Abstract
Purpose of Review
To describe recent advances in infection prevention strategies for penile prosthesis surgery.
Recent Findings
Improvements in surgical technique, antibiotic prophylaxis, prosthetic device design, and patient selection have globally reduced penile prosthesis infection rates. However, current societal antibiotic prophylaxis guidelines may fail to cover all organisms implicated in penile prosthesis infections, particularly fungal and anaerobic pathogens.
Summary
Although significant strides have been made in reducing penile prosthesis infections, further education and research efforts are needed to continue to prevent this infrequent, but devastating complication. This review discusses recent advances in penile infection understanding and prevention.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151(1):54–61.
Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol. 2010;57(5):804–14.
Montague DK, Jarow JP, Broderick GA, Dmochowski RR, Heaton JP, Lue TF, et al. Chapter 1: The management of erectile dysfunction: an AUA update. J Urol. 2005;174(1):230–9.
Ji YS, Ko YH, Song PH, Moon KH. Long-term survival and patient satisfaction with inflatable penile prosthesis for the treatment of erectile dysfunction. Korean J Urol. 2015;56(6):461–5.
Vitarelli A, Divenuto L, Fortunato F, et al. Long term patient satisfaction and quality of life with AMS700CX inflatable penile prosthesis. Arch Ital Urol Androl. 2013;85(3):133–7.
Selph JP, Carson CC 3rd. Penile prosthesis infection: approaches to prevention and treatment. Urol Clin North Am. 2011;38(2):227–35.
O’Rourke TK Jr, Erbella A, Zhang Y, Wosnitzer MS. Prevention, identification, and management of post-operative penile implant complications of infection, hematoma, and device malfunction. Transl Androl Urol. 2017:S832–48.
Henry GD, Donatucci CF, Conners W, Greenfield JM, Carson CC, Wilson SK, et al. An Outcomes Analysis of over 200 Revision Surgeries for Penile Prosthesis Implantation: A Multicenter Study. J Sex Med. 2012;9(1):309–15.
Wilson SK, Costerton JW. Biofilm and penile prosthesis infections in the era of coated implants: a review. J Sex Med. 2012;9(1):44–53.
Chason J, Sausville J, Kramer AC. Penile prosthesis implantation compares favorably in malpractice outcomes to other common urological procedures: findings from a malpractice insurance database. J Sex Med. 2009;6(8):2111–4.
Pederzoli F, Chappidi MR, Collica S, Kates M, Joice GA, Sopko NA, et al. Analysis of Hospital Readmissions After Prosthetic Urologic Surgery in the United States: Nationally Representative Estimates of Causes, Costs, and Predictive Factors. J Sex Med. 2017;14(8):1059–65.
Goetz A, Yu VL, O'Donnell WF. Surgical complications related to insertion of penile prostheses with emphasis on infection and cost. Infect Control Hosp Epidemiol. 1988;9(6):250–4.
Habous M, Tal R, Tealab A, Aziz M, Sherif H, Mahmoud S, et al. Predictors of Satisfaction in Men After Penile Implant Surgery. J Sex Med. 2018;15(8):1180–6.
Swanton AR, Munarriz RM, Gross MS. Updates in penile prosthesis infections. Asian J Androl. 2019. https://doi.org/10.4103/aja.aja_84_19
Krzastek SC, Smith R. An update on the best approaches to prevent complications in penile prosthesis recipients. Ther Adv Urol. 2019;11:1756287218818076–6.
Carson CC, Robertson CN. Late hematogenous infection of penile prostheses. J Urol. 1988;139(1):50–2.
Welliver RC Jr, Hanerhoff BL, Henry GD, Kohler TS. Significance of biofilm for the prosthetic surgeon. Curr Urol Rep. 2014;15(6):411.
Donlan RM. Biofilm Formation: A Clinically Relevant Microbiological Process. Clin Infect Dis. 2001;33(8):1387–92.
Stewart PS, Costerton JW. Antibiotic resistance of bacteria in biofilms. Lancet. 2001;358(9276):135–8.
Elmussareh M, Goddard JC, Summerton DJ, Terry TR. Minimising the risk of device infection in penile prosthetic surgery: a UK perspective. J Clin Urol. 2013;6(5):280–8.
Henry GD, Wilson SK, Delk JR 2nd, et al. Revision washout decreases penile prosthesis infection in revision surgery: a multicenter study. J Urol. 2005;173(1):89–92.
Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 2002;15(2):167–93.
