Abstract
Purpose of Review
Alzheimer’s disease and related dementias are the source of significant distress, impairment, and caregiver burden in aging populations. A prominent reason for this impact is the Behavioral and Psychological Symptoms of Dementia (BPSD). Common BPSD include disruptive behaviors, such as agitation, aggression, severe anxiety, delusions, depression, apathy, and sleep disturbances. Specific dementias, such as behavioral variant frontotemporal dementia and dementia with Lewy bodies, are associated with socioemotional disturbances and visual hallucinations, respectively. The aim of this review is to present current treatment options for the major BPSD.
Recent Findings
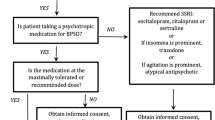
The management of the BPSD requires familiarity with non-pharmacological interventions and skill in the use of pharmacological agents in patients with dementias. This review outlines five important areas of non-pharmacological intervention. It then discusses the use of serotonergic medications, before considering antipsychotic drugs for disruptive behaviors and other BPSD. What is known about psychoactive drug use in cognitively normal populations does not necessarily apply to those with dementia, and the current treatment of patients with dementia emphasizes the need to consider their increased susceptibility to side effects from antipsychotic drugs.
Summary
Effective dementia care requires knowing both non-pharmacological and pharmacological interventions for the BPSD, which are present in nearly all patients with dementia at some time in their course. This review presents relatively easily applicable non-pharmacological techniques followed by discussions of the medication options for the major BPSD. In particular, clinicians need to understand current treatment strategies, particularly with regards to psychoactive medications, in this vulnerable population.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Magierski R, Sobow T, Schwertner E, Religa D. Pharmacotherapy of behavioral and psychological symptoms of dementia: state of the art and future progress. Front Pharmacol. 2020;11:1168. https://doi.org/10.3389/fphar.2020.01168.
Chen A, Copeli F, Metzger E, Cloutier A, Osser DN. The psychopharmacology algorithm project at the Harvard South Shore Program: an update on management of behavioral and psychological symptoms in dementia. Psychiatry Res. 2021;295: 113641. https://doi.org/10.1016/j.psychres.2020.113641.
Ornstein K, Gaugler JE. The problem with “problem behaviors”: a systematic review of the association between individual patient behavioral and psychological symptoms and caregiver depression and burden within the dementia patient-caregiver dyad. Int Psychogeriatrics / IPA. 2012;24(10):1536–52. https://doi.org/10.1017/S1041610212000737.
Hiyoshi-Taniguchi K, Becker CB, Kinoshita A. What behavioral and psychological symptoms of dementia affect caregiver burnout? Clin Gerontol. 2018;41(3):249–54. https://doi.org/10.1080/07317115.2017.1398797.
Gaugler JE, Yu F, Krichbaum K, Wyman JF. Predictors of nursing home admission for persons with dementia. Med Care. 2009;47(2):191–8. https://doi.org/10.1097/MLR.0b013e31818457ce.
Feast A, Moniz-Cook E, Stoner C, Charlesworth G, Orrell M. A systematic review of the relationship between behavioral and psychological symptoms (BPSD) and caregiver well-being. Int Psychogeriatrics / IPA. 2016;28(11):1761–74. https://doi.org/10.1017/S1041610216000922.
Terum TM, Andersen JR, Rongve A, Aarsland D, Svendsboe EJ, Testad I. The relationship of specific items on the Neuropsychiatric Inventory to caregiver burden in dementia: a systematic review. Int J Geriatr Psychiatry. 2017;32(7):703–17. https://doi.org/10.1002/gps.4704.
Vandepitte S, Putman K, Van Den Noortgate N, Verhaeghe S, Mormont E, Van Wilder L, De Smedt D, Annemans L. Factors associated with the caregivers’ desire to institutionalize persons with dementia: a cross-sectional study. Dement Geriatr Cogn Disord. 2018;46(5–6):298–309. https://doi.org/10.1159/000494023.
Kameoka N, Sumitani S, Ohmori T. Behavioral and psychological symptoms of dementia (BPSD) and care burden: examination in the facility staff for elderly residents. J Med Invest. 2020;67(3.4):236–239. https://doi.org/10.2152/jmi.67.236.
Cummings J, Ritter A, Rothenberg K. Advances in management of neuropsychiatric syndromes in neurodegenerative diseases. Curr Psychiatry Rep. 2019;21(8):79. https://doi.org/10.1007/s11920-019-1058-4.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–9. https://doi.org/10.1016/j.jalz.2011.03.005.
Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, van Swieten JC, Seelaar H, Dopper EG, Onyike CU, Hillis AE, Josephs KA, Boeve BF, Kertesz A, Seeley WW, Rankin KP, Johnson JK, Gorno-Tempini ML, Rosen H, Prioleau-Latham CE, Lee A, Kipps CM, Lillo P, Piguet O, Rohrer JD, Rossor MN, Warren JD, Fox NC, Galasko D, Salmon DP, Black SE, Mesulam M, Weintraub S, Dickerson BC, Diehl-Schmid J, Pasquier F, Deramecourt V, Lebert F, Pijnenburg Y, Chow TW, Manes F, Grafman J, Cappa SF, Freedman M, Grossman M, Miller BL. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134(Pt 9):2456–77. https://doi.org/10.1093/brain/awr179.
McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor JP, Weintraub D, Aarsland D, Galvin J, Attems J, Ballard CG, Bayston A, Beach TG, Blanc F, Bohnen N, Bonanni L, Bras J, Brundin P, Burn D, Chen-Plotkin A, Duda JE, El-Agnaf O, Feldman H, Ferman TJ, Ffytche D, Fujishiro H, Galasko D, Goldman JG, Gomperts SN, Graff-Radford NR, Honig LS, Iranzo A, Kantarci K, Kaufer D, Kukull W, Lee VMY, Leverenz JB, Lewis S, Lippa C, Lunde A, Masellis M, Masliah E, McLean P, Mollenhauer B, Montine TJ, Moreno E, Mori E, Murray M, O’Brien JT, Orimo S, Postuma RB, Ramaswamy S, Ross OA, Salmon DP, Singleton A, Taylor A, Thomas A, Tiraboschi P, Toledo JB, Trojanowski JQ, Tsuang D, Walker Z, Yamada M, Kosaka K. Diagnosis and management of dementia with Lewy bodies: fourth consensus report of the DLB Consortium. Neurology. 2017;89(1):88–100. https://doi.org/10.1212/WNL.0000000000004058.
