kuo MF, Hessenthaler S, Fresnoza S, Liebetanz D, Paulus W, Nitsche MA. Induction of late LTP-like plasticity in the human motor cortex by repeated non-invasive brain stimulation. Brain Stimul. 2013;6:424–32.
Jamil A, Batsikadze G, Kuo HI, Labruna L, Hasan A, Paulus W, Nitsche MA. Systematic evaluation of the impact of stimulation intensity on neuroplastic after-effects induced by transcranial direct current stimulation. J Physiol. 2017;595:1273–88.
Labruna L, Jamil A, Fresnoza S, Batsikadze G, Kuo MF, Vanderschelden B, Ivry RB, Nitsche MA. Efficacy of Anodal Transcranial Direct Current Stimulation is Related to Sensitivity to Transcranial Magnetic Stimulation. Brain Stimul. 2016;9:8–15.
Ridding MC, Ziemann U. Determinants of the induction of cortical plasticity by non-invasive brain stimulation in healthy subjects. J Physiol. 2010;588(Pt 13):2291–304.
Rossi S, Santarnecchi E, Feurra M. Noninvasive brain stimulation and brain oscillations. Handb Clin Neurol. 2022;184:239–47.
Mencarelli L, Menardi A, Neri F, Monti L, Ruffini G, Salvador R, Pascual-Leone A, Momi D, Sprugnoli G, Rossi A, Rossi S, Santarnecchi E. Impact of network-targeted multichannel transcranial direct current stimulation on intrinsic and network-to-network functional connectivity. J Neurosci Res. 2020;98:1843–56.
Ali MM, Sellers KK, Fröhlich F. Transcranial alternating current stimulation modulates large-scale cortical network activity by network resonance. J Neurosci. 2013;33:11262–75.
Ruffini G, Fox MD, Ripolles O, Miranda PC, Pascual-Leone A. Optimization of multifocal transcranial current stimulation for weighted cortical pattern targeting from realistic modeling of electric fields. Neuroimage. 2014;89:216–25.
Terney D, Chaieb L, Moliadze V, Antal A, Paulus W. Increasing human brain excitability by transcranial high-frequency random noise stimulation. J Neurosci. 2008;28:14147–55.
Schoen I, Fromherz P. Extracellular stimulation of mammalian neurons through repetitive activation of Na+ channels by weak capacitive currents on a silicon chip. J Neurophysiol. 2008;100:346–57.
van Doren J, Langguth B, Schecklmann M. Electroencephalographic effects of transcranial random noise stimulation in the auditory cortex. Brain Stimul. 2014;7:807–12.
Lefaucheur JP, Antal A, Ayache SS, Benninger DH, Brunelin J, Cogiamanian F, Cotelli M, De Ridder D, Ferrucci R, Langguth B, Marangolo P, Mylius V, Nitsche MA, Padberg F, Palm U, Poulet E, Priori A, Rossi S, Schecklmann M, Vanneste S, Ziemann U, Garcia-Larrea L, Paulus W. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS). Clin Neurophysiol. 2017;128:56–92.
Lefaucheur JP, Aleman A, Baeken C, Benninger DH, Brunelin J, Di Lazzaro V, Filipović SR, Grefkes C, Hasan A, Hummel FC, Jääskeläinen SK, Langguth B, Leocani L, Londero A, Nardone R, Nguyen JP, Nyffeler T, Oliveira-Maia AJ, Oliviero A, Padberg F, Palm U, Paulus W, Poulet E, Quartarone A, Rachid F, Rektorová I, Rossi S, Sahlsten H, Schecklmann M, Szekely D, Ziemann U. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): An update (2014–2018). Clin Neurophysiol. 2020;131:474–528.
Soleimani R, Jalali MM, Hasandokht T. Therapeutic impact of repetitive transcranial magnetic stimulation (rTMS) on tinnitus: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2016;273:1663–75.
Lefebvre-Demers M, Doyon N, Fecteau S. Non-invasive neuromodulation for tinnitus: A meta-analysis and modeling studies. Brain Stimul. 2021;14:113–28.
Chen S, Du M, Wang Y, Li Y, Tong B, Qiu J, Wu F, Liu Y. State of the art: non-invasive electrical stimulation for the treatment of chronic tinnitus. Ther Adv Chronic Dis. 2023;14:20406223221148060.
Maudoux A, Lefebvre P, Cabay J-E, Demertzi A, Vanhaudenhuyse A, Laureys S, et al. Auditory resting-state network connectivity in tinnitus: a functional MRI study. PLoS ONE. 2012;7: e36222.
Mirz F, Pedersen B, Ishizu K, Johannsen P, Ovesen T, Stødkilde-Jørgensen H, Gjedde A. Positron emission tomography of cortical centers of tinnitus. Hear Res. 1999;134:133–44.
Burton H, Wineland A, Bhattacharya M, Nicklaus J, Garcia KS, Piccirillo JF. Altered networks in bothersome tinnitus: a functional connectivity study. BMC Neurosci. 2012;13:3.
Yadollahpour A, Bayat A, Rashidi S, Saki N, Karimi M. Dataset of acute repeated sessions of bifrontal transcranial direct current stimulation for treatment of intractable tinnitus: A randomized controlled trial. Data Brief. 2017;15:40–6.
