Abstract
Purpose of Review
Amyloid A (AA) amyloidosis is an organ- or life-threatening complication of chronic inflammatory disorders. Here, we review the epidemiology, causes, pathogenesis, clinical features, and diagnostic and therapeutic strategies of AA amyloidosis.
Recent Findings
The incidence of AA amyloidosis has declined due to better treatment of the underlying diseases. Histopathological examination is the gold standard of diagnosis, but magnetic resonance imaging can be used to detect cardiac involvement. There is yet no treatment option for the clearance of amyloid fibril deposits; therefore, the management strategy primarily aims to reduce serum amyloid A protein. Anti-inflammatory biologic agents have drastically expanded our therapeutic armamentarium. Kidney transplantation is preferred in patients with kidney failure, and the recurrence of amyloidosis in the allograft has become rare as transplant recipients have started to benefit from the new agents.
Summary
The management of AA amyloidosis has been considerably changed over the recent years due to the novel therapeutic options aiming to control inflammatory activity. New agents capable of clearing amyloid deposits from the tissues are still needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disorders that create sustained inflammatory responses can result in extracellular deposition of amyloid A (AA) fibrils in various organs. These fibrils are derived from an acute-phase reactant, serum AA (SAA) protein, through a long process including cleavage, misfolding, and aggregation into an insoluble beta-sheet form [1]. The incidence of AA amyloidosis has been low in recent years especially in developed countries due to declining rates of chronic infections and better treatment strategies for inflammatory conditions including autoimmune and autoinflammatory diseases. However, it still continues to be a significant cause of morbidity and mortality if left untreated or undertreated. Herein, we will review the causes, pathogenesis, and clinical features with an emphasis on histological diagnosis as well as conventional and novel treatment strategies of AA amyloidosis. As the kidney is the major affected organ and the damage in kidneys usually defines the prognosis of AA amyloidosis [2], we will devote a separate section to various aspects of patients treated with kidney replacement therapies.
Epidemiology and Causes
The incidence of AA amyloidosis has been reported as one to two cases per million person-years [3, 4], yet these rates may be higher in resource-limited settings. As the incidence is in decline, its frequency among all forms of amyloidosis is being replaced by other types such as immunoglobulin light chain (AL) and transthyretin amyloidosis [2], and a recent proteomics study involving 16,175 samples revealed that only 2.9% of all cases suffered from AA amyloidosis [5, 6••]. Median age at diagnosis has been historically around 50 years, but it has recently been reported as high as 70 [7, 8]. Males are slightly more affected [8].
Even though any disorder causing sustained inflammation may increase the risk of AA amyloidosis, chronic infections and inflammatory arthritis are the commonest causes [2]. Primary immunodeficiencies leading to infections and immune dysregulation may create a state of chronic inflammation, and in particular, delays in diagnosis and therapeutic interventions were associated with the development of AA amyloidosis [9]. Monogenic periodic fever syndromes also constitute a significant risk for amyloidosis, and familial Mediterranean fever (FMF) is a prevalent cause for people originating from the Mediterranean basin [10•]. A substantial proportion of cases (up to 20%) appear to develop AA amyloidosis in the absence of overt inflammation and thus labeled idiopathic [11]. Obesity was suggested as a cause or susceptibility factor [5, 12], but yet undefined genetic and/or environmental causes might be involved in the pathogenesis of both obese and idiopathic cases [2]. The causes of AA amyloidosis are detailed in Table 1.
Pathogenesis
Pathogenesis of AA amyloidosis revolves around a cascade of events triggered by sustained inflammation and increased production of SAA, cleavage of the signal peptide, aberrant aggregation, SAA-derived fibril formation, and deposition of amyloid fibrils [13]. Amyloid formation typically involves misfolding of soluble precursor proteins into a beta-sheet structure, and the monomeric protein then aggregates into fibril conformations that are insoluble and show resistance to proteolytic enzymes [14]. Thirty-six different monomeric human precursor proteins like SAA have been recognized so far with the potential to form amyloid fibrils, which then cause systemic or localized amyloidosis [15].
SAA is an apolipoprotein of high-density lipoprotein synthesized especially by hepatocytes as an acute-phase reactant, primarily under the influence of pro-inflammatory cytokines such as interleukin-1 (IL-1), IL-6, and tumor necrosis factor-alpha (TNF-α) [16]. SAA is involved in lipid transfer and immune regulation during acute-phase responses including cytokine induction, matrix metalloproteinase (MMP) stimulation, phagocyte migration, chemoattraction, and bacterial opsonization [16, 17]. Also, it has a role in the atherosclerosis [18] through an interaction between lipid homeostasis and inflammatory cells and contributes to chronic injury in arthritis and tumor metastases [19, 20]. Table 2 summarizes several important factors that contribute to the amyloidogenic potential of SAA in addition to its physiologic functions.
Human SAA proteins are encoded by four SAA genes on chromosome 11p15.1 [21]. SAA1 and SAA2 are both acute-phase proteins and associated with AA amyloidosis. SAA3 is a pseudogene, and SAA4 is a constitutively expressed non-acute phase protein. SAA1, which predominates AA deposits, has 5 polymorphic alleles (SAA1.1–1.5) with differing amyloidogenic potential among them. Homozygosity for SAA1.1 in the European population [22, 23] and SAA1.3 in the Japanese population [25] increases the risk of amyloidosis, which can be partially explained by the increased susceptibility of SAA1.1 allele to degradation by MMP than SAA1.5 [26]. Inducible expression of SAA1 and SAA2 by proinflammatory cytokines during acute-phase response impacts the serum concentration of SAA [21]. Moreover, certain single nucleotide variations within the SAA genes can also affect the production and stability of SAA isoforms [31], and genotype–phenotype associations have been well described in patients with periodic fever syndromes [32]. In addition to the homozygosity for the most penetrant MEFV gene variant M694V, which is associated with a severe disease course [8], homozygosity for SAA1.1 allele contributes to the risk of amyloidosis in FMF patients [33]. Recently, a family with AA amyloidosis due to a genetic mutation in the promoter region of the SAA1 gene has also been reported [24]. In a multicenter study, patients’ country of recruitment [34] has been identified as a risk factor for kidney amyloidosis, more important than the MEFV genotype and disease duration in FMF, which suggests that ethnicity and environmental factors may play an additional role.
