Abstract
Purpose of Review
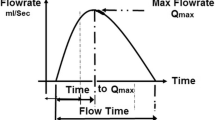
Uroflowmetry is widely used for initial non-invasive evaluation of lower urinary tract disorders. Current clinical use is mostly restricted to a scrutiny of the maximum flow rate and uroflow pattern recorded by a conventional flowmeter in a health care facility. There are several advancements in our understanding and in available technologies that promise to transform clinical utilization of this simple test.
Recent Findings
Several aspects of the uroflow test in addition to maximum flow rate and uroflow pattern show potential diagnostic utility. This includes flow acceleration, uroflow indices, uroflow-electromyography including lag time, stop uroflow test, and uroflow-based nomograms. There are initial attempts to use artificial intelligence in analysis. There is also new data with regard to factors influencing variability of uroflow testing that might influence the diagnostic value in as yet uncertain ways including diurnal variability, postural variability, locational variability, and operator variability. There are new technologies for uroflow testing in a home environment allowing for easy repetition. However, there are several challenges owing to a paucity of clinical data and standardization. There are also critical lacunae in terminology that need to be addressed.
Summary
There are exciting new advancements in the field of uroflowmetry. However, there is need to standardize and validate the newer uroflow tracing analyses and technologies.



Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
de Wachter S, Abranches-Monteiro L, Gammie A, Hashim H, Nitti V, Rosier P, Sinha S, Tarcan T, Toozs-Hobson P, Wen JG. Urodynamic testing. In: Cardozo L, Rovner E, Wagg A, Wein A, Abrams P, editors. Incontinence. 7th ed. Bristol, UK: ICUD ICS; 2023. p. 487–550.
Lerner LB, McVary KT, Barry MJ, Bixler BR, Dahm P, Das AK, et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA Guideline Part I-Initial work-up and medical management. J Urol. 2021;206(4):806–17.
Harding CK, Lapitan MC, Arlandis S, Bo K, Costantini E, Groen J, Nambiar AK, Omar MI, Phe V. Non-neurogenic female LUTS. European Association of Urology Guidelines. 2023 [cited 2023 Jan 5]. Available from https://uroweb.org/guideline/non-neurogenic-female-luts.
Cornu JN, Gacci M, Hashim H, Herrmann TRW, Malde S, Netsch C, Rieken M, Sakalis V, Tutolo M. Non-neurogenic male LUTS. European Association of Urology Guidelines. 2023 [cited 2023 Jun 12]. Available from https://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts/.
Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002;21(3):261–74.
•• Young GJ, Metcalfe C, Lane JA, Lewis AL, Abrams P, Blair PS, et al. Prostate surgery for men with lower urinary tract symptoms: Do we need urodynamics to find the right candidates? Exploratory findings from the UPSTREAM trial. Eur Urol Focus. 2022;8(5):1331–9. Secondary analysis of a large randomized trial comparing the outcome of prostate surgery in men offered routine care versus urodynamics-based evaluation. This analysis showed that regardless of evaluation pathway, uroflow was an important predictor of outcome.
Van Batavia JP, Combs AJ. Non-invasive testing and its role in diagnosis and management of children with voiding dysfunction. Curr Bladder Dysfunct Rep. 2018;13(2):56–65.
• Ben Muvhar R, Wagmaister J, Mekayten M. Navigating the diagnostic maze: unraveling the non-invasive evaluation of bladder outlet obstruction in men—A comprehensive systematic review. Curr Bladder Dysfunct Rep. 2023;18(4):318–32. Systematic review of all non-invasive evaluation for assessing bladder outlet obstruction in men including uroflowmetry with comments on flow rate, flow pattern and volume correction.
Ito H, Sakamaki K, Young GJ, Blair PS, Hashim H, Lane JA, et al. Predicting prostate surgery outcomes from standard clinical assessments of lower urinary tract symptoms to derive prognostic symptom and flowmetry criteria. Eur Urol Focus. 2023;S2405–4569(23):00154–62.
Escobar C, Brucker B. Urodynamics for the “failed” midurethral sling. Curr Bladder Dysfunct Rep. 2020;15(4):245–58.
Sinha S, Agarwal MM, Vasudeva P, Khattar N, Madduri VKS, Yande S, et al. The urological Society of India Guidelines for the evaluation and management of nonneurogenic urinary incontinence in adults (executive summary). Indian J Urol. 2019;35(3):185–8.
•• Tarcan T, Acar O, Agarwal MM, Rubilotta E, De Nunzio C, Rosier P. ICS educational module: The practice of uroflowmetry in adults. Continence. 2024;9:101065. An educational module from the International Continence Society on uroflowmetry with comments on technique, quality check, interpretation, and reporting based on a systematic review and expert consensus.
Bauer SB, Nijman RJM, Drzewiecki BA, Sillen U, Hoebeke P, International Children’s Continence Society Standardization Subcommittee. International Children’s Continence Society standardization report on urodynamic studies of the lower urinary tract in children. Neurourol Urodyn. 2015;34(7):640–7.
