Abstract
Purpose of Review
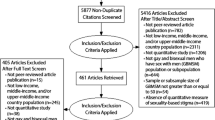
The purpose of the current review is to provide a summary of the recent research published on the relationships between intersectional stigma and sexual minority women’s experiences of sexual health. Given the emerging stage of this body of work, we employed a narrative review to both elicit this summary as well as identify gaps in the current work.
Recent Findings
We found that intersectional stigma affects sexual and gender minority women’s sexual health across multiple domains of health, including intersectional social determinants of health, sexual healthcare experiences and barriers to care, STI/HIV testing and prevention, cancer screening, and sexual violence. We also found that intersectional research remains the minority of sexual health research currently produced and that sexual health researchers operationalize intersectionality and intersectional research design in varied ways.
Summary
Intersectionality remains a critical framework for eliciting more representative sexual health data among multiply minoritized populations among sexual and gender minority women.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bowleg L. The Problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–73.
Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–98.
Bowleg L, Bauer G. Invited reflection: quantifying intersectionality. Psychol Women Q. 2016;40(3):337–41.
Else-Quest NM, Hyde JS. Intersectionality in quantitative psychological research: II. methods and Techniques. Psychol Women Q. 2016;40(3):319–36.
Bauer GR, Scheim AI. Methods for analytic intercategorical intersectionality in quantitative research: discrimination as a mediator of health inequalities. Soc Sci Med. 2019;1(226):236–45. Publication provides an overview of quantitative intersectional research design.
Crenshaw K. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ Chic Leg Forum. 1989;8(1):31.
Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanf Law Rev. 1991;43(6):1241–99.
Collins PH. Black feminist thought: knowledge, consciousness, and the politics of empowerment. Hyman 1990;p 384
The Combahee River Collective Statement [Internet]. Library of Congress, Washington, D.C. 20540 USA. [cited 2022 Jun 9]. Available from https://www.loc.gov/item/lcwaN0028151/
Purdie-Vaughns V, Eibach RP. Intersectional invisibility: the distinctive advantages and disadvantages of multiple subordinate-group identities. Sex Roles. 2008;59(5):377–91.
Keuchenius A, Mügge L. Intersectionality on the go: The diffusion of Black feminist knowledge across disciplinary and geographical borders. Br J Sociol. 2021;72(2):360–78.
Szymanski DM. Heterosexism and sexism as correlates of psychological distress in lesbians. J Couns Dev. 2005;83(3):355–60.
Ghabrial MA. “Trying to figure out where we belong”: narratives of racialized sexual minorities on community, identity, discrimination, and health. Sex Res Soc Policy. 2017;14(1):42–55.
Herek GM. Sexual stigma and sexual prejudice in the United States: a conceptual framework. In: Contemporary perspectives on lesbian, gay, and bisexual identities. New York, NY, US: Springer Science + Business Media; 2009. p 65–111. (Nebraska Symposium on Motivation).
Major B, Dovidio JF, Link BG. The Oxford handbook of stigma, discrimination, and health [Internet]. The Oxford Handbook of Stigma, Discrimination, and Health. Oxford University Press; 2018 [cited 2022 May 19]. Available from https://www.oxfordhandbooks.com/view/10.1093/oxfordhb/9780190243470.001.0001/oxfordhb-9780190243470
Sovacool BK, Axsen J, Sorrell S. Promoting novelty, rigor, and style in energy social science: towards codes of practice for appropriate methods and research design. Energy Res Soc Sci. 2018;1(45):12–42.
James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The report of the 2015 U.S. Transgender Survey. Washington (DC): National Center for Transgender Equality. 2016.
Gattamorta KA, Salerno JP, Castro AJ. Intersectionality and health behaviors among US high school students: examining race/ethnicity, sexual identity, and sex. J Sch Health. 2019;89(10):800–8.
Santos CA, Williams EC, Rodriguez J, Ornelas IJ. Sexual health in a social and cultural context: a qualitative study of young Latina lesbian, bisexual, and queer women. J Racial Ethn Health Disparities. 2017;4(6):1206–13.