Diagnosis
Clinical Features
AA amyloidosis manifests in multiple organs such as kidney, liver, gastrointestinal tract, peripheral nerves, heart, blood vessels, lungs, skin, and soft tissue. The expression of the disease is contingent upon the specific organs involved. Nevertheless, the prevailing symptoms frequently involve the emergence of proteinuria and gradual reduction in kidney function, apparent in over 90% of patients upon their initial presentation [1]. Nephrotic syndrome is noted in more than half of the patients, with approximately 10% exhibiting kidney failure at the time of presentation [1, 35, 36]. The site of the protein accumulation in kidneys varies, influencing clinical manifestations and disease progression. Typically, the involvement of glomeruli precipitates nephrotic-range proteinuria and an accelerated decline in estimated glomerular filtration rate (eGFR) [37]. Conversely, localized amyloid deposition within tubulointerstitium tends to result in less pronounced proteinuria. Individuals with tubular amyloid accumulation might exhibit bland urinary sediment and minimal proteinuria but can demonstrate symptoms of distal tubular impairment such as nephrogenic diabetes insipidus. Notably, crescentic glomerulonephritis, a rare event, may be ascribed to the rupture of the glomerular basement membrane due to amyloid deposition [38]. While the majority of cases follow an indolent course, a subset of individuals with FMF might undergo acute illness, marked by substantial proteinuria, elevated inflammatory markers, and rapid progression to kidney failure within weeks. These infrequent instances are named “amyloid storm,” which is thought to be precipitated by superimposed infections or other triggering events [39••].
Approximately 30% of cases have gastrointestinal involvement. The predominant symptom is diarrhea that is frequently unresponsive to standard treatment [11]. Other frequently encountered presenting symptoms include weight loss, abdominal pain, malabsorption, macroglossia, gastroesophageal reflux, esophageal dysmotility, gastric polyps, and episodes of upper and lower gastrointestinal bleeding [40]. Amyloid deposition in the myenteric plexus can potentially result in intestinal pseudo-obstruction [41]. While splenic and hepatic amyloid deposition is commonly detected in serum amyloid P (SAP) scintigraphy, its clinical relevance is limited [42]. Hepato- and splenomegaly commonly manifests during disease progression, whereas splenic rupture is exceptionally rare [1]. Elevated serum alkaline phosphatase (ALP) levels are noted in 5% of patients [1]. However, this may more accurately reflect underlying disease activity rather than amyloid deposition given that ALP functions as an acute-phase reactant. Incidences of increased serum aminotransferase and bilirubin levels have been seldomly reported, and liver failure is quite infrequent [43]. While cardiac infiltration is extensively documented in various amyloidosis types, it is a relatively rare cause of heart failure in AA amyloidosis [44]. Involvements of the thyroid, adrenals, and the nervous system might also be encountered [1, 11, 45].
Histology
A biopsy from the involved tissue demonstrating amyloid deposits provides the definitive diagnosis. Amyloid deposits within the tissue typically show high affinity for Congo red stain, which gives a characteristic birefringence under polarized light. For the diagnosis of AA amyloidosis subgroup, immunohistochemical analysis with anti-AA antibody is required [46]. Since AA amyloidosis is clinically more limited compared to AL amyloidosis and mostly involves the kidney, a kidney biopsy is usually rendered for diagnosis. Gastrointestinal tract, liver, spleen, and rarely heart can also be the location of a biopsy [46]. Salivary gland biopsy and periumbilical subcutaneous fat aspiration, or retrospective analysis of prior biopsies with Congo red staining may help as less invasive approaches with an overall sensitivity ranging from 77 to 89% [47,48,49]. If clinical suspicion is significantly high and these approaches render negative results, a sample should be retrieved from the affected organ.
The histopathological findings in the kidney of a patient with AA amyloidosis are shown in Fig. 1. Kidney deposits may be located in various compartments such as mesangium, glomerular basement membrane, arteries and arterioles, tubules, or interstitium [50]. It is typical for amyloid deposits to involve the mesangium first and the capillaries later, and if the entire glomerulus is involved with a nodular configuration, the histopathologic appearance may mimic light chain deposition disease, sclerosis, or diabetic nephropathy [51, 52]. Tubulointerstitial deposits might result in tubular atrophy and interstitial fibrosis [53]. The presence of amorphous hyaline deposits should raise a suspicion of amyloidosis which requires further examination with Congo red stain. These deposits typically show weak staining for periodic acid-Schiff and no staining for silver methenamine as the predominance of amyloid deposits reduces collagen deposition within the tissue [51]. Congo red stain should be routinely performed to rule out potential amyloid deposits since the deposits may be inconspicuous during the early courses of the disease and may lead to misdiagnosis of a podocytopathy in a patient with nephrotic-range proteinuria [54]. On electron microscopic examination, amyloid appears as rigid, randomly oriented, unbranched fibrils with a thickness of 8–12 nm in diameter. The fibril diameter is essential in differentiating amyloidosis from kidney diseases with fibrillary deposits, such as fibrillary glomerulonephritis with 15–20 nm and immunotactoid glomerulonephritis with 30–60 nm fibril diameters [55].
Kidney histology in a patient with AA amyloidosis. A Glomerulus with mesangial amorphous and eosinophilic deposits (hematoxylin and eosin, original magnification × 400). B Deposits not staining for silver methenamine (periodic Schiff-methenamine, original magnification × 400). C Congophilic glomerular deposits (Congo red, original magnification × 400). D Deposits showing apple green birefringence under polarized light (Congo red under polarized light, original magnification × 400). E Immunohistochemical reactivity for anti-AA antibody (original magnification × 400). F Randomly oriented, unbranched amyloid fibrils on electron microscopic examination (original magnification × 40,000). Deposits were marked with asterisks in panels A, B and C
In systemic amyloidosis, the amyloid precursor protein must be specified to guide the patient management [56]. Immunohistochemical analysis for SAA protein is the most commonly used method to detect AA amyloidosis [56]. Alternatively, direct immunofluorescence for kappa and lambda light chains on fresh frozen tissue is a reliable method to detect amyloid deposits and rule out AL amyloidosis in kidney biopsies [56]. Since various amyloid subtypes may involve different glomerular parts, these features are not entirely specific, and subtyping still requires immunohistochemical methods with specific antibodies against precursor proteins [50].