Zhao QF, Tan L, Wang HF, Jiang T, Tan MS, Tan L, Xu W, Li JQ, Wang J, Lai TJ, Yu JT. The prevalence of neuropsychiatric symptoms in Alzheimer’s disease: systematic review and meta-analysis. J Affect Disord. 2016;190:264–71. https://doi.org/10.1016/j.jad.2015.09.069.
Olazaran J, Reisberg B, Clare L, Cruz I, Pena-Casanova J, Del Ser T, Woods B, Beck C, Auer S, Lai C, Spector A, Fazio S, Bond J, Kivipelto M, Brodaty H, Rojo JM, Collins H, Teri L, Mittelman M, Orrell M, Feldman HH, Muniz R. Nonpharmacological therapies in Alzheimer’s disease: a systematic review of efficacy. Dement Geriatr Cogn Disord. 2010;30(2):161–78. https://doi.org/10.1159/000316119.
Ayalon L, Gum AM, Feliciano L, Arean PA. Effectiveness of nonpharmacological interventions for the management of neuropsychiatric symptoms in patients with dementia: a systematic review. Arch Intern Med. 2006;166(20):2182–8. https://doi.org/10.1001/archinte.166.20.2182.
Brodaty H, Arasaratnam C. Meta-analysis of nonpharmacological interventions for neuropsychiatric symptoms of dementia. Am J Psychiatry. 2012;169(9):946–53. https://doi.org/10.1176/appi.ajp.2012.11101529.
Yury CA, Fisher JE. Meta-analysis of the effectiveness of atypical antipsychotics for the treatment of behavioural problems in persons with dementia. Psychother Psychosom. 2007;76(4):213–8. https://doi.org/10.1159/000101499.
Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry. 2006;14(3):191–210. https://doi.org/10.1097/01.JGP.0000200589.01396.6d.
Dyer SM, Harrison SL, Laver K, Whitehead C, Crotty M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int Psychogeriatrics / IPA. 2018;30(3):295–309. https://doi.org/10.1017/S1041610217002344.
• Aigbogun MS, Cloutier M, Gauthier-Loiselle M, Guerin A, Ladouceur M, Baker RA, Grundman M, Duffy RA, Hartry A, Gwin K, Fillit H. Real-world treatment patterns and characteristics among patients with agitation and dementia in the United States: findings from a large, observational, retrospective chart review. J Alzheimers Dis 2020;77(3):1181–1194. https://doi.org/10.3233/JAD-200127. This is an important review of the issues and difficulties in implementing nonpharmacological interventions without quickly resorting the medications for the BPSD.
• Watt JA, Goodarzi Z, Veroniki AA, Nincic V, Khan PA, Ghassemi M, Thompson Y, Tricco AC, Straus SE. Comparative efficacy of interventions for aggressive and agitated behaviors in dementia: a systematic review and network meta-analysis. Ann Intern Med. 2019;171(9):633–642. https://doi.org/10.7326/M19-0993. The authors discuss non-pharmacological interventions for disruptive behaviors in comparison to other interventions.
Leng M, Zhao Y, Wang Z. Comparative efficacy of non-pharmacological interventions on agitation in people with dementia: a systematic review and Bayesian network meta-analysis. Int J Nurs Stud. 2020;102: 103489. https://doi.org/10.1016/j.ijnurstu.2019.103489.
Tonga JB, Saltyte Benth J, Arnevik EA, Werheid K, Korsnes MS, Ulstein ID. Managing depressive symptoms in people with mild cognitive impairment and mild dementia with a multicomponent psychotherapy intervention: a randomized controlled trial. Int Psychogeriatrics / IPA. 2021;33(3):217–31. https://doi.org/10.1017/S1041610220000216.
Rodrigues S, Silva JMD, Oliveira MCC, Santana CMF, Carvalho KM, Barbosa B. Physical exercise as a non-pharmacological strategy for reducing behavioral and psychological symptoms in elderly with mild cognitive impairment and dementia: a systematic review of randomized clinical trials. Arq Neuropsiquiatr. 2021;79(12):1129–37. https://doi.org/10.1590/0004-282X-ANP-2020-0539.
Garcia-Alberca JM. Cognitive intervention therapy as treatment for behaviour disorders in Alzheimer disease: evidence on efficacy and neurobiological correlations. Neurologia (Barcelona, Spain). 2015;30(1):8–15. https://doi.org/10.1016/j.nrl.2012.10.002.
Tariot PN. Treatment strategies for agitation and psychosis in dementia. J Clin Psychiatry. 1996;57(Suppl 14):21–9.
Kobayashi H, Ohnishi T, Nakagawa R, Yoshizawa K. The comparative efficacy and safety of cholinesterase inhibitors in patients with mild-to-moderate Alzheimer’s disease: a Bayesian network meta-analysis. Int J Geriatr Psychiatry. 2016;31(8):892–904. https://doi.org/10.1002/gps.4405.
Jin B, Liu H. Comparative efficacy and safety of therapy for the behavioral and psychological symptoms of dementia: a systemic review and Bayesian network meta-analysis. J Neurol. 2019;266(10):2363–75. https://doi.org/10.1007/s00415-019-09200-8.
Cummings JL, Schneider E, Tariot PN, Graham SM, Memantine MEMMDSG. Behavioral effects of memantine in Alzheimer disease patients receiving donepezil treatment. Neurology. 2006;67(1):57–63. https://doi.org/10.1212/01.wnl.0000223333.42368.f1.