Turner CM, Ahern J, Santos GM, Arayasirikul S, Wilson EC. Parent/caregiver responses to gender identity associated with HIV-related sexual risk behavior among young trans women in San Francisco. J Adolesc Health. 2019;65(4):491–7.
Wilson EC, Dhakal M, Sharma S, Rai A, Lama R, Chettri S, et al. Population-based HIV prevalence, stigma and HIV risk among trans women in Nepal. BMC Infect Dis. 2021;21(1):128.
Gessner M, Bishop MD, Martos A, Wilson BDM, Russell ST. Sexual minority people’s perspectives of sexual health care: understanding minority stress in sexual health settings. Sex Res Social Policy. 2020;17(4):607–18.
Ejaife OL, Ho IK. Healthcare experiences of a Black lesbian in the United States. J Health Psychol. 2019;24(1):52–64.
Agénor M, Pérez AE, Wihoit A, Almeda F, Charlton BM, Evans ML, Borrero S, Austin B. Contraceptive care disparities among sexual orientation identity and racial/ethnic subgroups of U.S. women: a national probability sample study. J Women’s Health. 2021;30(10):1406–15.
Cerezo A, Ching S, Ramirez A. Healthcare access and health-related cultural norms in a community sample of black and Latinx sexual minority gender expansive women. J Homosex. 2021;29:1–24. Publication provides an in-depth qualitative analysis of how intersectional identity and discrimination affect Black and Latinx women’s interactions with sexual healthcare services.
Bastos JL, Harnois CE, Paradies YC. Health care barriers, racism, and intersectionality in Australia. Soc Sci Med. 2018;199:209–18.
McNulty MC, Acree ME, Kerman J, Williams HHS, Schneider JA. Shared decision making for HIV pre-exposure prophylaxis (PrEP) with black transgender women. Cult Health Sex. 2021;13:1–20.
Logie CH, Lys CL, Dias L, Schott N, Zouboules MR, MacNeill N, et al. “Automatic assumption of your gender, sexuality and sexual practices is also discrimination”: Exploring sexual healthcare experiences and recommendations among sexually and gender diverse persons in Arctic Canada. Health Soc Care Community. 2019;27(5):1204–13.
Grant R, Nash M, Hansen E. What does inclusive sexual and reproductive healthcare look like for bisexual, pansexual and queer women? Findings from an exploratory study from Tasmania, Australia. Cult Health Sex. 2020;22(3):247–60.
Agénor M, Pérez AE, Koma JW, Abrams JA, McGregor AJ, Ojikutu BO. Sexual orientation identity, race/ethnicity, and lifetime HIV testing in a national probability sample of U.S. Women and Men: An Intersectional Approach. LGBT Health. 2019;6(6):306–18. Publication provides an example of a population-level intersectional design highlighting HIV testing access across intersectional identity.
Logie CH, Gibson MF. A mark that is no mark? Queer women and violence in HIV discourse. Cult Health Sex. 2013;15(1):29–43.
Harvey TD, Opara I, Wang EA. Role of the intersections of gender, race and sexual orientation in the association between substance use behaviors and sexually transmitted infections in a national sample of adults with recent criminal legal involvement. Int J Environ Res Public Health. 2022;19(7):4100.
Abubakari GM, Dada D, Nur J, Turner D, Otchere A, Tanis L, et al. Intersectional stigma and its impact on HIV prevention and care among MSM and WSW in sub-Saharan African countries: a protocol for a scoping review. BMJ Open. 2021;11(8):e047280.
Agénor M, Pérez A, Peitzmeier SM, Potter J, Borrero S. Human papillomavirus vaccination initiation among sexual orientation identity and racial/ethnic subgroups of Black and White U.S. women and girls: an intersectional analysis. J Womens Health. 2018;27(11):1349–58.
Zubizarreta D, Beccia AL, Trinh MH, Reynolds CA, Reisner SL, Charlton BM. Human papillomavirus vaccination disparities among U.S. college students: an intersectional Multilevel Analysis of Individual Heterogeneity and Discriminatory Accuracy (MAIHDA). Soc Sci Med. 2022;301:114871.
Dean LT, Greene N, Adams MA, Geffen SR, Malone J, Tredway K, et al. Beyond Black and White: race and sexual identity as contributors to healthcare system distrust after breast cancer screening among US women. Psychooncology. 2021;30(7):1145–50.