The accuracy of immunohistochemical technique depends on the quality of antibodies and the experience of the pathologist; hence, it may fail to determine the amyloid subtype accurately [57]. A false positive result is a diagnostic pitfall in especially determining AA amyloidosis [58]. Immunoelectron microscopy may yield higher sensitivity and specificity, identifying the amyloid subtype in more than 99% of cases; however, it suffers from limited use and lack of global experience [48, 59]. In the last decade, laser microdissection/mass spectrometry (LD/MS) has been used as an alternative but expensive method for amyloid detection, where amyloid deposits are extracted from the tissue via laser microdissection and then processed for protein extraction and mass spectrometer analysis. Although immune methods are still currently used, newer methods are expected to provide a more accurate diagnostic evaluation, especially when the standard approaches fail [53, 54, 60].
Imaging
Whole-body 123I-labeled SAP scintigraphy demonstrates a high sensitivity, reaching up to 90%, in diagnosing both AA and AL amyloidosis [61]. Additionally, it provides insights into the extent of organ involvement. Although it does not replace histological evaluation, SAP scintigraphy has substantially improved diagnostic precision and has been proven as a valuable tool in disease progression and monitoring therapy [62]. However, routine diagnostic application of SAP scintigraphy has a significant obstacle due to its very limited accessibility. It is exclusively performed in highly specialized centers, primarily owing to its high costs and technical intricacies. Moreover, the limited half-life of the isotope renders it impractical for the assessment of cardiac involvement [62]. Additionally, the capacity to evaluate intracerebral or peripheral nerve amyloidosis is impeded by the gradual infiltration of SAP into the nervous system [1].
There are several imaging modalities available for assessing cardiac amyloidosis. Two-dimensional Doppler echocardiography has been traditionally employed to illustrate the thickening of ventricular walls and valves, as well as to assess diastolic restrictive dysfunction associated with amyloid infiltration. Cardiac involvement is characterized by a mean left ventricular wall thickness exceeding 12 mm, excluding hypertension or other causes of left ventricular hypertrophy [63]. Cardiac magnetic resonance (CMR) imaging is gaining prominence in the swiftly evolving domain of cardiac investigations. Notably, late or diffusely distributed subendocardial gadolinium enhancement serves as a distinctive hallmark of amyloidosis in CMR [64]. Even though use of gadolinium in patients with low eGFR was traditionally discouraged, American College of Radiology group II and III agents have been reported to be very safe [65, 66]. While the specific role of CMR in tracking the progression or regression of amyloidosis remains undefined, the application of equilibrium CMR, previously validated for fibrosis, holds promise as a valuable tool for quantifying amyloid [67].
Treatment
General Principles and Supportive Measures
The management of AA amyloidosis has been drastically changed over the recent decades as novel therapeutic options have transformed the treatment of inflammatory conditions [36]. Historically, our options were restricted to medications that would nonspecifically target inflammation, such as colchicine, non-steroidal anti-inflammatory agents, glucocorticoids and even cyclophosphamide, with somewhat variable but potentially favorable results if started in a timely fashion [68,69,70]. As our understanding of the pathogenesis of inflammatory diseases progressed and our therapeutic armamentarium expanded with tailored potent anti-inflammatory therapies, there has been a paradigm shift in AA amyloidosis therapeutics.
The mainstay of treatment is targeted at managing the underlying pathogenic mechanisms by suppressing the cytokine-induced production of SAA protein by the liver. Notably, controlling inflammation is time-sensitive as delayed control of the inflammation cannot prevent the development of amyloid fibril deposits and can lead to disease progression [1]. Hence, treatment options are tailored accordingly, with infections treated promptly with antimicrobials, and rheumatological and genetic autoinflammatory conditions treated with the appropriate anti-inflammatory therapies. The monitoring of the treatment response is essential by the assessment of inflammatory symptoms as well as biochemical parameters with the measurements of SAA, as decreased levels have been consistently associated with the regression of amyloid deposition, improved organ function, and reduced mortality, or conversely, uncontrolled high SAA concentrations have been linked to progressive disease and increased mortality [1, 71].
Supportive measures are usually needed during the disease course, especially when the kidneys are affected. It is imperative to prevent further insults such as hypoperfusion or nephrotoxic drug use. In nephrotic syndrome or nephrotic-range proteinuria, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers are the first choice of drugs with antiproteinuric properties, and patients should restrict dietary sodium to < 2 g/day to reduce edema [72]. Loop diuretics are generally required to manage hypervolemia, which should be combined with mechanistically different diuretics in resistant cases [72]. Hyperlipidemia, hypercoagulability, and symptoms originating from each affected organ should be treated according to the guidelines/recommendations.
In light of the above, we will review the different anti-inflammatory agents used in the treatment of AA amyloidosis and the recently investigated experimental therapies.
Systemic Anti-inflammatory Agents
Colchicine has become the mainstay of FMF treatment after its efficacy in preventing attacks was demonstrated in 1970s [73]. It suppresses inflammasome activation and IL-1β production by inhibiting caspase-1 and causes secondary reductions in other pro-inflammatory cytokines like TNF-α and IL-6 [74]. In a study examining 960 patients with FMF without evidence of amyloidosis at baseline, the cumulative rate of proteinuria after 11 years was reported as 1.7% in colchicine-compliant patients while 48.9% in the non-compliants [75]. Additionally, proteinuria resolved in 5 of 86 (5.8%) patients with non-nephrotic range proteinuria and stabilized in 68 (79.1%). In another study evaluating 68 FMF patients with amyloidosis, deterioration in kidney function was associated with a baseline serum creatinine of > 1.5 mg/dl and colchicine dose of < 1.5 mg/day [76]. However, evidence for its efficacy in AA amyloidosis due to causes other than FMF is still quite limited [68, 77].
