Abstract
Purpose of review
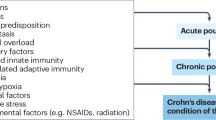
Pouchitis is common after restorative proctocolectomy and ileal pouch-anal anastomosis in patients with underlying ulcerative colitis. A majority of patients with acute antibiotic-responsive pouchitis develop chronic antibiotic-dependent pouchitis or antibiotic-refractory pouchitis. Contributing factors for chronic pouchitis include Clostridium difficile infection, the use of non-steroidal anti-inflammatory drugs, concurrent autoimmune disorders, surgical ischemia, and fecal stasis from structural or functional pouch outlet obstruction. Chronic antibiotic-refractory pouchitis is considered one of “difficult-to-treat” inflammatory bowel diseases (IBD).
Recent findings
While acute pouchitis often responds to oral antibiotic therapy, chronic pouchitis usually requires induction and maintenance therapy. Biological agents, particularly vedolizumab, may be used for the treatment of chronic pouchitis. The role of small molecule agents in the treatment of chronic pouchitis warrants further investigation. Fecal microbiota transplant, though effective in the eradication of Clostridium difficile of the pouch, has a limited therapeutic role in the management of chronic pouchitis. Hyperbaric oxygen therapy showed promising effects on chronic pouchitis.
Summary
Pouchitis represents a disease spectrum ranging from acute antibiotic-responsive to chronic antibiotic-refractory phenotypes. The treatment of chronic antibiotic-refractory pouchitis is similar to that of IBD, with confounding factors from surgery-associated ischemia and concurrent autoimmune disorders, particularly primary sclerosing cholangitis.

Similar content being viewed by others
Data Availability
All figures and tables are original and have never published before.
Abbreviations
- CADP:
-
Chronic antibiotic-dependent pouchitis
- CARP:
-
Chronic antibiotic-refractory pouchitis
- CD:
-
Crohn’s disease
- CDI:
-
Clostridium difficile Infection
- CDP:
-
Crohn’s disease of the pouch
- CT:
-
Computed tomography
- FAP:
-
Familial adenomatous polyposis
- FDA:
-
The Food and Drug Administration
- FODMAP:
-
Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols
- FMT:
-
Fecal microbiota transplant
- HOBT:
-
Hyperbaric oxygen therapy
- IBD:
-
Inflammatory bowel disease
- IPAA:
-
Ileal pouch-anal anastomosis
- IQR:
-
Interquartile range
- NSAID:
-
Non-steroidal anti-inflammatory drugs
- PDAI:
-
The Pouchitis Disease Activity Index
- RCT:
-
Randomized controlled trial
- TNF:
-
Tumor necrosis factor
- UC:
-
Ulcerative colitis
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Worley G, Almoudaris A, Bassett P, et al. Colectomy rates for ulcerative colitis in England 2003–2016. Aliment Pharmacol Ther. 2021;53:484–98.
Tsai L, Ma C, Dulai PS, et al. Contemporary risk of surgery in patients with ulcerative colitis and crohn’s disease: a meta-analysis of population-based cohorts. Clin Gastroenterol Hepatol. 2021;19:2031–45.
Dai N, Haidar O, Askari A, Segal JP. Colectomy rates in ulcerative colitis: a systematic review and meta-analysis. Dig Liver Dis. 2023;55:13–20.
Shaffer SR, Bernstein CN. Controversies in Crohn’s disease before and after pouch surgery. Dis Colon Rectum. 2022;65(S1):S45–9.
Akiyama S, Dyer EC, Rubin DT. Diagnostic and management considerations for the IPAA with Crohn’s disease-like features. Dis Colon Rectum. 2022;65(S1):S77–84.
Fazio VW, Kiran RP, Remzi FH, et al. Ileal pouch anal anastomosis: analysis of outcome and quality of life in 3707 patients. Ann Surg. 2013;257:679–85.
Shen B, Kochhar GS, Kariv R, et al. Diagnosis and classification of ileal pouch disorders: consensus guidelines from the International Ileal Pouch Consortium. Lancet Gastroenterol Hepatol. 2021;6:826–49.
Shen B, Kochhar GS, Rubin DT, et al. Treatment of pouchitis, Crohn’s disease, cuffitis, and other inflammatory disorders of the pouch: consensus guidelines from the International Ileal Pouch Consortium. Lancet Gastroenterol Hepatol. 2022;7:69–95.