ICS Glossary [Internet]. ICS. [cited 2022 Sep 26]. Available from https://www.ics.org/glossary.
Wada N, Watanabe M, Ishikawa M, Takeuchi K, Miyauchi K, Abe N, et al. Uroflowmetry pattern in detrusor underactivity and bladder outlet obstruction in male patients with lower urinary tract symptoms. Low Urin Tract Symptoms. 2021;13(3):361–5.
Netto JMB, Hittelman A, Lambert S, Murphy K, Collette-Gardere T, Franco I. Interpretation of uroflow curves: A global survey measuring inter and intra rater reliability. Neurourol Urodyn. 2020;39(2):826–32.
Martonosi ÁR, Pázmány P, Kiss S, Földi M, Zsákai A, Szabó L. Urine flow acceleration in healthy children: A retrospective cohort study. Neurourol Urodyn. 2023;42(2):463–71.
Karasu AFG, Aydın S, Kalkan S, Ersoz C. Association of intrinsic sphincter deficiency with urine flow acceleration measurement. Low Urin Tract Symptoms. 2021;13(1):154–9.
Futyma K, Nowakowski Ł, Bogusiewicz M, Ziętek A, Wieczorek AP, Rechberger T. Use of uroflow parameters in diagnosing an overactive bladder-back to the drawing board. Neurourol Urodyn. 2017;36(1):198–202.
Franco I, Franco J, Lee YS, Choi EK, Han SW. Can a quantitative means be used to predict flow patterns: Agreement between visual inspection vs flow index derived flow patterns. J Pediatr Urol. 2016;12(4):218.e1–8.
Ha JS, Lee YS, Han SW, Kim SW. The relationship among flow index, uroflowmetry curve shape, and EMG lag time in children. Neurourol Urodyn. 2020;39(5):1387–93.
• Van Batavia JP, Pohl HG, Farhat WA, Chiang G, BaniHani A, Collett-Gardere T, et al. Is it time to reconsider how we document pediatric uroflow studies?: A study from the SPU Voiding Dysfunction task force. J Pediatr Urol. 2023;19(5):546–54. Study from the Society of Pediatric Urology Voiding Dysfunction task force showing the limitations of using flow pattern.
Sinha S. Dysfunctional voiding: a review of the terminology, presentation, evaluation and management in children and adults. Indian J Urol. 2011;27(4):437–47.
Sharifi-Rad L, Ladi-Seyedian S-S, Amirzargar H, Kajbafzadeh A-M. Pelvic floor electromyography and urine flow patterns in children with vesicoureteral reflux and lower urinary tract symptoms. Int Braz J Urol. 2018;44(6):1207–14.
Rosier PFWM, Gammie A, Valdevenito JP, Speich J, Smith P, Sinha S, et al. ICS-SUFU standard: Theory, terms, and recommendations for pressure-flow studies performance, analysis, and reporting. Part 2: Analysis of PFS, reporting, and diagnosis. Neurourol Urodyn. 2023. https://doi.org/10.1002/nau.25187.
El-Hakim A, Al-Hathal N, Al-Qaoud T, Gagné G, Larocque S, Denis R, et al. Novel uroflow stop test at time of catheter removal is a strong predictor of early urinary continence recovery following robotic-assisted radical prostatectomy: A pilot study. Neurourol Urodyn. 2015;34(1):60–4.
Alenizi AM, Bienz M, Rajih E, Alesawi A, Al-Hathal N, Benayoun S, et al. Uroflow stop test and potency recovery: A surrogate for pelvic floor integrity post robotic-assisted radical prostatectomy? Urology. 2015;86(4):766–71.
Boni A, Gervasoni F, Lomauro A, Del Zingaro M, Maiolino G, Galletti C, et al. Urologic latency time during uroflow stop test with electromyography: An incontinence detector in rehabilitation after robotic radical prostatectomy. Eur J Phys Rehabil Med. 2023;59(1):94–102.
Shinohara M, Torimoto K, Matsushita C, Gotoh D, Yoshida H, Saka T, et al. A new nomogram of urinary flow rate and volume based on multiple measurements per healthy adult Japanese men using a portable uroflowmeter (P-Flowdiary®). BMC Urol. 2022;22(1):130.
Szmydki D, Burzynski B, Soltysiak-Gibala Z, Przymuszala P, Trzewik M, Chudek J, et al. Prediction of detrusor underactivity based on non-invasive functional tests and clinical data in patients with symptoms of bladder outlet obstruction. Eur Rev Med Pharmacol Sci. 2020;24(21):10992–8.
Matsukawa Y, Kameya Y, Takahashi T, Shimazu A, Ishida S, Yamada M, et al. Characteristics of uroflowmetry patterns in men with detrusor underactivity revealed by artificial intelligence. Int J Urol. 2023;30(10):907–12.