Wilcock GK, Ballard CG, Cooper JA, Loft H. Memantine for agitation/aggression and psychosis in moderately severe to severe Alzheimer’s disease: a pooled analysis of 3 studies. J Clin Psychiatry. 2008;69(3):341–8. https://doi.org/10.4088/jcp.v69n0302.
•• Ringman JM, Schneider L. Treatment options for agitation in dementia. Curr Treat Options Neurol. 2019;21:7–30. https://doi.org/10.1007/s11940-019-0572-3. This review is an exceptional discussion of current treatment options for agitation and related disruptive behavior in patients with dementia. It includes discussion of the potential problems in reverting to antipsychotic medications without considering other medications.
Halpern R, Seare J, Tong J, Hartry A, Olaoye A, Aigbogun MS. Using electronic health records to estimate the prevalence of agitation in Alzheimer disease/dementia. Int J Geriatr Psychiatry. 2019;34(3):420–31. https://doi.org/10.1002/gps.5030.
Davies SJ, Burhan AM, Kim D, Gerretsen P, Graff-Guerrero A, Woo VL, Kumar S, Colman S, Pollock BG, Mulsant BH, Rajji TK. Sequential drug treatment algorithm for agitation and aggression in Alzheimer’s and mixed dementia. J Psychopharmacol. 2018;32(5):509–23. https://doi.org/10.1177/0269881117744996.
Grippe TC, Goncalves BS, Louzada LL, Quintas JL, Naves JO, Camargos EF, Nobrega OT. Circadian rhythm in Alzheimer disease after trazodone use. Chronobiol Int. 2015;32(9):1311–4. https://doi.org/10.3109/07420528.2015.1077855.
Seitz DP, Adunuri N, Gill SS, Gruneir A, Herrmann N, Rochon P. Antidepressants for agitation and psychosis in dementia. Cochrane Database Syst Rev. 2011;(2):CD008191. https://doi.org/10.1002/14651858.CD008191.pub2.
Viscogliosi G, Chiriac IM, Ettorre E. Efficacy and safety of citalopram compared to atypical antipsychotics on agitation in nursing home residents with Alzheimer dementia. J Am Med Dir Assoc. 2017;18(9):799–802. https://doi.org/10.1016/j.jamda.2017.06.010.
Porsteinsson AP, Antonsdottir IM. An update on the advancements in the treatment of agitation in Alzheimer’s disease. Expert Opin Pharmacother. 2017;18(6):611–20. https://doi.org/10.1080/14656566.2017.1307340.
Porsteinsson AP, Drye LT, Pollock BG, Devanand DP, Frangakis C, Ismail Z, Marano C, Meinert CL, Mintzer JE, Munro CA, Pelton G, Rabins PV, Rosenberg PB, Schneider LS, Shade DM, Weintraub D, Yesavage J, Lyketsos CG, Cit ADRG. Effect of citalopram on agitation in Alzheimer disease: the CitAD randomized clinical trial. JAMA. 2014;311(7):682–91. https://doi.org/10.1001/jama.2014.93.
Weintraub D, Drye LT, Porsteinsson AP, Rosenberg PB, Pollock BG, Devanand DP, Frangakis C, Ismail Z, Marano C, Meinert CL, Mintzer JE, Munro CA, Pelton G, Rabins PV, Schneider LS, Shade DM, Yesavage J, Lyketsos CG, Cit ADRG. Time to response to citalopram treatment for agitation in Alzheimer disease. Am J Geriatr Psychiatry. 2015;23(11):1127–33. https://doi.org/10.1016/j.jagp.2015.05.006.
•• Reus VI, Fochtmann LJ, Eyler AE, Hilty DM, Horvitz-Lennon M, Jibson MD, Lopez OL, Mahoney J, Pasic J, Tan ZS, Wills CD, Rhoads R, Yager J. The American Psychiatric Association practice guideline on the use of antipsychotics to treat agitation or psychosis in patients with dementia. Am J Psychiatry. 2016;173(5):543–546. https://doi.org/10.1176/appi.ajp.2015.173501. The authors provide guidance and guidelines for considering the use of antipsychotic medications for agitation and psychosis in those with dementia.
Desai VC, Heaton PC, Kelton CM. Impact of the Food and Drug Administration’s antipsychotic black box warning on psychotropic drug prescribing in elderly patients with dementia in outpatient and office-based settings. Alzheimers Dement. 2012;8(5):453–7. https://doi.org/10.1016/j.jalz.2011.08.004.
Norgaard A, Jensen-Dahm C, Gasse C, Hansen HV, Waldemar G. Time trends in antipsychotic drug use in patients with dementia: a nationwide study. J Alzheimers Dis. 2016;49(1):211–20. https://doi.org/10.3233/JAD-150481.
Rios S, Perlman CM, Costa A, Heckman G, Hirdes JP, Mitchell L. Antipsychotics and dementia in Canada: a retrospective cross-sectional study of four health sectors. BMC Geriatr. 2017;17(1):244. https://doi.org/10.1186/s12877-017-0636-8.
Jessop T, Harrison F, Cations M, Draper B, Chenoweth L, Hilmer S, Westbury J, Low LF, Heffernan M, Sachdev P, Close J, Blennerhassett J, Marinkovich M, Shell A, Brodaty H. Halting Antipsychotic Use in Long-Term care (HALT): a single-arm longitudinal study aiming to reduce inappropriate antipsychotic use in long-term care residents with behavioral and psychological symptoms of dementia. Int Psychogeriatrics / IPA. 2017;29(8):1391–403. https://doi.org/10.1017/S1041610217000084.
Kirkham J, Sherman C, Velkers C, Maxwell C, Gill S, Rochon P, Seitz D. Antipsychotic use in dementia. Can J Psychiatry. 2017;62(3):170–81. https://doi.org/10.1177/0706743716673321.