Poteat TC, Adams MA, Malone J, Geffen S, Greene N, Nodzenski M, et al. Delays in breast cancer care by race and sexual orientation: results from a national survey with diverse women in the United States. Cancer. 2021;127(19):3514–22.
Chen J, Walters ML, Gilbert LK, Patel N. Sexual violence, stalking, and intimate partner violence by sexual orientation, United States. Psychol Violence. 2020;10(1):110–9.
Canan SN, Jozkowski KN, Wiersma-Mosley JD, Bradley M, Blunt-Vinti H. Differences in lesbian, bisexual, and heterosexual women’s experiences of sexual assault and rape in a national U.S. sample. J Interpers Violence. 2021;36(19–20):9100–20.
Whitfield DL, Coulter RWS, Langenderfer-Magruder L, Jacobson D. Experiences of intimate partner violence among lesbian, gay, bisexual, and transgender college students: the intersection of gender, race, and sexual orientation. J Interpers Violence. 2021;36(11–12):NP6040–64.
Flanders CE, VanKim N, Anderson RE, Tarasoff LA. Exploring potential determinants of sexual victimization disparities among young sexual minoritized people: a mixed-method study. Psychology of Sexual Orientation and Gender Diversity [Internet]. 2021 Sep 2 [cited 2021 Sep 22]; Available from http://proxy.mtholyoke.edu:2048/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=pdh&AN=2021-81526-001&site=eds-live&scope=site
Gilmore AK, Walsh K, López C, Fortson K, Oesterle DW, Salamanca NK, et al. Sexual assault victimization: Latinx identity as a protective factor for sexual minorities. J Interpers Violence. 2021;10:0886260521999122.
Hawkey AJ, Ussher JM, Liamputtong P, Marjadi B, Sekar JA, Perz J, et al. Trans women’s responses to sexual violence: vigilance, resilience, and need for support. Arch Sex Behav. 2021;50(7):3201–22.
Sanger N, Lynch I. ‘You have to bow right here’: heteronormative scripts and intimate partner violence in women’s same-sex relationships. Cult Health Sex. 2018;20(2):201–17.
Tam MW. Queering reproductive access: reproductive justice in assisted reproductive technologies. Reprod Health. 2021;18(1):164.
Bilge S. The fungibility of intersectionality: an Afropessimist reading. Ethn Racial Stud. 2020;43(13):2298–326.
Bilge S. Intersectionality undone: saving intersectionality from feminist intersectionality studies 1. Du Bois Review: Social Science Research on Race. 2013 ed;10(2):405–24.
Balsam KF, Molina Y, Beadnell B, Simoni J, Walters K. Measuring multiple minority stress: the LGBT people of color microaggressions scale. Cultur Divers Ethnic Minor Psychol. 2011;17(2):163–74.
Scheim AI, Bauer GR. The intersectional discrimination index: development and validation of measures of self-reported enacted and anticipated discrimination for intercategorical analysis. Soc Sci Med. 2019;1(226):225–35.
Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389(10072):941–50.
Sexual and Gender Minority Research Office. Bisexual health research workshop: identifying research opportunities in bisexual health research [Internet]. National Intitutes of Health. Available from https://dpcpsi.nih.gov/sites/default/files/Summary_BisexualHealthResearchWorkshopv2_508.pdf
Brenick A, Romano K, Kegler C, Eaton LA. Understanding the influence of stigma and medical mistrust on engagement in routine healthcare among Black women who have sex with women. LGBT Health. 2017;4(1):4–10.
Greene MZ, Hughes TL, Hanlon A, Huang, L, Sommers, MS, Meghani SH. Predicting cervical cancer screening among sexual minority women using classification and regression tree analysis. Preventative Medicine Reports. 2019;13:153–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Female Sexual Dysfunction and Disorders.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Flanders, C.E., Khandpur, S. & Fitzgerald, R. Intersectional Stigma and Sexual Health Among Sexual and Gender Minority Women. Curr Sex Health Rep 14, 190–199 (2022). https://doi.org/10.1007/s11930-022-00338-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11930-022-00338-7