Shen B, Kochhar GS, Navaneethan U, et al. Endoscopic evaluation of surgically altered bowel in inflammatory bowel disease: a consensus guideline from the Global Interventional Inflammatory Bowel Disease Group. Lancet Gastroenterol Hepatol. 2021;6:482–97. Erratum in: Lancet Gastroenterol Hepatol. 2021;6:e5.
Kiran RP, Kochhar GS, Kariv R, et al. Management of pouch neoplasia: consensus guidelines from the International Ileal Pouch Consortium. Lancet Gastroenterol Hepatol. 2022;7:871–93.
Santiago P, Barnes EL, Raffals LE. Classification and management of disorders of the j pouch [published online ahead of print, 2023 Jun 26]. Am J Gastroenterol. 2023.https://doi.org/10.14309/ajg.0000000000002348.
Gionchetti P, Rizzello F, Helwig U, et al. Prophylaxis of pouchitis onset with probiotic therapy: a double-blind, placebo-controlled trial. Gastroenterology. 2003;124:1202–9.
Yamamoto T, Shimoyama T, Bamba T, Matsumoto K. Consecutive monitoring of fecal calprotectin and lactoferrin for the early diagnosis and prediction of pouchitis after restorative proctocolectomy for ulcerative colitis. Am J Gastroenterol. 2015;110:881–7.
Madden MV, McIntyre AS, Nicholls RJ. Double-blind crossover trial of metronidazole versus placebo in chronic unremitting pouchitis. Dig Dis Sci. 1994;39:1193–216.
Shen B, Achkar JP, Lashner BA, et al. A randomized clinical trial of ciprofloxacin and metronidazole to treat acute pouchitis. Inflamm Bowel Dis. 2001;7:301–5.
Hassan Y, Connell WR, Rawal A, Wright EK. Review of long-term complications and functional outcomes of ileoanal pouch procedures in patients with inflammatory bowel disease. ANZ J Surg. 2023;93:1503–9.
• Parigi TL, D’Amico F, Abreu MT, et al. Difficult-to-treat inflammatory bowel disease: results from an international consensus meeting. Lancet Gastroenterol Hepatol. 2023;8:853–9. This consensus article from expert IBD specialists for the first time “officially” listed chronic antibiotic-refractory pouchitis is one of the 5 most difficult-to-treat IBD conditions.
Tome J, Raffals LE, Pardi DS. Management of acute and chronic pouchitis. Dis Colon Rectum. 2022;65(S1):S69–76. https://doi.org/10.1097/DCR.0000000000002562.
Navaneethan U, Venkatesh PG, Bennett AE, et al. Impact of budesonide on liver function tests and gut inflammation in patients with primary sclerosing cholangitis and ileal pouch-anal anastomosis. J Crohns Colitis. 2012;6:536–42.
Sambuelli A, Boerr L, Negreira S, et al. Budesonide enema in pouchitis-a double-blind, double-dummy, controlled trial. Aliment Pharmacol Ther. 2002;16:27–34.
•• Travis S, Silverberg MS, Danese S, et al. Vedolizumab for the treatment of chronic pouchitis. N Engl J Med. 2023;388:1191–200. This is the first phase4, double-blind, randomized, placeb controlled trial of vedolizumab for the treatment chronic antibiotic-dependent and chronic antibiotic-refractory pouchitis.
Ollech JE, Rubin DT, Glick L, et al. Ustekinumab is effective for the treatment of chronic antibiotic-refractory pouchitis. Dig Dis Sci. 2019;64:3596–601.
Rocchi C, Soliman YY, Massidda M, Vadalà di Prampero SF, Bulajic M, Sorrentino D. Is ustekinumab effective in refractory Crohn’s disease of the pouch and chronic pouchitis? a systematic review. Dig Dis Sci. 2022;67:1948–55.
Viazis N, Giakoumis M, Koukouratos T, et al. One-year infliximab administration for the treatment of chronic refractory pouchitis. Ann Gastroenterol. 2011;24:290–3.
Barreiro-de Acosta M, García-Bosch O, Souto R, et al. Efficacy of infliximab rescue therapy in patients with chronic refractory pouchitis: a multicenter study. Inflamm Bowel Dis. 2012;18:812–7.