Seitz DP, Gill SS, Herrmann N, Brisbin S, Rapoport MJ, Rines J, Wilson K, Le Clair K, Conn DK. Pharmacological treatments for neuropsychiatric symptoms of dementia in long-term care: a systematic review. Int Psychogeriatrics / IPA. 2013;25(2):185–203. https://doi.org/10.1017/S1041610212001627.
Yunusa I, Alsumali A, Garba AE, Regestein QR, Eguale T. Assessment of reported comparative effectiveness and safety of atypical antipsychotics in the treatment of behavioral and psychological symptoms of dementia: a network meta-analysis. JAMA Netw Open. 2019;2(3): e190828. https://doi.org/10.1001/jamanetworkopen.2019.0828.
Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294(15):1934–43. https://doi.org/10.1001/jama.294.15.1934.
Kales HC, Kim HM, Zivin K, Valenstein M, Seyfried LS, Chiang C, Cunningham F, Schneider LS, Blow FC. Risk of mortality among individual antipsychotics in patients with dementia. Am J Psychiatry. 2012;169(1):71–9. https://doi.org/10.1176/appi.ajp.2011.11030347.
Ma H, Huang Y, Cong Z, Wang Y, Jiang W, Gao S, Zhu G. The efficacy and safety of atypical antipsychotics for the treatment of dementia: a meta-analysis of randomized placebo-controlled trials. J Alzheimers Dis. 2014;42(3):915–37. https://doi.org/10.3233/JAD-140579.
Ralph SJ, Espinet AJ. Increased all-cause mortality by antipsychotic drugs: updated review and meta-analysis in dementia and general mental health care. J Alzheimers Dis Rep. 2018;2(1):1–26. https://doi.org/10.3233/ADR-170042.
Schneider LS, Tariot PN, Dagerman KS, Davis SM, Hsiao JK, Ismail MS, Lebowitz BD, Lyketsos CG, Ryan JM, Stroup TS, Sultzer DL, Weintraub D, Lieberman JA, Group C-AS. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer’s disease. N Engl J Med. 2006;355(15):1525–38. https://doi.org/10.1056/NEJMoa061240.
Ismail MS, Dagerman K, Tariot PN, Abbott S, Kavanagh S, Schneider LS. National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness-Alzheimer’s Disease (CATIE-AD): baseline characteristics. Curr Alzheimer Res. 2007;4(3):325–35. https://doi.org/10.2174/156720507781077214.
Sultzer DL, Davis SM, Tariot PN, Dagerman KS, Lebowitz BD, Lyketsos CG, Rosenheck RA, Hsiao JK, Lieberman JA, Schneider LS, Group C-AS. Clinical symptom responses to atypical antipsychotic medications in Alzheimer’s disease: phase 1 outcomes from the CATIE-AD effectiveness trial. Am J Psychiatry. 2008;165(7):844–54. https://doi.org/10.1176/appi.ajp.2008.07111779.
Maust DT, Kim HM, Seyfried LS, Chiang C, Kavanagh J, Schneider LS, Kales HC. Antipsychotics, other psychotropics, and the risk of death in patients with dementia: number needed to harm. JAMA Psychiat. 2015;72(5):438–45. https://doi.org/10.1001/jamapsychiatry.2014.3018.
Rochon PA, Normand SL, Gomes T, Gill SS, Anderson GM, Melo M, Sykora K, Lipscombe L, Bell CM, Gurwitz JH. Antipsychotic therapy and short-term serious events in older adults with dementia. Arch Intern Med. 2008;168(10):1090–6. https://doi.org/10.1001/archinte.168.10.1090.
Steinberg M, Lyketsos CG. Atypical antipsychotic use in patients with dementia: managing safety concerns. Am J Psychiatry. 2012;169(9):900–6. https://doi.org/10.1176/appi.ajp.2012.12030342.
Van der Spek K, Gerritsen DL, Smalbrugge M, Nelissen-Vrancken MH, Wetzels RB, Smeets CH, Zuidema SU, Koopmans RT. Only 10% of the psychotropic drug use for neuropsychiatric symptoms in patients with dementia is fully appropriate. The Proper I-study. Int Psychogeriatrics / IPA. 2016;28(10):1589–1595. https://doi.org/10.1017/S104161021600082X.
Kongpakwattana K, Sawangjit R, Tawankanjanachot I, Bell JS, Hilmer SN, Chaiyakunapruk N. Pharmacological treatments for alleviating agitation in dementia: a systematic review and network meta-analysis. Br J Clin Pharmacol. 2018;84(7):1445–56. https://doi.org/10.1111/bcp.13604.
Lonergan E, Luxenberg J, Colford J. Haloperidol for agitation in dementia. Cochrane Database Syst Rev. 2002;(2):CD002852. https://doi.org/10.1002/14651858.CD002852.
Katz I, de Deyn PP, Mintzer J, Greenspan A, Zhu Y, Brodaty H. The efficacy and safety of risperidone in the treatment of psychosis of Alzheimer’s disease and mixed dementia: a meta-analysis of 4 placebo-controlled clinical trials. Int J Geriatr Psychiatry. 2007;22(5):475–84. https://doi.org/10.1002/gps.1792.
Street JS, Clark WS, Gannon KS, Cummings JL, Bymaster FP, Tamura RN, Mitan SJ, Kadam DL, Sanger TM, Feldman PD, Tollefson GD, Breier A. Olanzapine treatment of psychotic and behavioral symptoms in patients with Alzheimer disease in nursing care facilities: a double-blind, randomized, placebo-controlled trial. The HGEU Study Group. Arch Gen Psychiatry. 2000;57(10):968–976. https://doi.org/10.1001/archpsyc.57.10.968.
Mulsant BH, Gharabawi GM, Bossie CA, Mao L, Martinez RA, Tune LE, Greenspan AJ, Bastean JN, Pollock BG. Correlates of anticholinergic activity in patients with dementia and psychosis treated with risperidone or olanzapine. J Clin Psychiatry. 2004;65(12):1708–14. https://doi.org/10.4088/jcp.v65n1217.