Studies evaluating anti-TNF therapy in AA amyloidosis predominantly include patients with rheumatoid arthritis and spondyloarthritis. In a retrospective series including 15 patients treated with anti-TNF, amyloidosis progressed in seven patients (46.7%), stabilized in five (33.3%), and regression of proteinuria occurred in three (20%) in 10 months [78]. Notably, in a multicenter study in which 36 patients with AA amyloidosis treated with anti-TNF therapy were followed prospectively for 5 years, > 50% decrease in proteinuria was observed in more than half of the patients [79]. Starting anti-TNF agents early in the disease course, especially when the baseline serum creatinine level was < 1.5 mg/dl, may improve the prognosis of the kidney disease [80]. Moreover, several reports showed improvement in AA amyloidosis with tocilizumab (anti-IL-6 receptor monoclonal antibody) treatment [81]. Notably, a retrospective analysis including 42 patients with AA amyloidosis demonstrated that tocilizumab was superior to anti-TNFs in terms of obtaining a decrease in SAA, improvement in kidney function, and suppression of the disease activity [82]. Anti-TNF agents are also used to treat inflammatory bowel diseases and improvement of AA amyloidosis in these patients has also been reported [83].
Considering the central role of IL-1 in the pathogenesis of autoinflammatory diseases, IL-1 blockade has become an important target. Efficacies of anakinra (a recombinant homolog of the human IL-1 receptor antagonist), rilonacept (an IL-1 receptor fusion protein), and canakinumab (fully human anti-IL-1β monoclonal antibody) in monogenic inflammasomopathies such as FMF, NLRP3-associated autoinflammatory disorder (formerly known as cryopyrin-associated periodic syndrome), TNF receptor-associated periodic syndrome (TRAPS), mevalonate kinase deficiency, and in other inflammasome-associated diseases with complex etiology such systemic onset juvenile idiopathic arthritis have been extensively shown in various studies [84••, 85,86,87,88,89, 90••, 91,92,93].
Experimental Therapies
The advent of assays capable of defining the structure of the SAA has allowed us to understand better the biochemical basis of this protein folding disorder and explore the possibility of tailoring drugs aimed at protein misfolding prevention and promoting its removal [27, 94]. First significant attempt at exploring this was eprodisate, a molecule preventing SAA deposition by interacting with its polymerization. Initial results reported that eprodisate slowed the kidney function decline [95], which was not confirmed in a randomized control trial (NCT01215747) [96].
Further efforts have been attempted to deactivate the chaperone protein SAP which is responsible for facilitating the folding of amyloid proteins [97]. Miridesap, a serum SAP inhibitor, was initially investigated in a mixed amyloidosis population, followed by subsequent trials where it was administered in tandem with dezamizumab, a monoclonal antibody targeting SAP tissue depositions [98, 99•, 100]. These interventions appeared to remove the amyloid deposited in the organs of a small sample of patients, but the development was unfortunately discontinued due to fatal adverse effects during the clearance of amyloid deposits. Subsequently, a per os formulation of miridesap that achieves similar adequate blood levels as the parenteral formulation was reported, but no further investigation was pursued as arrhythmias were observed in the initial study [101].
The use of anti-sense oligonucleotides suppressing SAA production demonstrated a decreased amyloid organ deposition, yet its effects have not been studied in humans to date [102]. The development of new treatment options, which can effectively clear amyloid deposits from the tissues, is needed.
Dialysis and Kidney Transplantation
Dialysis modalities and kidney transplantation are both suitable for patients suffering from AA amyloidosis and kidney failure [5]. Still, survival is poor among patients on dialysis, especially when cardiac involvement is prevalent [103]. Notably, the tendency to hypotension due to cardiovascular amyloid deposition and nephrotic syndrome might constitute a significant problem in these patients.
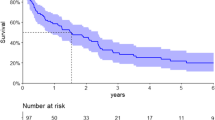
Even though kidney transplantation is the optimal treatment, 10-year patient and graft survival in patients with AA amyloidosis were reported as low as 62.3% and 56.4%, respectively [104]. However, contemporary series from the last years demonstrated higher patient and graft survival rates [105, 106••]. Recurrence is associated with a quite dismal prognosis [105], and it has recently become scarce due to better diagnosis and treatment of the underlying disorders [106••], but the diagnosis of subclinical recurrence in the graft should not be overlooked as many centers do not routinely perform protocol biopsies. Mortality after transplantation has been reported as high, mostly due to the involvement of the cardiovascular system [105, 107]. Therefore, a thorough cardiac assessment before transplantation has the utmost significance in patients with AA amyloidosis although its utility in the general transplant population is currently under debate.
Ant-TNF use in kidney transplant recipients (KTRs) has been associated with a better control of inflammation and remission of the underlying disease at the cost of increased rate of infections [108]. The results are expected as these agents are commonly used on top of maintenance immunosuppression. Notably, we recently evaluated 36 KTRs with FMF who showed resistance or inadequate response to colchicine and used anakinra or canakinumab in comparison with a propensity score-matched control group of KTRs [109••]. Anakinra and canakinumab were quite effective, culminating in longer graft survival and lower rejection rates but an increased number of deaths, which might have originated not only from infections but also the progression of the deposition of amyloid fibrils in the cardiovascular system. Colchicine has been reported to be safe in KTRs [105], but tacrolimus should be preferred over cyclosporine since the latter might increase the serum level or the effects of colchicine resulting in toxicity [110].
Conclusions
AA amyloidosis is a serious complication of chronic inflammatory disorders and predominantly affects the kidneys. It has become quite rare due to the reduced rates of chronic infections and better treatment strategies for highly inflammatory autoimmune and autoinflammatory diseases. Diagnosis still relies on histology, and the therapeutic approach must aim to reduce SAA levels and keep in within normal limits. In addition to conventional therapies, biologic agents such as anti-TNFs and IL-1 and IL-6 antagonists have considerably expanded our therapeutic armamentarium. Kidney transplantation is preferred when amyloidosis results in progression to kidney failure. Recurrence after transplantation has also become scarce due to the aforementioned treatment options, but higher rates of infection and mortality might be of concern. Experimental therapies aiming to clear amyloid deposits from the tissues have not been successful so far.
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lachmann HJ, Goodman HJ, Gilbertson JA, Gallimore JR, Sabin CA, Gillmore JD, et al. Natural history and outcome in systemic AA amyloidosis. N Engl J Med. 2007;356(23):2361–71. https://doi.org/10.1056/NEJMoa070265.
Papa R, Lachmann HJ. Secondary, AA, Amyloidosis. Rheum Dis Clin North Am. 2018;44(4):585–603. https://doi.org/10.1016/j.rdc.2018.06.004.