Hata K, Ishihara S, Nozawa H, et al. Pouchitis after ileal pouch-anal anastomosis in ulcerative colitis: diagnosis, management, risk factors, and incidence. Dig Endosc. 2017;29:26–34.
Seril DN, Yao Q, Shen B. The association between autoimmunity and pouchitis. Inflamm Bowel Dis. 2014;20:378–88.
Quinn KP, Urquhart SA, Janssens LP, Lennon RJ, Chedid VG, Raffals LE. Primary sclerosing cholangitis-associated pouchitis: a distinct clinical phenotype. Clin Gastroenterol Hepatol. 2022;20:e964–73.
Wasmuth HH, Tranø G, Endreseth BH, Wibe A, Rydning A, Myrvold HE. Primary sclerosing cholangitis and extraintestinal manifestations in patients with ulcerative colitis and ileal pouch-anal anastomosis. J Gastrointest Surg. 2010;14:1099–104.
Kitajima T, Okita Y, Kawamura M, et al. The relationship between preoperative T helper cytokines in the ileal mucosa and the pathogenesis of pouchitis. BMC Gastroenterol. 2020;20:277.
Shen B, Plesec TP, Remer E, et al. Asymmetric endoscopic inflammation of the ileal pouch: a sign of ischemic pouchitis? Inflamm Bowel Dis. 2010;16:836–46.
• Gao XH, Yu GY, Khan F, et al. Greater peripouch fat area on CT image is associated with chronic pouchitis and pouch failure in inflammatory bowel disease patients. Dig Dis Sci. 2020;65:3660–71. This is one of series of articles on the pathogenetic role of the mesenteric fat and parapouch fat in chronic pouchitis. The findings suggest the role of adipose tissue along with gut microbiome and mucosal immunology in the development of chronic pouchitis and possible future therapeutic target.
Gao XH, Li JQ, Khan F, et al. Difference in the frequency of pouchitis between ulcerative colitis and familial adenomatous polyposis: is the explanation in peripouch fat? Colorectal Dis. 2019;21:1032–44.
Gao XH, Chouhan H, Liu GL, et al. Peripouch fat area measured on MRI image and its association with adverse pouch outcomes. Inflamm Bowel Dis. 2018;24:806–17.
Wu XR, Zhu H, Kiran RP, Remzi FH, Shen B. Excessive weight gain is associated with an increased risk for pouch failure in patients with restorative proctocolectomy. Inflamm Bowel Dis. 2013;19:2173–81.
Wu XR, Ashburn J, Remzi FH, Li Y, Fass H, Shen B. Male gender is associated with a high risk for chronic antibiotic-refractory pouchitis and ileal pouch anastomotic sinus. J Gastrointest Surg. 2016;20:631–9.
Achkar JP, Al-Haddad M, Lashner B, et al. Differentiating risk factors for acute and chronic pouchitis. Clin Gastroenterol Hepatol. 2005;3:60–6.
Lan N, Zhang L, Shen B. Post-index procedural gain in body mass index is associated with recurrent ileal pouch sinus after endoscopic or surgical therapy. Surg Endosc. 2020;34:2127–35.
Lan N, Hull TL, Shen B. Endoscopic sinusotomy versus redo surgery for the treatment of chronic pouch anastomotic sinus in ulcerative colitis patients. Gastrointest Endosc. 2019;89:144–56.
Shen B, Jiang ZD, Fazio VW, et al. Clostridium difficile infection in patients with ileal pouch-anal anastomosis. Clin Gastroenterol Hepatol. 2008;6:782–8.
Shore BM, Weaver KN, Allegretti JR, Herfarth HH, Barnes EL. Prevalence of Clostridioides difficile infection after ileal pouch-anal anastomosis in patients with chronic antibiotic-dependent pouchitis and Crohn’s-like disease of the pouch. Inflamm Bowel Dis. 2023;29:932–7.
Lee KE, Shen B. Endoscopic therapy for pouch leaks and strictures: a systematic review. Dis Colon Rectum. 2022;65(S1):S92–104.
Wu XR, Kirat HT, Xhaja X, Hammel JP, Kiran RP, Church JM. The impact of mesenteric tension on pouch outcome and quality of life in patients undergoing restorative proctocolectomy. Colorectal Dis. 2014;16:986–94.