Lanctot KL, Amatniek J, Ancoli-Israel S, Arnold SE, Ballard C, Cohen-Mansfield J, Ismail Z, Lyketsos C, Miller DS, Musiek E, Osorio RS, Rosenberg PB, Satlin A, Steffens D, Tariot P, Bain LJ, Carrillo MC, Hendrix JA, Jurgens H, Boot B. Neuropsychiatric signs and symptoms of Alzheimer’s disease: new treatment paradigms. Alzheimers Dement (N Y). 2017;3(3):440–9. https://doi.org/10.1016/j.trci.2017.07.001.
De Deyn PP, Katz IR, Brodaty H, Lyons B, Greenspan A, Burns A. Management of agitation, aggression, and psychosis associated with dementia: a pooled analysis including three randomized, placebo-controlled double-blind trials in nursing home residents treated with risperidone. Clin Neurol Neurosurg. 2005;107(6):497–508. https://doi.org/10.1016/j.clineuro.2005.03.013.
Rocha FL, Hara C, Ramos MG, Kascher GG, Santos MA, de Oliveira LG, Magalhaes Scoralick F. An exploratory open-label trial of ziprasidone for the treatment of behavioral and psychological symptoms of dementia. Dement Geriatr Cogn Disord. 2006;22(5–6):445–8. https://doi.org/10.1159/000095804.
Mintzer JE, Tune LE, Breder CD, Swanink R, Marcus RN, McQuade RD, Forbes A. Aripiprazole for the treatment of psychoses in institutionalized patients with Alzheimer dementia: a multicenter, randomized, double-blind, placebo-controlled assessment of three fixed doses. Am J Geriatr Psychiatry. 2007;15(11):918–31. https://doi.org/10.1097/JGP.0b013e3181557b47.
Streim JE, Porsteinsson AP, Breder CD, Swanink R, Marcus R, McQuade R, Carson WH. A randomized, double-blind, placebo-controlled study of aripiprazole for the treatment of psychosis in nursing home patients with Alzheimer disease. Am J Geriatr Psychiatry. 2008;16(7):537–50. https://doi.org/10.1097/JGP.0b013e318165db77.
Azermai M, Petrovic M, Engelborghs S, Elseviers MM, Van der Mussele S, Debruyne H, Van Bortel L, Vander Stichele RH. The effects of abrupt antipsychotic discontinuation in cognitively impaired older persons: a pilot study. Aging Ment Health. 2013;17(1):125–32. https://doi.org/10.1080/13607863.2012.717255.
Miarons M, Cabib C, Baron FJ, Rofes L. Evidence and decision algorithm for the withdrawal of antipsychotic treatment in the elderly with dementia and neuropsychiatric symptoms. Eur J Clin Pharmacol. 2017;73(11):1389–98. https://doi.org/10.1007/s00228-017-2314-3.
• Gedde MH, Husebo BS, Mannseth J, Kjome RLS, Naik M, Berge LI. Less is more: the impact of deprescribing psychotropic drugs on behavioral and psychological symptoms and daily functioning in nursing home patients. Results From the Cluster-Randomized Controlled COSMOS Trial. Am J Geriatr Psychiatry. 2021;29(3):304–315. https://doi.org/10.1016/j.jagp.2020.07.004. This article is a good review and discussion of the issue of withdrawing medications used for the BPSD and of how to approach this issue.
Declercq T, Petrovic M, Azermai M, Vander Stichele R, De Sutter AI, van Driel ML, Christiaens T. Withdrawal versus continuation of chronic antipsychotic drugs for behavioural and psychological symptoms in older people with dementia. Cochrane database Syst Rev. 2013;(3):CD007726. https://doi.org/10.1002/14651858.CD007726.pub2.
Gao RL, Lim KS, Luthra AS. Discontinuation of antipsychotics treatment for elderly patients within a specialized behavioural unit: a retrospective review. Int J Clin Pharm. 2021;43(1):212–9. https://doi.org/10.1007/s11096-020-01135-9.
Van Leeuwen E, Petrovic M, van Driel ML, De Sutter AI, Vander Stichele R, Declercq T, Christiaens T. Withdrawal versus continuation of long-term antipsychotic drug use for behavioural and psychological symptoms in older people with dementia. Cochrane Database Syst Rev. 2018;3:CD007726. https://doi.org/10.1002/14651858.CD007726.pub3.
Devanand DP, Mintzer J, Schultz SK, Andrews HF, Sultzer DL, de la Pena D, Gupta S, Colon S, Schimming C, Pelton GH, Levin B. Relapse risk after discontinuation of risperidone in Alzheimer’s disease. N Engl J Med. 2012;367(16):1497–507. https://doi.org/10.1056/NEJMoa1114058.
Baillon SF, Narayana U, Luxenberg JS, Clifton AV. Valproate preparations for agitation in dementia. Cochrane Database Syst Rev. 2018;10:CD003945. https://doi.org/10.1002/14651858.CD003945.pub4.
Suzuki H, Gen K. Clinical efficacy of lamotrigine and changes in the dosages of concomitantly used psychotropic drugs in Alzheimer’s disease with behavioural and psychological symptoms of dementia: a preliminary open-label trial. Psychogeriatrics : Official J Japanese Psychogeriatric Soc. 2015;15(1):32–7. https://doi.org/10.1111/psyg.12085.
Cummings JL, Lyketsos CG, Peskind ER, Porsteinsson AP, Mintzer JE, Scharre DW, De La Gandara JE, Agronin M, Davis CS, Nguyen U, Shin P, Tariot PN, Siffert J. Effect of dextromethorphan-quinidine on agitation in patients with Alzheimer disease dementia: a randomized clinical trial. JAMA. 2015;314(12):1242–54. https://doi.org/10.1001/jama.2015.10214.
van den Elsen GA, Ahmed AI, Verkes RJ, Kramers C, Feuth T, Rosenberg PB, van der Marck MA, Olde Rikkert MG. Tetrahydrocannabinol for neuropsychiatric symptoms in dementia: a randomized controlled trial. Neurology. 2015;84(23):2338–46. https://doi.org/10.1212/WNL.0000000000001675.