Spyropoulos E, Galanakis I, Deligiannis D, Spyropoulou A, Kotsiris D, Panagopoulos A, et al. Flow resistive forces index (QRF): Development and clinical applicability assessment of a novel measure of bladder outlet resistance, aiming to enhance the diagnostic performance of uroflowmetry. Low Urin Tract Symptoms. 2020;12(3):190–7.
Yoshiyama A, Tsujimura A, Hiramatsu I, Morino J, Anno Y, Kurosawa M, et al. Circadian rhythm of voided volume, maximum flow rate, and voiding time evaluated by toilet uroflowmetry in hospitalized women with nocturia. Urology. 2023;179:50–7.
Hiramatsu I, Tsujimura A, Miyoshi M, Ogasa T, Miyoshi Y, Ishikawa K, et al. Maximum flow rate is lowest in the early morning in hospitalized men with nocturia evaluated over 24 hours by toilet uroflowmetry. Urology. 2022;166:196–201.
Kato S, Watanabe H, Yamasue K. Freeflow: The novel portable uroflowmeter can help to realize practical urinary conditions at home. Low Urin Tract Symptoms. 2022;14(3):208–13.
•• Lee HJ, Aslim EJ, Balamurali BT, Ng LYS, Kuo TLC, Lin CMY, et al. Development and validation of a deep learning system for sound-based prediction of urinary flow. Eur Urol Focus. 2023;9(1):209–15. Study of audio analysis of the uroflow pattern with use of machine deep learning to develop a smartphone-based test that can identify abnormal and normal flow based on audioflow analysis.
Pandolfo SD, Crauso F, Aveta A, Cilio S, Barone B, Napolitano L, et al. A novel low-cost uroflowmetry for patient telemonitoring. Int J Environ Res Public Health. 2023;20(4):3287.
Gallo GA, Cabral Dias Filho A, Cruz PR, Moraes CF. Development and construction of an open-platform, open-source low-cost portable uroflowmeter: The OpenFlow device. Neurourol Urodyn. 2024;43(1):153–60.
Rosier PFWM, Valdevenito JP, Smith P, Sinha S, Speich J, Gammie A. ICS-SUFU standard: Theory, terms, and recommendations for pressure-flow studies performance, analysis, and reporting, Part 1: Background theory and practice. Continence. 2023;100710. https://doi.org/10.1016/j.cont.2023.100710.
Bladt L, Kashtiara A, Platteau W, De Wachter S, De Win G. First-year experience of managing urology patients with home uroflowmetry: Descriptive retrospective analysis. JMIR Form Res. 2023;7:e51019.
Long Depaquit T, Michel F, Gaillet S, Savoie P-H, Karsenty G. Home uroflowmetry technics and clinical relevance: A narrative review. Prog Urol. 2022;32(17):1531–42.
Namiri NK, Cheema B, Lui H, Enriquez A, Rios N, Srirangapatanam S, et al. Characterizing voiding experiences of men choosing seated and standing positions. Neurourol Urodyn. 2020;39(8):2509–19.
Alrabadi A, Al Demour S, Mansi H, AlHamss S, Al OL. Evaluation of voiding position on uroflowmetry parameters and post void residual urine in patients with benign prostatic hyperplasia and healthy men. Am J Mens Health. 2020;14(4):1557988320938969.
Dönmez Mİ, Özkent MS, Hamarat MB, Kocalar M. Through the zipper or pants down: Does it change uroflowmetry parameters in healthy males? Low Urin Tract Symptoms. 2022;14(5):341–5.
Dogan S. Comparison of self-conducted and assistant-supervised uroflowmetry methods. Cureus. 2022;14(2):e22030.
Jin J, Chung Y, Kim W, Heo Y, Jeon J, Hoh J, et al. Classification of bladder emptying patterns by LSTM neural network trained using acoustic signatures. Sensors (Basel). 2021;21(16):5328.
Schultz RE. Smartphone app for in-home uroflowmetry. Urol Pract. 2022;9(6):524–30.
Qi Y, Kong H, Kim Y. Estimation of urine flow velocity using millimeter-wave FMCW radar. Sensors (Basel). 2022;22(23):9402.
Han JH, Lee JH, Jun J, Park MU, Lee JS, Park S, et al. Validity and reliability of a home-based, guardian-conducted video voiding test for voiding evaluation after hypospadias surgery. Investig Clin Urol. 2020;61(4):425–31.
Rogel R, Lorenzo L, Avargues A, Lujan S, Broseta E, Arlandis S. ANalogical UroFlowmetry (ANUF): Correspondence between this new visual pictogram and uroflowmetry in men with lower urinary tract symptoms: A new approach for the study of male micturition dynamics. Urology. 2020;146:236–41.
Funding
No funding for this work.
Author information
Authors and Affiliations
Contributions
SS: All aspects of this work.
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Images are from author’s archive and have not been used in prior publication.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sinha, S. The Use of Uroflowmetry as a Diagnostic Test. Curr Urol Rep 25, 99–107 (2024). https://doi.org/10.1007/s11934-024-01200-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-024-01200-0