Lan N, Ashburn J, Shen B. Fecal microbiota transplantation for Clostridium difficile infection in patients with ileal pouches. Gastroenterol Rep (Oxf). 2017;5:200–7.
Levin KE, Pemberton JH, Phillips SF, Zinsmeister AR, Pezim ME. Role of oxygen free radicals in the etiology of pouchitis. Dis Colon Rectum. 1992;35:452–6.
•• Hasan B, Yim Y, Ur Rashid M, et al. Hyperbaric oxygen therapy in chronic inflammatory conditions of the pouch. Inflamm Bowel Dis. 2021;27:965–70. This is the first case series demonstrating the efficacy of hyperbaric oxygen therapy in the treatment chronic pouchitis, Crohn’s disease of the pouch, and pouch fistula. The favorable outcome also provides clue of the role tissue ischemia and tissue hypoxia in the pathogenesis of pouchitis.
Fahad H, Dulai PS, Shen B, Kochhar GS. Hyperbaric oxygen therapy is effective in the treatment of inflammatory and fistulizing pouch complications. Clin Gastroenterol Hepatol. 2021;1:1288–91.
Kienle P, Weitz J, Reinshagen S, et al. Association of decreased perfusion of the ileoanal pouch mucosa with early postoperative pouchitis and local septic complications. Arch Surg. 2001;136:1124–30.
Quinn KP, Lightner AL, Pendegraft RS, Enders FT, Boardman LA, Raffals LE. Pouchitis is a common complication in patients with familial adenomatous polyposis following ileal pouch-anal anastomosis. Clin Gastroenterol Hepatol. 2016;14:1296–301.
Abbass MA, Lavryk OA, Hyman N, Liska D, Kalady MF, Church J. Nonspecific, Acute pouchitis in patients with familial adenomatous polyposis: less common than we think. Dis Colon Rectum. 2022;65:846–50.
Church J. nuances of ileal pouch-anal anastomosis in familial adenomatous polyposis. Dis Colon Rectum. 2022;65(S1):S41-S44. 9.
Church JM. The anatomy and physiology of the ileal pouch and its relevance to pouch dysfunction [published online ahead of print, 2023 Feb 28]. Abdom Radiol (NY). 2023. https://doi.org/10.1007/s00261-022-03721-z.
Freeha K, Grace S, Nan L, Gao XH, Hull TL, Shen B. Pouch wall thickness and floppy pouch complex. Surg Endosc. 2020;34:4298–304.
Chis RS, Silverberg MS. Measurement of disease activity of pouchitis. Dis Colon Rectum. 2022;65(S1):S50–6.
Gionchetti P, Rizzello F, Venturi A, et al. Oral bacteriotherapy as maintenance treatment in patients with chronic pouchitis: a double-blind, placebo-controlled trial. Gastroenterology. 2000;119:305–9.
Gionchetti P, Rizzello F, Helwig U, et al. Prophylaxis of pouchitis onset with probiotic therapy: a double-blind, placebo-controlled trial. Gastroenterology. 2003;124(1202–1209):9.
Mimura T, Rizzello F, Helwig U, et al. Once daily high dose probiotic therapy (VSL#3) for maintaining remission in recurrent or refractory pouchitis. Gut. 2004;53:108–14.
Shen B, Brzezinski A, Fazio VW, et al. Maintenance therapy with a probiotic in antibiotic-dependent pouchitis: experience in clinical practice. Aliment Pharmacol Ther. 2005;22:721–8.
Dubinsky V, Reshef L, Bar N, et al. Predominantly antibiotic-resistant intestinal microbiome persists in patients with pouchitis who respond to antibiotic therapy. Gastroenterology. 2020;158:610–24.
Fukushima K, Saito T, Kohyama A, Watanabe K. Increased quinolone-resistant mutations of gyrA and parC genes after pouchitis treatment with ciprofloxacin. Dig Surg. 2020;37:321–30.
Shen B, Remzi FH, Lopez AR, Queener E. Rifaximin for maintenance therapy in antibiotic-dependent pouchitis. BMC Gastroenterol. 2008;8:26.