Hemminki K, Li X, Försti A, Sundquist J, Sundquist K. Incidence and survival in non-hereditary amyloidosis in Sweden. BMC Public Health. 2012;12:974. https://doi.org/10.1186/1471-2458-12-974.
Aguirre MA, Boietti BR, Nucifora E, Sorroche PB, González Bernaldo de Quirós F, Giunta DH, et al. Incidence rate of amyloidosis in patients from a medical care program in Buenos Aires, Argentina: a prospective cohort. Amyloid. 2016;23(3):184–7. https://doi.org/10.1080/13506129.2016.1207626.
Karam S, Haidous M, Royal V, Leung N. Renal AA amyloidosis: presentation, diagnosis, and current therapeutic options: a review. Kidney Int. 2023;103(3):473–84. https://doi.org/10.1016/j.kint.2022.10.028.
Dasari S, Theis JD, Vrana JA, Rech KL, Dao LN, Howard MT, et al. Amyloid typing by mass spectrometry in clinical practice: a comprehensive review of 16,175 samples. Mayo Clin Proc. 2020;95(9):1852–64. https://doi.org/10.1016/j.mayocp.2020.06.029. A significant study addressing the clinical use of mass spectrometry in amyloidosis.
Real de Asúa D, Costa R, Galván JM, Filigheddu MT, Trujillo D, Cadiñanos J. Systemic AA amyloidosis: epidemiology, diagnosis, and management. Clin Epidemiol. 2014;6:369–77. https://doi.org/10.2147/clep.S39981.
Bektas M, Koca N, Oguz E, Sari S, Dagci G, Ince B, et al. Characteristics and course of patients with AA amyloidosis: single centre experience with 174 patients from Turkey. Rheumatology (Oxford). 2024;63(2):319–28. https://doi.org/10.1093/rheumatology/kead465.
Delplanque M, Galicier L, Oziol E, Ducharme-Bénard S, Oksenhendler E, Buob D, et al. AA Amyloidosis secondary to primary immune deficiency: about 40 cases including 2 new French cases and a systematic literature review. J Allergy Clin Immunol Pract. 2021;9(2):745-52.e1. https://doi.org/10.1016/j.jaip.2020.09.023.
Lachmann HJ. Periodic fever syndromes. Best Pract Res Clin Rheumatol. 2017;31(4):596–609. https://doi.org/10.1016/j.berh.2017.12.001. A recent review of periodic fever syndromes that are known to result in AA amyloidosis if left untreated or undertreated.
Bunker D, Gorevic P. AA amyloidosis: Mount Sinai experience, 1997–2012. Mt Sinai J Med. 2012;79(6):749–56. https://doi.org/10.1002/msj.21342.
Blank N, Hegenbart U, Dietrich S, Brune M, Beimler J, Röcken C, et al. Obesity is a significant susceptibility factor for idiopathic AA amyloidosis. Amyloid. 2018;25(1):37–45. https://doi.org/10.1080/13506129.2018.1429391.
Westermark GT, Fändrich M, Westermark P. AA amyloidosis: pathogenesis and targeted therapy. Annu Rev Pathol. 2015;10:321–44. https://doi.org/10.1146/annurev-pathol-020712-163913.
Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med. 2003;349(6):583–96. https://doi.org/10.1056/NEJMra023144.
Benson MD, Buxbaum JN, Eisenberg DS, Merlini G, Saraiva MJM, Sekijima Y, et al. Amyloid nomenclature 2020: update and recommendations by the International Society of Amyloidosis (ISA) nomenclature committee. Amyloid. 2020;27(4):217–22. https://doi.org/10.1080/13506129.2020.1835263.
Sack GH Jr. Serum amyloid A (SAA) proteins. Subcell Biochem. 2020;94:421–36. https://doi.org/10.1007/978-3-030-41769-7_17.
Shah C, Hari-Dass R, Raynes JG. Serum amyloid A is an innate immune opsonin for Gram-negative bacteria. Blood. 2006;108(5):1751–7. https://doi.org/10.1182/blood-2005-11-011932.
Getz GS, Krishack PA, Reardon CA. Serum amyloid A and atherosclerosis. Curr Opin Lipidol. 2016;27(5):531–5. https://doi.org/10.1097/mol.0000000000000331.
Connolly M, Mullan RH, McCormick J, Matthews C, Sullivan O, Kennedy A, et al. Acute-phase serum amyloid A regulates tumor necrosis factor α and matrix turnover and predicts disease progression in patients with inflammatory arthritis before and after biologic therapy. Arthritis Rheum. 2012;64(4):1035–45. https://doi.org/10.1002/art.33455.
Malle E, Sodin-Semrl S, Kovacevic A. Serum amyloid A: an acute-phase protein involved in tumour pathogenesis. Cell Mol Life Sci. 2009;66(1):9–26. https://doi.org/10.1007/s00018-008-8321-x.
Uhlar CM, Whitehead AS. Serum amyloid A, the major vertebrate acute-phase reactant. Eur J Biochem. 1999;265(2):501–23. https://doi.org/10.1046/j.1432-1327.1999.00657.x.
Booth DR, Booth SE, Gillmore JD, Hawkins PN, Pepys MB. SAA1 alleles as risk factors in reactive systemic AA amyloidosis. Amyloid. 1998;5(4):262–5. https://doi.org/10.3109/13506129809007299.
Yilmaz E, Balci B, Kutlay S, Ozen S, Ertürk S, Oner A, et al. Analysis of the modifying effects of SAA1, SAA2 and TNF-alpha gene polymorphisms on development of amyloidosis in FMF patients. Turk J Pediatr. 2003;45(3):198–202.
Sikora J, Kmochová T, Mušálková D, Pohludka M, Přikryl P, Hartmannová H, et al. A mutation in the SAA1 promoter causes hereditary amyloid A amyloidosis. Kidney Int. 2022;101(2):349–59. https://doi.org/10.1016/j.kint.2021.09.007.
Baba S, Masago SA, Takahashi T, Kasama T, Sugimura H, Tsugane S, et al. A novel allelic variant of serum amyloid A, SAA1 gamma: genomic evidence, evolution, frequency, and implication as a risk factor for reactive systemic AA-amyloidosis. Hum Mol Genet. 1995;4(6):1083–7. https://doi.org/10.1093/hmg/4.6.1083.
van der Hilst JC, Yamada T, Op den Camp HJ, van der Meer JW, Drenth JP, Simon A. Increased susceptibility of serum amyloid A 1.1 to degradation by MMP-1: potential explanation for higher risk of type AA amyloidosis. Rheumatology (Oxford). 2008;47(11):1651–4. https://doi.org/10.1093/rheumatology/ken371.