Yadollahpour A, Mayo M, Saki N, Rashidi S, Bayat A. A chronic protocol of bilateral transcranial direct current stimulation over auditory cortex for tinnitus treatment: Dataset from a double-blinded randomized controlled trial. F1000Res. 2018;7:733.
Vanneste S, Plazier M, Ost J, van der Loo E, Van de Heyning P, De Ridder D. Bilateral dorsolateral prefrontal cortex modulation for tinnitus by transcranial direct current stimulation: a preliminary clinical study. Exp Brain Res. 2010;202:779–85.
Datta A, Bansal V, Diaz J, Patel J, Reato D, Bikson M. Gyri-precise head model of transcranial direct current stimulation: improved spatial focality using a ring electrode versus conventional rectangular pad. Brain Stimul. 2009;2(201–7):207.e1.
Vanneste S, Fregni F, De Ridder D. Head-to-head comparison of transcranial random noise stimulation, transcranial AC stimulation, and transcranial DC stimulation for tinnitus. Front Psychiatry. 2013;4:158.
Vanneste S, Walsh V, Van De Heyning P, De Ridder D. Comparing immediate transient tinnitus suppression using tACS and tDCS: a placebo-controlled study. Exp Brain Res. 2013;226:25–31.
Claes L, Stamberger H, Van de Heyning P, De Ridder D, Vanneste S. Auditory cortex tACS and tRNS for tinnitus: single versus multiple sessions. Neural Plast. 2014;2014436713.
Mohsen S, Pourbakht A, Farhadi M, Mahmoudian S. The efficacy and safety of multiple sessions of multisite transcranial random noise stimulation in treating chronic tinnitus. Braz J Otorhinolaryngol. 2019;85:628–35.
Kreuzer PM, Poeppl TB, Rupprecht R, Vielsmeier V, Lehner A, Langguth B, Schecklmann M. Daily high-frequency transcranial random noise stimulation of bilateral temporal cortex in chronic tinnitus - a pilot study. Sci Rep. 2019;9:12274.
Joos K, De Ridder D, Vanneste S. The differential effect of low- versus high-frequency random noise stimulation in the treatment of tinnitus. Exp Brain Res. 2015;233:1433–40.
Manta S, Dong J, Debonnel G, Blier P. Enhancement of the function of rat serotonin and norepinephrine neurons by sustained vagus nerve stimulation. J Psychiatry Neurosci. 2009;34:272–80.
Edeline JM, Manunta Y, Hennevin E. Induction of selective plasticity in the frequency tuning of auditory cortex and auditory thalamus neurons by locus coeruleus stimulation. Hear Res. 2011;274:75–84.
Fernández-Hernando D, Fernández-de-Las-Peñas C, Machado-Martín A, Angulo-Díaz-Parreño S, García-Esteo FJ, Mesa-Jiménez JA. Effects of Non-Invasive Neuromodulation of the Vagus Nerve for Management of Tinnitus: A Systematic Review with Meta-Analysis. J Clin Med. 2023;12:3673.
Engineer ND, Riley JR, Seale JD, Vrana WA, Shetake JA, Sudanagunta SP, Borland MS, Kilgard MP. Reversing pathological neural activity using targeted plasticity. Nature. 2011;470(7332):101–4.
Markovitz CD, Smith BT, Gloeckner CD, Lim HH. Investigating a new neuromodulation treatment for brain disorders using synchronized activation of multimodal pathways. Sci Rep. 2015;5:9462.
Tyler R, Cacace A, Stocking C, Tarver B, Engineer N, Martin J, Deshpande A, Stecker N, Pereira M, Kilgard M, Burress C, Pierce D, Rennaker R, Vanneste S. Vagus Nerve Stimulation Paired with Tones for the Treatment of Tinnitus: A Prospective Randomized Double-blind Controlled Pilot Study in Humans. Sci Rep. 2017;7:11960.
Conlon B, Langguth B, Hamilton C, Hughes S, Meade E, Connor CO, Schecklmann M, Hall DA, Vanneste S, Leong SL, Subramaniam T, D'Arcy S, Lim HH. Bimodal neuromodulation combining sound and tongue stimulation reduces tinnitus symptoms in a large randomized clinical study. Sci Transl Med. 2020;12:eabb2830.
Conlon B, Hamilton C, Meade E, Leong SL, O Connor C, Langguth B, Vanneste S, Hall DA, Hughes S, Lim HH. Different bimodal neuromodulation settings reduce tinnitus symptoms in a large randomized trial. Sci Rep. 2022;12:10845. The largest clinical trial, although no placebo-controlled, on bimodal neuromodulation in tinnitus.
Acknowledgements
The authors wish to thank Dr. Massimo Cincotta for reviewing their manuscript.
Funding
Open access funding provided by Università degli Studi di Siena within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
SR and MM conceived and wrote the paper.
Corresponding author
Ethics declarations
Competing Interest
The authors declare no competing interest, Simone Rossi and Marco Mandalà have no potential conflicts of interest.
Human and Animal Rights And Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rossi, S., Mandalà, M. TINNITUS. A Non-invasive Neuromodulatory Perspective. Curr Treat Options Neurol (2024). https://doi.org/10.1007/s11940-024-00802-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s11940-024-00802-w