Naasan G, Shdo SM, Rodriguez EM, Spina S, Grinberg L, Lopez L, Karydas A, Seeley WW, Miller BL, Rankin KP. Psychosis in neurodegenerative disease: differential patterns of hallucination and delusion symptoms. Brain. 2021;144(3):999–1012. https://doi.org/10.1093/brain/awaa413.
Brommelhoff JA, Gatz M, Johansson B, McArdle JJ, Fratiglioni L, Pedersen NL. Depression as a risk factor or prodromal feature for dementia? Findings in a population-based sample of Swedish twins. Psychol Aging. 2009;24(2):373–84. https://doi.org/10.1037/a0015713.
Li G, Wang LY, Shofer JB, Thompson ML, Peskind ER, McCormick W, Bowen JD, Crane PK, Larson EB. Temporal relationship between depression and dementia: findings from a large community-based 15-year follow-up study. Arch Gen Psychiatry. 2011;68(9):970–7. https://doi.org/10.1001/archgenpsychiatry.2011.86.
Mirza SS, Wolters FJ, Swanson SA, Koudstaal PJ, Hofman A, Tiemeier H, Ikram MA. 10-year trajectories of depressive symptoms and risk of dementia: a population-based study. Lancet Psychiatry. 2016;3(7):628–35. https://doi.org/10.1016/S2215-0366(16)00097-3.
Magierski R, Sobow T. Serotonergic drugs for the treatment of neuropsychiatric symptoms in dementia. Expert Rev Neurother. 2016;16(4):375–87. https://doi.org/10.1586/14737175.2016.1155453.
Sepehry AA, Lee PE, Hsiung GY, Beattie BL, Jacova C. Effect of selective serotonin reuptake inhibitors in Alzheimer’s disease with comorbid depression: a meta-analysis of depression and cognitive outcomes. Drugs Aging. 2012;29(10):793–806. https://doi.org/10.1007/s40266-012-0012-5.
• Dudas R, Malouf R, McCleery J, Dening T. Antidepressants for treating depression in dementia. Cochrane Database Syst Rev. 2018;8:CD003944. https://doi.org/10.1002/14651858.CD003944.pub2. This Cochrane review focuses on the use of SSRI and other antidepressants for the treatment of depression among those with dementia.
Martin BK, Frangakis CE, Rosenberg PB, Mintzer JE, Katz IR, Porsteinsson AP, Schneider LS, Rabins PV, Munro CA, Meinert CL, Niederehe G, Lyketsos CG. Design of depression in Alzheimer’s Disease study-2. Am J Geriatr Psychiatry. 2006;14(11):920–30. https://doi.org/10.1097/01.JGP.0000240977.71305.ee.
Rosenberg PB, Drye LT, Martin BK, Frangakis C, Mintzer JE, Weintraub D, Porsteinsson AP, Schneider LS, Rabins PV, Munro CA, Meinert CL, Lyketsos CG, Group D-R. Sertraline for the treatment of depression in Alzheimer disease. Am J Geriatr Psychiatry. 2010;18(2):136–45. https://doi.org/10.1097/JGP.0b013e3181c796eb.
Weintraub D, Rosenberg PB, Drye LT, Martin BK, Frangakis C, Mintzer JE, Porsteinsson AP, Schneider LS, Rabins PV, Munro CA, Meinert CL, Lyketsos CG, Group D-R. Sertraline for the treatment of depression in Alzheimer disease: week-24 outcomes. Am J Geriatr Psychiatry. 2010;18(4):332–40. https://doi.org/10.1097/JGP.0b013e3181cc0333.
Katz IR. Depression in late life: psychiatric-medical comorbidity. Dialogues Clin Neurosci. 1999;1(2):81–94.
Tariot PN, Erb R, Podgorski CA, Cox C, Patel S, Jakimovich L, Irvine C. Efficacy and tolerability of carbamazepine for agitation and aggression in dementia. Am J Psychiatry. 1998;155(1):54–61. https://doi.org/10.1176/ajp.155.1.54.
de Vugt ME, Stevens F, Aalten P, Lousberg R, Jaspers N, Winkens I, Jolles J, Verhey FR. Behavioural disturbances in dementia patients and quality of the marital relationship. Int J Geriatr Psychiatry. 2003;18(2):149–54. https://doi.org/10.1002/gps.807.
Sepehry AA, Sarai M, Hsiung GR. Pharmacological therapy for apathy in Alzheimer’s disease: a systematic review and meta-analysis. Can J Neurol Sci. 2017;44(3):267–75. https://doi.org/10.1017/cjn.2016.426.
• Ruthirakuhan MT, Herrmann N, Abraham EH, Chan S, Lanctot KL. Pharmacological interventions for apathy in Alzheimer’s disease. Cochrane database Syst Rev. 2018;5:CD012197. https://doi.org/10.1002/14651858.CD012197.pub2. The authors present one of the best recent reviews of medications used to treat apathy among patients with Alzheimer’s disease.
Rosenberg PB, Lanctot KL, Drye LT, Herrmann N, Scherer RW, Bachman DL, Mintzer JE, Investigators A. Safety and efficacy of methylphenidate for apathy in Alzheimer’s disease: a randomized, placebo-controlled trial. J Clin Psychiatry. 2013;74(8):810–6. https://doi.org/10.4088/JCP.12m08099.
Padala PR, Padala KP, Lensing SY, Ramirez D, Monga V, Bopp MM, Roberson PK, Dennis RA, Petty F, Sullivan DH, Burke WJ. Methylphenidate for apathy in community-dwelling older veterans with mild Alzheimer’s disease: a double-blind, randomized, placebo-controlled trial. Am J Psychiatry. 2018;175(2):159–68. https://doi.org/10.1176/appi.ajp.2017.17030316.