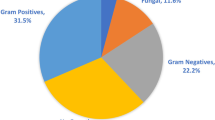
•• Gross MS, Phillips EA, Carrasquillo RJ, et al. Multicenter Investigation of the Micro-Organisms Involved in Penile Prosthesis Infection: An Analysis of the Efficacy of the AUA and EAU Guidelines for Penile Prosthesis Prophylaxis. J Sex Med. 2017;14(3):455–63. Multicenter retrospective study to investigate penile prosthesis infection microbiology to consider with changes in practice could decrease infection rate, to evaluate current antibiotic prophylaxis guidelines, and to develop a proposed algorithm for penile prosthesis infections. This study showed a high incidence of anaerobic, Candida, and MRSA infections. Approximately 1/3 on infected prosthesis cases had negative cultures. Microorganisms identified in this study were not covered by the EUA and AUA antibiotic guidelines in at least 14% to 38% of cases. These findings suggest broadening antibiotic prophylaxis guidelines and creating a management now greater than for IPP infections might lower infection rate improved cell base excess
Pineda M, Burnett AL. Penile Prosthesis Infections-A Review of Risk Factors, Prevention, and Treatment. Sex Med Rev. 2016;4(4):389–98.
Cakan M, Demirel F, Karabacak O, Yalcinkaya F, Altug U. Risk factors for penile prosthetic infection. Int Urol Nephrol. 2003;35(2):209–13.
Wilson SK, Delk JR 2nd. Inflatable penile implant infection: predisposing factors and treatment suggestions. J Urol. 1995;153(3 Pt 1):659–61.
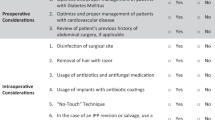
Lipsky MJ, Onyeji I, Golan R, Munarriz R, Kashanian JA, Stember DS, et al. Diabetes Is a Risk Factor for Inflatable Penile Prosthesis Infection: Analysis of a Large Statewide Database. Sex Med. 2019;7(1):35–40.
• Gross MS, Reinstatler L, Henry GD, et al. Multicenter Investigation of Fungal Infections of Inflatable Penile Prostheses. J Sex Med. 2019;16(7):1100–5. Multi-institutional database review of IPP infections to examine for common patient and surgical factors related to IPP fungal infections. Fungal infection represent 12% of all penile prosthesis infections in our series and were seen mostly in diabetic are rate patients, who may benefit from antifungal prophylaxis.
Balen A, Gross MS, Phillips EA, Henry GD, Munarriz R. Active Polysubstance Abuse Concurrent With Surgery as a Possible Newly Identified Infection Risk Factor in Inflatable Penile Prosthesis Placement Based on a Retrospective Analysis of Health and Socioeconomic Factors. J Sex Med. 2016;13(4):697–701.
Hebert KJ, Kohler TS. Penile Prosthesis Infection: Myths and Realities. World J Mens Health. 2019;37(3):276–87.
Carson CC 3rd, Mulcahy JJ, Harsch MR. Long-term infection outcomes after original antibiotic impregnated inflatable penile prosthesis implants: up to 7.7 years of followup. J Urol. 2011;185(2):614–8.
Carrasquillo RJ, Munarriz RM, Gross MS. Infection Prevention Considerations for Complex Penile Prosthesis Recipients. Curr Urol Rep. 2019;20(3):12.
Jarow JP. Risk factors for penile prosthetic infection. J Urol. 1996;156(2 Pt 1):402–4.
Gross MS, Vollstedt AJ, Cleves MA, et al. Multicenter investigation on the influence of climate in penile prosthesis infection. Int J Impot Res. 2019.
Onyeji IC, Sui W, Pagano MJ, Weinberg AC, James MB, Theofanides MC, et al. Impact of Surgeon Case Volume on Reoperation Rates after Inflatable Penile Prosthesis Surgery. J Urol. 2017;197(1):223–9.
Kavoussi NL, Siegel JA, Viers BR, Pagliara TJ, Hofer MD, Cordon BH, et al. Preoperative Urine Culture Results Correlate Poorly With Bacteriology of Urologic Prosthetic Device Infections. J Sex Med. 2017;14(1):163–8.
Bode LG, Kluytmans JA, Wertheim HF, Bogaers D, Vandenbroucke-Grauls CM, Roosendaal R, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362(1):9–17.
Chlebicki MP, Safdar N, O'Horo JC, Maki DG. Preoperative chlorhexidine shower or bath for prevention of surgical site infection: a meta-analysis. Am J Infect Control. 2013;41(2):167–73.