Shen B, Fazio VW, Remzi FH, et al. Combined ciprofloxacin and tinidazole therapy in the treatment of chronic refractory pouchitis. Dis Colon Rectum. 2007;50:498–508.
Abdelrazeq AS, Kelly SM, Lund JN, Leveson SH. Rifaximin-ciprofloxacin combination therapy is effective in chronic active refractory pouchitis. Colorectal Dis. 2005;7:182–6.
Shen B. Oral vancomycin in the treatment of primary sclerosing cholangitis-associated pouchitis. Gastroenterol Rep (Oxf). 2021;9:274–5.
Lupu G, Weaver KN, Herfarth HH, Barnes EL. Vancomycin is effective in the treatment of chronic inflammatory conditions of the pouch. Inflamm Bowel Dis. 2022;28:1610–3.
Scaioli E, Sartini A, Liverani E, et al. Sulfasalazine in prevention of pouchitis after proctocolectomy with ileal pouch-anal anastomosis for ulcerative colitis. Dig Dis Sci. 2017;62:1016–24.
Shen B, Fazio VW, Remzi FH, et al. Combined ciprofloxacin and tinidazole therapy in the treatment of chronic refractory pouchitis. Dis Colon Rectum. 2007;50:498–508.
Sambuelli A, Boerr L, Negreira S, et al. Budesonide enema in pouchitis–a double-blind, double-dummy, controlled trial. Aliment Pharmacol Ther. 2002;16:27–34.
Zullow S, Fazelat A, Farraye FA. Central serous chorioretinopathy in a patient with ulcerative colitis with pouchitis on budesonide-EC. Inflamm Bowel Dis. 2017;23:E19.
Haveran LA, Sehgal R, Poritz LS, McKenna KJ, Stewart DB, Koltun WA. Infliximab and/or azathioprine in the treatment of Crohn’s disease-like complications after IPAA. Dis Colon Rectum. 2011;54:15–20.
Uchino M, Ikeuchi H, Matsuoka H, et al. Topical tacrolimus therapy for antibiotic-refractory pouchitis. Dis Colon Rectum. 2013;56:1166–73.
Godoy-Brewer G, Salem G, Limketkai B, et al. Use of biologics for the treatment of inflammatory conditions of the pouch: a systematic review [published online ahead of print, 2023 Feb 8]. J Clin Gastroenterol. 2023. https://doi.org/10.1097/MCG.0000000000001828
Shehab M, Alrashed F, Charabaty A, Bessissow T. Biologic therapies for the treatment of post-ileal pouch anal anastomosis surgery chronic inflammatory disorders: systematic review and meta-analysis. J Can Assoc Gastroenterol. 2022;5:287–96.
Li Y, Lopez R, Queener E, Shen B. Adalimumab therapy in Crohn’s disease of the ileal pouch. Inflamm Bowel Dis. 2012;18:2232–9.
Kjær MD, Qvist N, Nordgaard-Lassen I, Christensen LA, Kjeldsen J. Adalimumab in the treatment of chronic pouchitis. A randomized double-blind, placebo-controlled trial. Scand J Gastroenterol. 2019;54:188–93.
Huguet M, Pereira B, Goutte M, et al. Systematic review with meta-analysis: anti-TNF therapy in refractory pouchitis and Crohn’s disease-like complications of the pouch after ileal pouch-anal anastomosis following colectomy for ulcerative colitis. Inflamm Bowel Dis. 2018;24:261–8.
Weaver KN, Gregory M, Syal G, et al. Ustekinumab is effective for the treatment of Crohn’s disease of the pouch in a multicenter cohort. Inflamm Bowel Dis. 2019;25:67–774.
Dalal RS, Gupta S, Goodrick H, Mitri J, Allegretti JR. Outcomes of standard and intensified dosing of ustekinumab for chronic pouch disorders. Inflamm Bowel Dis. 2022;28:146–9.
Rocchi C, Soliman YY, Massidda M, Vadalà di Prampero SF, Bulajic M, Sorrentino D. Is ustekinumab effective in refractory Crohn’s disease of the pouch and chronic pouchitis? A systematic review. Dig Dis Sci. 2022;67:1948–55.
Dalal RS, Bains K, Marcus J, McClure EL, Allegretti JR. Tofacitinib for the treatment of pouch-related disorders: a case series. Inflamm Bowel Dis. 2022;28:1787–9.