•• Khoury R, Liu Y, Sheheryar Q, Grossberg GT. Pharmacotherapy for frontotemporal dementia. CNS Drugs. 2021;35(4):425–438 https://doi.org/10.1007/s40263-021-00813-0. This paper is a highly informative and well-organized review of the drug treatments available for the particular BPSD from bvFTD and related syndromes.
Mendez MF, Shapira JS, McMurtray A, Licht E. Preliminary findings: behavioral worsening on donepezil in patients with frontotemporal dementia. Am J Geriatr Psychiatry. 2007;15(1):84–7. https://doi.org/10.1097/01.JGP.0000231744.69631.33.
Lanctot KL, Herrmann N, Ganjavi H, Black SE, Rusjan PM, Houle S, Wilson AA. Serotonin-1A receptors in frontotemporal dementia compared with controls. Psychiatry Res. 2007;156(3):247–50. https://doi.org/10.1016/j.pscychresns.2007.07.003.
Procter AW, Qurne M, Francis PT. Neurochemical features of frontotemporal dementia. Dement Geriatr Cogn Disord. 1999;10(Suppl 1):80–4. https://doi.org/10.1159/000051219.
Yang Y, Schmitt HP. Frontotemporal dementia: evidence for impairment of ascending serotoninergic but not noradrenergic innervation. Immunocytochemical and quantitative study using a graph method. Acta Neuropathol. 2001;101(3):256–270. https://doi.org/10.1007/s004010000293.
Swartz JR, Miller BL, Lesser IM, Darby AL. Frontotemporal dementia: treatment response to serotonin selective reuptake inhibitors. J Clin Psychiatry. 1997;58(5):212–6.
Chow TW, Mendez MF. Goals in symptomatic pharmacologic management of frontotemporal lobar degeneration. Am J Alzheimers Dis Other Demen. 2002;17(5):267–72. https://doi.org/10.1177/153331750201700504.
Ljubenkov PA, Boxer AL. FTLD treatment: current practice and future possibilities. Adv Exp Med Biol. 2021;1281:297–310. https://doi.org/10.1007/978-3-030-51140-1_18.
Huey ED, Putnam KT, Grafman J. A systematic review of neurotransmitter deficits and treatments in frontotemporal dementia. Neurology. 2006;66(1):17–22. https://doi.org/10.1212/01.wnl.0000191304.55196.4d.
Prodan CI, Monnot M, Ross ED. Behavioural abnormalities associated with rapid deterioration of language functions in semantic dementia respond to sertraline. J Neurol Neurosurg Psychiatry. 2009;80(12):1416–7. https://doi.org/10.1136/jnnp.2009.173260.
• Trieu C, Gossink F, Stek ML, Scheltens P, Pijnenburg YAL, Dols A. Effectiveness of pharmacological interventions for symptoms of behavioral variant frontotemporal dementia: a systematic review. Cogn Behav Neurol. 2020;33(1):1–15. https://doi.org/10.1097/WNN.0000000000000217. The authors review the current knowledge of pharmacological interventions for the BPDS of bvFTD.
Lebert F, Stekke W, Hasenbroekx C, Pasquier F. Frontotemporal dementia: a randomised, controlled trial with trazodone. Dement Geriatr Cogn Disord. 2004;17(4):355–9. https://doi.org/10.1159/000077171.
Rahman S, Robbins TW, Hodges JR, Mehta MA, Nestor PJ, Clark L, Sahakian BJ. Methylphenidate (‘Ritalin’) can ameliorate abnormal risk-taking behavior in the frontal variant of frontotemporal dementia. Neuropsychopharmacology. 2006;31(3):651–8. https://doi.org/10.1038/sj.npp.1300886.
Huey ED, Garcia C, Wassermann EM, Tierney MC, Grafman J. Stimulant treatment of frontotemporal dementia in 8 patients. J Clin Psychiatry. 2008;69(12):1981–2. https://doi.org/10.4088/jcp.v69n1219a.
Hermann M, Waade RB, Molden E. Therapeutic drug monitoring of selective serotonin reuptake inhibitors in elderly patients. Ther Drug Monit. 2015;37(4):546–9. https://doi.org/10.1097/FTD.0000000000000169.
Devanand DP, Pelton GH, D’Antonio K, Strickler JG, Kreisl WC, Noble J, Marder K, Skomorowsky A, Huey ED. Low-dose lithium treatment for agitation and psychosis in Alzheimer disease and frontotemporal dementia: a case series. Alzheimer Dis Assoc Disord. 2017;31(1):73–5. https://doi.org/10.1097/WAD.0000000000000161.
Mendez MF, Shapira JS, Miller BL. Stereotypical movements and frontotemporal dementia. Mov Disord. 2005;20(6):742–5. https://doi.org/10.1002/mds.20465.
Meyer S, Mueller K, Gruenewald C, Grundl K, Marschhauser A, Tiepolt S, Barthel H, Sabri O, Schroeter ML. Citalopram improves obsessive-compulsive crossword puzzling in frontotemporal dementia. Case Rep Neurol. 2019;11(1):94–105. https://doi.org/10.1159/000495561.
Moretti R, Torre P, Antonello RM, Cazzato G, Bava A. Frontotemporal dementia: paroxetine as a possible treatment of behavior symptoms. A randomized, controlled, open 14-month study. Eur Neurol. 2003;49(1):13–19. https://doi.org/10.1159/000067021.
Deakin JB, Rahman S, Nestor PJ, Hodges JR, Sahakian BJ. Paroxetine does not improve symptoms and impairs cognition in frontotemporal dementia: a double-blind randomized controlled trial. Psychopharmacology. 2004;172(4):400–8. https://doi.org/10.1007/s00213-003-1686-5.
Cruz M, Marinho V, Fontenelle LF, Engelhardt E, Laks J. Topiramate may modulate alcohol abuse but not other compulsive behaviors in frontotemporal dementia: case report. Cogn Behav Neurol. 2008;21(2):104–6. https://doi.org/10.1097/WNN.0b013e31816bdf73.
