Opinion Statement
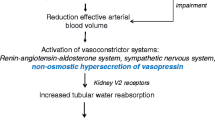
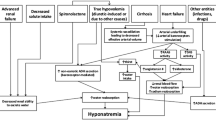
Hyponatremia may occur in patients with cirrhosis and ascites mainly due to water retention and an inability of the kidney to excrete free water. The main reason for this abnormality is related to the fact that these patients have portal hypertension and this leads to systemic vasodilation that in turn activates sodium-retaining and water-retaining systems such as the renin-angiotensin-aldosterone system and arginine vasopressin (AVP). AVP increases solute-free water retention by acting on the V2 receptors of the kidney-collecting tubes. Hyponatremia in cirrhosis is defined as a serum sodium level less than 130 meq/L. The appearance of hyponatremia in patients with advanced cirrhosis portends a poor prognosis before and after liver transplantation. Treatment of hyponatremia is difficult; fluid restriction rarely increases serum sodium levels and other therapies are associated with important drawbacks. A thorough discussion of the underlying mechanisms leading to hyponatremia and hypernatremia in cirrhosis and current treatment options including the use of vaptans (V2 receptor antagonists) are discussed in this review.


Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently have been highlighted as: • Of importance •• Of major importance
Angeli P et al. Hyponatremia in cirrhosis: results of a patient population survey. Hepatology. 2006;44(6):1535–42.
Gines P et al. Hyponatremia in cirrhosis: from pathogenesis to treatment. Hepatology. 1998;28(3):851–64.
Adrogue HJ, Madias NE. Diagnosis and treatment of hyponatremia. Am J Kidney Dis. 2014;64(5):681–4.
Gines P, Guevara M. Hyponatremia in cirrhosis: pathogenesis, clinical significance, and management. Hepatology. 2008;48(3):1002–10.
John S, Thuluvath PJ. Hyponatremia in cirrhosis: pathophysiology and management. World J Gastroenterol. 2015;21(11):3197–205.
Biggins SW et al. Serum sodium predicts mortality in patients listed for liver transplantation. Hepatology. 2005;41(1):32–9.
Gines A et al. Incidence, predictive factors, and prognosis of the hepatorenal syndrome in cirrhosis with ascites. Gastroenterology. 1993;105(1):229–36.
Sola E et al. Factors related to quality of life in patients with cirrhosis and ascites: relevance of serum sodium concentration and leg edema. J Hepatol. 2012;57(6):1199–206.
Yun BC et al. Impact of pretransplant hyponatremia on outcome following liver transplantation. Hepatology. 2009;49(5):1610–5.
Londono MC et al. Hyponatremia impairs early posttransplantation outcome in patients with cirrhosis undergoing liver transplantation. Gastroenterology. 2006;130(4):1135–43.
Heuman DM et al. Persistent ascites and low serum sodium identify patients with cirrhosis and low MELD scores who are at high risk for early death. Hepatology. 2004;40(4):802–10.
Kim WR et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359(10):1018–26.
Biggins SW et al. Evidence-based incorporation of serum sodium concentration into MELD. Gastroenterology. 2006;130(6):1652–60.
Ruf AE et al. Addition of serum sodium into the MELD score predicts waiting list mortality better than MELD alone. Liver Transpl. 2005;11(3):336–43.
Fernandez-Seara J et al. Systemic and regional hemodynamics in patients with liver cirrhosis and ascites with and without functional renal failure. Gastroenterology. 1989;97(5):1304–12.
Esteva-Font C et al. Aquaporin-1 and aquaporin-2 urinary excretion in cirrhosis: relationship with ascites and hepatorenal syndrome. Hepatology. 2006;44(6):1555–63.
Maroto A et al. Brachial and femoral artery blood flow in cirrhosis: relationship to kidney dysfunction. Hepatology. 1993;17(5):788–93.
Vallance P, Moncada S. Hyperdynamic circulation in cirrhosis: a role for nitric oxide? Lancet. 1991;337(8744):776–8.
Schrier RW. Water and sodium retention in edematous disorders: role of vasopressin and aldosterone. Am J Med. 2006;119(7 Suppl 1):S47–53.
Gines P, Cardenas A. The management of ascites and hyponatremia in cirrhosis. Semin Liver Dis. 2008;28(1):43–58.
Iwakiri Y. The molecules: mechanisms of arterial vasodilatation observed in the splanchnic and systemic circulation in portal hypertension. J Clin Gastroenterol. 2007;41 Suppl 3:S288–94.
Thibonnier M et al. Molecular pharmacology of human vasopressin receptors. Adv Exp Med Biol. 1998;449:251–76.
Kwon TH et al. Physiology and pathophysiology of renal aquaporins. Semin Nephrol. 2001;21(3):231–8.
Nielsen S et al. Aquaporins in the kidney: from molecules to medicine. Physiol Rev. 2002;82(1):205–44.
Sterns RH, Riggs JE, Schochet Jr SS. Osmotic demyelination syndrome following correction of hyponatremia. N Engl J Med. 1986;314(24):1535–42.
Tanneau RS et al. High incidence of neurologic complications following rapid correction of severe hyponatremia in polydipsic patients. J Clin Psychiatry. 1994;55(8):349–54.
Guevara M et al. Hyponatremia is a risk factor of hepatic encephalopathy in patients with cirrhosis: a prospective study with time-dependent analysis. Am J Gastroenterol. 2009;104(6):1382–9.