Lu J, Yu Y, Zhu I, Cheng Y, Sun PD. Structural mechanism of serum amyloid A-mediated inflammatory amyloidosis. Proc Natl Acad Sci U S A. 2014;111(14):5189–94. https://doi.org/10.1073/pnas.1322357111.
Bansal A, Schmidt M, Rennegarbe M, Haupt C, Liberta F, Stecher S, et al. AA amyloid fibrils from diseased tissue are structurally different from in vitro formed SAA fibrils. Nat Commun. 2021;12(1):1013. https://doi.org/10.1038/s41467-021-21129-z.
Pepys MB. Amyloidosis. Annu Rev Med. 2006;57:223–41. https://doi.org/10.1146/annurev.med.57.121304.131243.
Gharibyan AL, Zamotin V, Yanamandra K, Moskaleva OS, Margulis BA, Kostanyan IA, et al. Lysozyme amyloid oligomers and fibrils induce cellular death via different apoptotic/necrotic pathways. J Mol Biol. 2007;365(5):1337–49. https://doi.org/10.1016/j.jmb.2006.10.101.
Migita K, Agematsu K, Masumoto J, Ida H, Honda S, Jiuchi Y, et al. The contribution of SAA1 polymorphisms to Familial Mediterranean fever susceptibility in the Japanese population. PLoS ONE. 2013;8(2):e55227. https://doi.org/10.1371/journal.pone.0055227.
Papa R, Doglio M, Lachmann HJ, Ozen S, Frenkel J, Simon A, et al. A web-based collection of genotype-phenotype associations in hereditary recurrent fevers from the Eurofever registry. Orphanet J Rare Dis. 2017;12(1):167. https://doi.org/10.1186/s13023-017-0720-3.
Atoyan S, Hayrapetyan H, Sarkisian T, Ben-Chetrit E. MEFV and SAA1 genotype associations with clinical features of familial Mediterranean fever and amyloidosis in Armenia. Clin Exp Rheumatol. 2016;34(6 Suppl 102):72–6.
Touitou I, Sarkisian T, Medlej-Hashim M, Tunca M, Livneh A, Cattan D, et al. Country as the primary risk factor for renal amyloidosis in familial Mediterranean fever. Arthritis Rheum. 2007;56(5):1706–12. https://doi.org/10.1002/art.22507.
Palladini G, Riva E, Basset M, Russo F, Milani P, Pasquinucci E, et al. Prognostication of survival and progression to dialysis in AA amyloidosis. Amyloid. 2017;24(sup1):136–7. https://doi.org/10.1080/13506129.2017.1289917.
Lane T, Pinney JH, Gilbertson JA, Hutt DF, Rowczenio DM, Mahmood S, et al. Changing epidemiology of AA amyloidosis: clinical observations over 25 years at a single national referral centre. Amyloid. 2017;24(3):162–6. https://doi.org/10.1080/13506129.2017.1342235.
Uda H, Yokota A, Kobayashi K, Miyake T, Fushimi H, Maeda A, et al. Two distinct clinical courses of renal involvement in rheumatoid patients with AA amyloidosis. J Rheumatol. 2006;33(8):1482–7.
Nagata M, Shimokama T, Harada A, Koyama A, Watanabe T. Glomerular crescents in renal amyloidosis: an epiphenomenon or distinct pathology? Pathol Int. 2001;51(3):179–86. https://doi.org/10.1046/j.1440-1827.2001.01188.x.
Kukuy OL, Beckerman P, Dinour D, Ben-Zvi I, Livneh A. Amyloid storm: acute kidney injury and massive proteinuria, rapidly progressing to end-stage kidney disease in AA amyloidosis of familial Mediterranean fever. Rheumatology (Oxford). 2021;60(7):3235–42. https://doi.org/10.1093/rheumatology/keaa772. A retrospective analysis providing great insights to the very rare “amyloid storm.”
Dahiya DS, Kichloo A, Singh J, Albosta M, Wani F. Gastrointestinal amyloidosis: a focused review. World J Gastrointest Endosc. 2021;13(1):1–12. https://doi.org/10.4253/wjge.v13.i1.1.
den Braber-Ymker M, Heijker S, Lammens M, Croockewit S, Nagtegaal ID. Intestinal involvement in amyloidosis is a sequential process. Neurogastroenterol Motil. 2018;30(12):e13469. https://doi.org/10.1111/nmo.13469.
Hawkins PN. Serum amyloid P component scintigraphy for diagnosis and monitoring amyloidosis. Curr Opin Nephrol Hypertens. 2002;11(6):649–55. https://doi.org/10.1097/00041552-200211000-00013.
Ebert EC, Nagar M. Gastrointestinal manifestations of amyloidosis. Am J Gastroenterol. 2008;103(3):776–87. https://doi.org/10.1111/j.1572-0241.2007.01669.x.
Shah KB, Inoue Y, Mehra MR. Amyloidosis and the heart: a comprehensive review. Arch Intern Med. 2006;166(17):1805–13. https://doi.org/10.1001/archinte.166.17.1805.
Gertz MA, Kyle RA. Secondary systemic amyloidosis: response and survival in 64 patients. Medicine (Baltimore). 1991;70(4):246–56.
Georgin-Lavialle S, Savey L, Buob D, Bastard JP, Fellahi S, Karras A, et al. French practical guidelines for the diagnosis and management of AA amyloidosis. Rev Med Interne. 2023;44(2):62–71. https://doi.org/10.1016/j.revmed.2022.12.004.
Hazenberg BP, Bijzet J, Limburg PC, Skinner M, Hawkins PN, Butrimiene I, et al. Diagnostic performance of amyloid A protein quantification in fat tissue of patients with clinical AA amyloidosis. Amyloid. 2007;14(2):133–40. https://doi.org/10.1080/13506120701260224.