Wolf JS, Bennett CJ, Dmochowski RR, Hollenbeck BK, Pearle MS, Schaeffer AJ. Best Practice Policy Statement on Urologic Surgery Antimicrobial Prophylaxis. J Urol. 2008;179(4):1379–90.
Grabe M, Bartolett R, Bjerklund Johansen TEB, et al. Guidelines of Urological Infections. https://uroweb.org/wp-content/uploads/19-Urological-infections_LR2.pdf. Published 2015. Accessed September 22, 2019.
Mandava SH, Serefoglu EC, Freier MT, Wilson SK, Hellstrom WJ. Infection retardant coated inflatable penile prostheses decrease the incidence of infection: a systematic review and meta-analysis. J Urol. 2012;188(5):1855–60.
Henry GD, Kansal NS, Callaway M, et al. Centers of excellence concept and penile prostheses: an outcome analysis. J Urol. 2009;181(3):1264–8.
Katz BF, Gaunay GS, Barazani Y, Nelson CJ, Moreira DM, Dinlenc CZ, et al. Use of a preoperative checklist reduces risk of penile prosthesis infection. J Urol. 2014;192(1):130–5.
Darouiche RO, Wall MJ Jr, Itani KM, et al. Chlorhexidine-Alcohol versus Povidone-Iodine for Surgical-Site Antisepsis. N Engl J Med. 2010;362(1):18–26.
Yeung LL, Grewal S, Bullock A, Lai HH, Brandes SB. A comparison of chlorhexidine-alcohol versus povidone-iodine for eliminating skin flora before genitourinary prosthetic surgery: a randomized controlled trial. J Urol. 2013;189(1):136–40.
Eid JF. No-touch technique. J Sex Med. 2011;8(1):5–8.
Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209–15.
Greif R, Akça O, Horn E-P, Kurz A, Sessler DI. Supplemental Perioperative Oxygen to Reduce the Incidence of Surgical-Wound Infection. N Engl J Med. 2000;342(3):161–7.
Rosenberger LH, Politano AD, Sawyer RG. The surgical care improvement project and prevention of post-operative infection, including surgical site infection. Surg Infect. 2011;12(3):163–8.
• Gross MS, Phillips EA, Balen A, et al. The Malleable Implant Salvage Technique: Infection Outcomes after Mulcahy Salvage Procedure and Replacement of Infected Inflatable Penile Prosthesis with Malleable Prosthesis. J Urol. 2016;195(3):694–7. Multi-institutional retrospective review of 58 patients treated between 2002 and 2014 who underwent Mulcahy salvage with inflatable penile prosthesis removal and replacement with malleable prosthesis. This analysis shows a high infection free rate. Additionally 17 of 54 patient who remained infection free were able to successfully undergo subsequent removal of the malleable prosthesis replacement with an inflatable penile prosthesis.
Lao M, Graydon RJ, Bieniek JM. Salvage penile prosthetic surgery utilizing temporary malleable implants. Transl Androl Urol. 2017;6(Suppl 5):S806–12.
Mulcahy JJ. Long-term experience with salvage of infected penile implants. J Urol. 2000;163(2):481–2.
Pan S, Rodriguez D, Thirumavalavan N, Gross MS, Eid JF, Mulcahy J, et al. The Use of Antiseptic Solutions in the Prevention and Management of Penile Prosthesis Infections: A Review of the Cytotoxic and Microbiological Effects of Common Irrigation Solutions. J Sex Med. 2019;16(6):781–90.
Manka M, Hebert K, Dodge N, Yang D, Kohler T, Trost L. MP27-18 INTRAOPERATIVE USE OF BETADINE IRRIGATION IS ASSOCIATED WITH A 9-FOLD INCREASE OF PENILE PROSTHESIS INFECTION. J Urol. 2019;201(Supplement 4):e370–1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Rezaee, Dr. Butaney, and Dr. Thirumavalavan each declare they have no conflicts of interest to disclose. This research study was not supported financially.
Dr. Gross reports grants and personal fees from Coloplast, outside the submitted work.
Dr. Munarriz reports his role as a consultant and investigator for Coloplast.
Research Involving Human Participants and/or Animals
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Male Sexual Dysfunction and Disorders
Rights and permissions
About this article
Cite this article
Rezaee, M.E., Butaney, M., Thirumavalavan, N. et al. Advances in Infection Prevention Strategies for Penile Prosthesis Surgery. Curr Sex Health Rep 11, 399–405 (2019). https://doi.org/10.1007/s11930-019-00235-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11930-019-00235-6