Riggio O et al. Incidence, natural history, and risk factors of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stent grafts. Am J Gastroenterol. 2008;103(11):2738–46.
Guevara M et al. Risk factors for hepatic encephalopathy in patients with cirrhosis and refractory ascites: relevance of serum sodium concentration. Liver Int. 2010;30(8):1137–42.
Schwabl P et al. Risk factors for development of spontaneous bacterial peritonitis and subsequent mortality in cirrhotic patients with ascites. Liver Int. 2015;35(9):2121–8. Retrospective cohort study demonstrating that hyponatremia along with Child-Pugh stage C and elevated ascites represent predictive factors for SBP development and higher mortality in patients with liver cirrhosis.
Rimola A et al. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. Int Ascites Club J Hepatol. 2000;32(1):142–53.
Arvaniti V et al. Infections in patients with cirrhosis increase mortality four-fold and should be used in determining prognosis. Gastroenterology. 2010;139(4):1246–56. 1256.e1–5.
European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53(3): 397–417.
Cordoba J, Blei AT. Brain edema and hepatic encephalopathy. Semin Liver Dis. 1996;16(3):271–80.
Blei AT, Larsen FS. Pathophysiology of cerebral edema in fulminant hepatic failure. J Hepatol. 1999;31(4):771–6.
Haussinger D et al. Hepatic encephalopathy in chronic liver disease: a clinical manifestation of astrocyte swelling and low-grade cerebral edema? J Hepatol. 2000;32(6):1035–8.
Butterworth RF. Pathogenesis of hepatic encephalopathy: new insights from neuroimaging and molecular studies. J Hepatol. 2003;39(2):278–85.
Videen JS et al. Human cerebral osmolytes during chronic hyponatremia. A proton magnetic resonance spectroscopy study. J Clin Invest. 1995;95(2):788–93.
Soupart A et al. Rapid (24-hour) reaccumulation of brain organic osmolytes (particularly myo-inositol) in azotemic rats after correction of chronic hyponatremia. J Am Soc Nephrol. 2002;13(6):1433–41.
Laubenberger J et al. Proton magnetic resonance spectroscopy of the brain in symptomatic and asymptomatic patients with liver cirrhosis. Gastroenterology. 1997;112(5):1610–6.
Restuccia T et al. Effects of dilutional hyponatremia on brain organic osmolytes and water content in patients with cirrhosis. Hepatology. 2004;39(6):1613–22.
Furst H et al. The urine/plasma electrolyte ratio: a predictive guide to water restriction. Am J Med Sci. 2000;319(4):240–4.
McCormick PA et al. Intravenous albumin infusion is an effective therapy for hyponatraemia in cirrhotic patients with ascites. Gut. 1990;31(2):204–7.
Abbasoglu O et al. Liver transplantation in hyponatremic patients with emphasis on central pontine myelinolysis. Clin Transpl. 1998;12(3):263–9.
Decaux G, Soupart A, Vassart G. Non-peptide arginine-vasopressin antagonists: the vaptans. Lancet. 2008;371(9624):1624–32.
Wong F et al. A vasopressin receptor antagonist (VPA-985) improves serum sodium concentration in patients with hyponatremia: a multicenter, randomized, placebo-controlled trial. Hepatology. 2003;37(1):182–91.
Gerbes AL et al. Therapy of hyponatremia in cirrhosis with a vasopressin receptor antagonist: a randomized double-blind multicenter trial. Gastroenterology. 2003;124(4):933–9.
Schrier RW et al. Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N Engl J Med. 2006;355(20):2099–112.
Gines P et al. Effects of satavaptan, a selective vasopressin V(2) receptor antagonist, on ascites and serum sodium in cirrhosis with hyponatremia: a randomized trial. Hepatology. 2008;48(1):204–13.
Cardenas A et al. Tolvaptan, an oral vasopressin antagonist, in the treatment of hyponatremia in cirrhosis. J Hepatol. 2012;56(3):571–8. Sub-analysis of the Study of Ascending Levels of Tolvaptan trials, comparing tolvaptan treatment against placebo exclusively in cirrhotic patients with hyponatremia. The results demonstrated that tolvaptan in addition to standard therapy, effectively raises and maintains serum sodium concentrations and improves health-related quality of life.
O’Leary JG, Davis GL. Conivaptan increases serum sodium in hyponatremic patients with end-stage liver disease. Liver Transpl. 2009;15(10):1325–9.
Torres VE, Chapman AB, Devuyst O, et al. Tolvaptan in patients with autosomal dominant polycystic kidney disease. N Engl J Med. 2012;367:2407–18.
Samsca (Tolvaptan): Drug safety communication—FDA limits duration and usage due to possible liver injury leading to organ transplant or death. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm350185.htm.
Cárdenas A, Riggio O. Correction of hyponatraemia in cirrhosis: treating more than a number! J Hepatol. 2015;62(1):13–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Blanca Lizaola declares that she has no conflict of interest. Alan Bonder declares that he has no conflict of interest. Elliot B. Tapper declares that he has no conflict of interest. Angela Mendez-Bocanegra declares that she has no conflict of interest. Andres Cardenas declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Liver
Rights and permissions
About this article
Cite this article
Lizaola, B., Bonder, A., Tapper, E.B. et al. The Changing Role of Sodium Management in Cirrhosis. Curr Treat Options Gastro 14, 274–284 (2016). https://doi.org/10.1007/s11938-016-0094-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-016-0094-y