Wisniowski B, Wechalekar A. Confirming the diagnosis of amyloidosis. Acta Haematol. 2020;143(4):312–21. https://doi.org/10.1159/000508022.
van Gameren II, Hazenberg BP, Bijzet J, van Rijswijk MH. Diagnostic accuracy of subcutaneous abdominal fat tissue aspiration for detecting systemic amyloidosis and its utility in clinical practice. Arthritis Rheum. 2006;54(6):2015–21. https://doi.org/10.1002/art.21902.
Fedotov SA, Khrabrova MS, Anpilova AO, Dobronravov VA, Rubel AA. Noninvasive diagnostics of renal amyloidosis: current state and perspectives. Int J Mol Sci. 2022;23(20). https://doi.org/10.3390/ijms232012662.
Said SM, Sethi S, Valeri AM, Leung N, Cornell LD, Fidler ME, et al. Renal amyloidosis: origin and clinicopathologic correlations of 474 recent cases. Clin J Am Soc Nephrol. 2013;8(9):1515–23. https://doi.org/10.2215/cjn.10491012.
Sethi S, Theis JD. Pathology and diagnosis of renal non-AL amyloidosis. J Nephrol. 2018;31(3):343–50. https://doi.org/10.1007/s40620-017-0426-6.
Feitosa VA, Neves P, Jorge LB, Noronha IL, Onuchic LF. Renal amyloidosis: a new time for a complete diagnosis. Braz J Med Biol Res. 2022;55:e12284. https://doi.org/10.1590/1414-431X2022e12284.
Picken MM. Modern approaches to the treatment of amyloidosis: the critical importance of early detection in surgical pathology. Adv Anat Pathol. 2013;20(6):424–39. https://doi.org/10.1097/PAP.0b013e3182a92dc3.
Dember LM. Amyloidosis-associated kidney disease. J Am Soc Nephrol. 2006;17(12):3458–71. https://doi.org/10.1681/asn.2006050460.
Taylor MS, Sidiqi H, Hare J, Kwok F, Choi B, Lee D, et al. Current approaches to the diagnosis and management of amyloidosis. Intern Med J. 2022;52(12):2046–67. https://doi.org/10.1111/imj.15974.
Gilbertson JA, Theis JD, Vrana JA, Lachmann H, Wechalekar A, Whelan C, et al. A comparison of immunohistochemistry and mass spectrometry for determining the amyloid fibril protein from formalin-fixed biopsy tissue. J Clin Pathol. 2015;68(4):314–7. https://doi.org/10.1136/jclinpath-2014-202722.
Owen-Casey MP, Sim R, Cook HT, Roufosse CA, Gillmore JD, Gilbertson JA, et al. Value of antibodies to free light chains in immunoperoxidase studies of renal biopsies. J Clin Pathol. 2014;67(8):661–6. https://doi.org/10.1136/jclinpath-2014-202231.
Fernández de Larrea C, Verga L, Morbini P, Klersy C, Lavatelli F, Foli A, et al. A practical approach to the diagnosis of systemic amyloidoses. Blood. 2015;125(14):2239–44. https://doi.org/10.1182/blood-2014-11-609883.
Sethi S, Vrana JA, Theis JD, Dogan A. Mass spectrometry based proteomics in the diagnosis of kidney disease. Curr Opin Nephrol Hypertens. 2013;22(3):273–80. https://doi.org/10.1097/MNH.0b013e32835fe37c.
Law S, Gillmore JD. When to suspect and how to approach a diagnosis of amyloidosis. Am J Med. 2022;135(Suppl 1):S2-s8. https://doi.org/10.1016/j.amjmed.2022.01.004.
Hawkins PN, Lavender JP, Pepys MB. Evaluation of systemic amyloidosis by scintigraphy with 123I-labeled serum amyloid P component. N Engl J Med. 1990;323(8):508–13. https://doi.org/10.1056/nejm199008233230803.
Gertz MA, Comenzo R, Falk RH, Fermand JP, Hazenberg BP, Hawkins PN, et al. Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18–22 April 2004. Am J Hematol. 2005;79(4):319–28. https://doi.org/10.1002/ajh.20381.
Perugini E, Rapezzi C, Piva T, Leone O, Bacchi-Reggiani L, Riva L, et al. Non-invasive evaluation of the myocardial substrate of cardiac amyloidosis by gadolinium cardiac magnetic resonance. Heart. 2006;92(3):343–9. https://doi.org/10.1136/hrt.2005.061911.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2024;105(4S):S117-S314. https://doi.org/10.1016/j.kint.2023.10.018.
Weinreb JC, Rodby RA, Yee J, Wang CL, Fine D, McDonald RJ, et al. Use of intravenous gadolinium-based contrast media in patients with kidney disease: consensus statements from the American College of Radiology and the National Kidney Foundation. Radiology. 2021;298(1):28–35. https://doi.org/10.1148/radiol.2020202903.
Flett AS, Hayward MP, Ashworth MT, Hansen MS, Taylor AM, Elliott PM, et al. Equilibrium contrast cardiovascular magnetic resonance for the measurement of diffuse myocardial fibrosis: preliminary validation in humans. Circulation. 2010;122(2):138–44. https://doi.org/10.1161/circulationaha.109.930636.
Livneh A, Zemer D, Langevitz P, Shemer J, Sohar E, Pras M. Colchicine in the treatment of AA and AL amyloidosis. Semin Arthritis Rheum. 1993;23(3):206–14. https://doi.org/10.1016/s0049-0172(05)80042-3.
Berglund K, Thysell H, Keller C. Results, principles and pitfalls in the management of renal AA-amyloidosis; a 10–21 year followup of 16 patients with rheumatic disease treated with alkylating cytostatics. J Rheumatol. 1993;20(12):2051–7.
Nakamura T, Yamamura Y, Tomoda K, Tsukano M, Shono M, Baba S. Efficacy of cyclophosphamide combined with prednisolone in patients with AA amyloidosis secondary to rheumatoid arthritis. Clin Rheumatol. 2003;22(6):371–5. https://doi.org/10.1007/s10067-003-0763-9.
Gillmore JD, Lovat LB, Persey MR, Pepys MB, Hawkins PN. Amyloid load and clinical outcome in AA amyloidosis in relation to circulating concentration of serum amyloid A protein. Lancet. 2001;358(9275):24–9. https://doi.org/10.1016/s0140-6736(00)05252-1.
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021;100(4S):S1-S276. https://doi.org/10.1016/j.kint.2021.05.021.