Nestor PJ. Reversal of abnormal eating and drinking behaviour in a frontotemporal lobar degeneration patient using low-dose topiramate. J Neurol Neurosurg Psychiatry. 2012;83(3):349–50. https://doi.org/10.1136/jnnp.2010.238899.
Singam C, Walterfang M, Mocellin R, Evans A, Velakoulis D. Topiramate for abnormal eating behaviour in frontotemporal dementia. Behav Neurol. 2013;27(3):285–6. https://doi.org/10.3233/BEN-120257.
Shinagawa S, Tsuno N, Nakayama K. Managing abnormal eating behaviours in frontotemporal lobar degeneration patients with topiramate. Psychogeriatrics : Official J Japanese Psychogeriatric Soc. 2013;13(1):58–61. https://doi.org/10.1111/j.1479-8301.2012.00429.x.
Anneser JM, Jox RJ, Borasio GD. Inappropriate sexual behaviour in a case of ALS and FTD: successful treatment with sertraline. Amyotroph Lateral Scler. 2007;8(3):189–90. https://doi.org/10.1080/17482960601073543.
Black B, Muralee S, Tampi RR. Inappropriate sexual behaviors in dementia. J Geriatr Psychiatry Neurol. 2005;18(3):155–62. https://doi.org/10.1177/0891988705277541.
Guay DR. Inappropriate sexual behaviors in cognitively impaired older individuals. Am J Geriatr Pharmacother. 2008;6(5):269–88. https://doi.org/10.1016/j.amjopharm.2008.12.004.
Light SA, Holroyd S. The use of medroxyprogesterone acetate for the treatment of sexually inappropriate behaviour in patients with dementia. J Psychiatry Neurosci. 2006;31(2):132–4.
Poetter CE, Stewart JT. Treatment of indiscriminate, inappropriate sexual behavior in frontotemporal dementia with carbamazepine. J Clin Psychopharmacol. 2012;32(1):137–8. https://doi.org/10.1097/JCP.0b013e31823f91b9.
Galvez-Andres A, Blasco-Fontecilla H, Gonzalez-Parra S, Molina JD, Padin JM, Rodriguez RH. Secondary bipolar disorder and Diogenes syndrome in frontotemporal dementia: behavioral improvement with quetiapine and sodium valproate. J Clin Psychopharmacol. 2007;27(6):722–3. https://doi.org/10.1097/JCP.0b013e31815a57c1.
Jesso S, Morlog D, Ross S, Pell MD, Pasternak SH, Mitchell DG, Kertesz A, Finger EC. The effects of oxytocin on social cognition and behaviour in frontotemporal dementia. Brain. 2011;134(Pt 9):2493–501. https://doi.org/10.1093/brain/awr171.
Finger EC, MacKinley J, Blair M, Oliver LD, Jesso S, Tartaglia MC, Borrie M, Wells J, Dziobek I, Pasternak S, Mitchell DG, Rankin K, Kertesz A, Boxer A. Oxytocin for frontotemporal dementia: a randomized dose-finding study of safety and tolerability. Neurology. 2015;84(2):174–81. https://doi.org/10.1212/WNL.0000000000001133.
Cummings JL, Atri A, Ballard C, Boneva N, Frolich L, Molinuevo JL, Raket LL, Tariot PN. Insights into globalization: comparison of patient characteristics and disease progression among geographic regions in a multinational Alzheimer’s disease clinical program. Alzheimers Res Ther. 2018;10(1):116. https://doi.org/10.1186/s13195-018-0443-2.
O’Brien J, Taylor JP, Ballard C, Barker RA, Bradley C, Burns A, Collerton D, Dave S, Dudley R, Francis P, Gibbons A, Harris K, Lawrence V, Leroi I, McKeith I, Michaelides M, Naik C, O’Callaghan C, Olsen K, Onofrj M, Pinto R, Russell G, Swann P, Thomas A, Urwyler P, Weil RS, Ffytche D. Visual hallucinations in neurological and ophthalmological disease: pathophysiology and management. J Neurol Neurosurg Psychiatry. 2020;91(5):512–9. https://doi.org/10.1136/jnnp-2019-322702.
Watts KE, Storr NJ, Barr PG, Rajkumar AP. Systematic review of pharmacological interventions for people with Lewy body dementia. Aging Mental Health. 2022;1–14. https://doi.org/10.1080/13607863.2022.2032601.
Emre M, Tsolaki M, Bonuccelli U, Destee A, Tolosa E, Kutzelnigg A, Ceballos-Baumann A, Zdravkovic S, Bladstrom A, Jones R, Study I. Memantine for patients with Parkinson’s disease dementia or dementia with Lewy bodies: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2010;9(10):969–77. https://doi.org/10.1016/S1474-4422(10)70194-0.
Lee C, Shen YC. Aripiprazole improves psychotic, cognitive, and motor symptoms in a patient with Lewy body dementia. J Clin Psychopharmacol. 2017;37(5):628–30. https://doi.org/10.1097/JCP.0000000000000769.
Sugawara Kikuchi Y, Shimizu T. Aripiprazole for the treatment of psychotic symptoms in patients with dementia with Lewy bodies: a case series. Neuropsychiatr Dis Treat. 2019;15:543–7. https://doi.org/10.2147/NDT.S189050.
• Russo M, Carrarini C, Dono F, Rispoli MG, Di Pietro M, Di Stefano V, Ferri L, Bonanni L, Sensi SL, Onofrj M. The pharmacology of visual hallucinations in synucleinopathies. Front Pharmacol. 2019;10:1379. https://doi.org/10.3389/fphar.2019.01379. This reference is an excellent source for understanding visual hallucinations in DLB, and how to manage them.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mario F. Mendez declares that he has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Dementia
Rights and permissions
About this article
Cite this article
Mendez, M.F. Managing the Behavioral and Psychological Symptoms of Dementia. Curr Treat Options Neurol 24, 183–201 (2022). https://doi.org/10.1007/s11940-022-00715-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-022-00715-6