Akiyama S, Cohen NA, Kayal M, Dubinsky MC, Colombel JF, Rubin DT. Treatment of chronic inflammatory pouch conditions with tofacitinib: a case series from 2 tertiary ibd centers in the United States [published online ahead of print, 2023 Feb 6]. Inflamm Bowel Dis. 2023;izad011. https://doi.org/10.1093/ibd/izad011.
Uzzan M, Nachury M, Amiot A, et al. Effectiveness and safety of tofacitinib in patients with chronic pouchitis multirefractory to biologics. Dig Liver Dis. 2023;55:1158–60.
Ardalan ZS, Yao CK, Sparrow MP, Gibson PR. Review article: the impact of diet on ileoanal pouch function and on the pathogenesis of pouchitis. Aliment Pharmacol Ther. 2020;52:1323–40.
Croagh C, Shepherd SJ, Berryman M, Muir JG, Gibson PR. Pilot study on the effect of reducing dietary FODMAP intake on bowel function in patients without a colon. Inflamm Bowel Dis. 2007;13:1522–8.
Godny L, Reshef L, Pfeffer-Gik T, et al. Adherence to the Mediterranean diet is associated with decreased fecal calprotectin in patients with ulcerative colitis after pouch surgery. Eur J Nutr. 2020;59:3183–90.
Mehta M, Ahmed S, Dryden G. Refractory pouchitis improves after administration of the green tea polyphenol EGCG: a retrospective review. Int J Colorectal Dis. 2018;33:83–6.
• Karjalainen EK, Renkonen-Sinisalo L, Satokari R, et al. Fecal microbiota transplantation in chronic pouchitis: a randomized, parallel, double-blinded clinical trial. Inflamm Bowel Dis. 2021;27:1766–72. This double-blinded, randomized clinical trial demonstrated minimal efficacy of FMT in the management of chronic pouchitis. The results suggest that the manipulation of the gut microbiome in the patients with pouchitis may not alter the disease course.
Kousgaard SJ, Michaelsen TY, Nielsen HL, et al. Clinical results and microbiota changes after faecal microbiota transplantation for chronic pouchitis: a pilot study. Scand J Gastroenterol. 2020;55:421–9.
Selvig D, Piceno Y, Terdiman J, et al. Fecal microbiota transplantation in pouchitis: Clinical, endoscopic, histologic, and microbiota results from a pilot study. Dig Dis Sci. 2020;65:1099–106.
Kayal M, Lambin T, Pinotti R, Dubinsky MC, Grinspan A. A systematic review of fecal microbiota transplant for the management of pouchitis. Crohns Colitis 360. 2020;2:otaa034. Published 2020 May 12. https://doi.org/10.1093/crocol/otaa034.
Zaman S, Akingboye A, Mohamedahmed AY, et al. Faecal microbiota transplantation (FMT) in the treatment of chronic refractory pouchitis: a systematic review and meta-analysis [published online ahead of print, 2023 Jul 14]. J Crohns Colitis. 2023;jjad120. https://doi.org/10.1093/ecco-jcc/jjad120.
Nyabanga CT, Kulkarni G, Shen B. Hyperbaric oxygen therapy for chronic antibiotic-refractory ischemic pouchitis. Gastroenterol Rep (Oxf). 2017;5:320–1.
Naftali T, Bar-Lev Schleider L, Kayless H, Bromberg Z, Dotan I, Broide E. Cannabis improves clinical outcomes and quality of life in patients with chronic pouchitis. ACG Case Rep J. 2023;10:e01131. Published 2023 Aug 17.
Acknowledgements
Dr. Bo Shen is supported by the Edelman-Jarislowsky Professorship in Surgical Sciences. The author is grateful to Mr. and Mrs. Donaghy, Mr. and Mrs. Story, Mr. and Mrs. Kerr, Mr. and Mrs. Hyman, and Mr. and Mrs. Quint for their general support.
Author information
Authors and Affiliations
Contributions
This is a single-author article.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This review article does not contain any with human or animal subjects performed by the author.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shen, B. Current Management of Pouchitis. Curr Treat Options Gastro 21, 395–410 (2023). https://doi.org/10.1007/s11938-023-00438-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-023-00438-w