Zemer D, Revach M, Pras M, Modan B, Schor S, Sohar E, et al. A controlled trial of colchicine in preventing attacks of familial mediterranean fever. N Engl J Med. 1974;291(18):932–4. https://doi.org/10.1056/nejm197410312911803.
Leung YY, Yao Hui LL, Kraus VB. Colchicine–update on mechanisms of action and therapeutic uses. Semin Arthritis Rheum. 2015;45(3):341–50. https://doi.org/10.1016/j.semarthrit.2015.06.013.
Zemer D, Pras M, Sohar E, Modan M, Cabili S, Gafni J. Colchicine in the prevention and treatment of the amyloidosis of familial Mediterranean fever. N Engl J Med. 1986;314(16):1001–5. https://doi.org/10.1056/nejm198604173141601.
Livneh A, Zemer D, Langevitz P, Laor A, Sohar E, Pras M. Colchicine treatment of AA amyloidosis of familial Mediterranean fever. An analysis of factors affecting outcome. Arthritis Rheum. 1994;37(12):1804–11. https://doi.org/10.1002/art.1780371215.
Unverdi S, Inal S, Ceri M, Unverdi H, Batgi H, Tuna R, et al. Is colchicine therapy effective in all patients with secondary amyloidosis? Ren Fail. 2013;35(8):1071–4. https://doi.org/10.3109/0886022x.2013.811345.
Gottenberg JE, Merle-Vincent F, Bentaberry F, Allanore Y, Berenbaum F, Fautrel B, et al. Anti-tumor necrosis factor alpha therapy in fifteen patients with AA amyloidosis secondary to inflammatory arthritides: a followup report of tolerability and efficacy. Arthritis Rheum. 2003;48(7):2019–24. https://doi.org/10.1002/art.11163.
Fernández-Nebro A, Olivé A, Castro MC, Varela AH, Riera E, Irigoyen MV, et al. Long-term TNF-alpha blockade in patients with amyloid A amyloidosis complicating rheumatic diseases. Am J Med. 2010;123(5):454–61. https://doi.org/10.1016/j.amjmed.2009.11.010.
Esatoglu SN, Hatemi G, Ugurlu S, Gokturk A, Tascilar K, Ozdogan H. Long-term follow-up of secondary amyloidosis patients treated with tumor necrosis factor inhibitor therapy: a STROBE-compliant observational study. Medicine (Baltimore). 2017;96(34):e7859. https://doi.org/10.1097/md.0000000000007859.
Courties A, Grateau G, Philippe P, Flipo RM, Astudillo L, Aubry-Rozier B, et al. AA amyloidosis treated with tocilizumab: case series and updated literature review. Amyloid. 2015;22(2):84–92. https://doi.org/10.3109/13506129.2014.1002031.
Okuda Y, Ohnishi M, Matoba K, Jouyama K, Yamada A, Sawada N, et al. Comparison of the clinical utility of tocilizumab and anti-TNF therapy in AA amyloidosis complicating rheumatic diseases. Mod Rheumatol. 2014;24(1):137–43. https://doi.org/10.3109/14397595.2013.854048.
Serra I, Oller B, Mañosa M, Naves JE, Zabana Y, Cabré E, et al. Systemic amyloidosis in inflammatory bowel disease: retrospective study on its prevalence, clinical presentation, and outcome. J Crohns Colitis. 2010;4(3):269–74. https://doi.org/10.1016/j.crohns.2009.11.009.
Ben-Zvi I, Kukuy O, Giat E, Pras E, Feld O, Kivity S, et al. Anakinra for colchicine-resistant familial Mediterranean fever: a randomized, double-blind, placebo-controlled trial. Arthritis Rheumatol. 2017;69(4):854–62. https://doi.org/10.1002/art.39995. Randomized controlled trial of anakinra in patients with colchicine-resistant FMF which is a known cause of AA amyloidosis, especially in the Mediterranean basin.
Bodar EJ, Kuijk LM, Drenth JP, van der Meer JW, Simon A, Frenkel J. On-demand anakinra treatment is effective in mevalonate kinase deficiency. Ann Rheum Dis. 2011;70(12):2155–8. https://doi.org/10.1136/ard.2011.149922.
Neven B, Marvillet I, Terrada C, Ferster A, Boddaert N, Couloignier V, et al. Long-term efficacy of the interleukin-1 receptor antagonist anakinra in ten patients with neonatal-onset multisystem inflammatory disease/chronic infantile neurologic, cutaneous, articular syndrome. Arthritis Rheum. 2010;62(1):258–67. https://doi.org/10.1002/art.25057.
Gattorno M, Pelagatti MA, Meini A, Obici L, Barcellona R, Federici S, et al. Persistent efficacy of anakinra in patients with tumor necrosis factor receptor-associated periodic syndrome. Arthritis Rheum. 2008;58(5):1516–20. https://doi.org/10.1002/art.23475.
Lovell DJ, Giannini EH, Reiff AO, Kimura Y, Li S, Hashkes PJ, et al. Long-term safety and efficacy of rilonacept in patients with systemic juvenile idiopathic arthritis. Arthritis Rheum. 2013;65(9):2486–96. https://doi.org/10.1002/art.38042.
Hashkes PJ, Spalding SJ, Giannini EH, Huang B, Johnson A, Park G, et al. Rilonacept for colchicine-resistant or -intolerant familial Mediterranean fever: a randomized trial. Ann Intern Med. 2012;157(8):533–41. https://doi.org/10.7326/0003-4819-157-8-201210160-00003.
De Benedetti F, Gattorno M, Anton J, Ben-Chetrit E, Frenkel J, Hoffman HM, et al. Canakinumab for the treatment of autoinflammatory recurrent fever syndromes. N Engl J Med. 2018;378(20):1908–19. https://doi.org/10.1056/NEJMoa1706314. Landmark study of canakinumab for the treatment of periodic fever syndromes.
Ruperto N, Brunner HI, Quartier P, Constantin T, Wulffraat N, Horneff G, et al. Two randomized trials of canakinumab in systemic juvenile idiopathic arthritis. N Engl J Med. 2012;367(25):2396–406. https://doi.org/10.1056/NEJMoa1205099.
Hoffman HM, Throne ML, Amar NJ, Sebai M, Kivitz AJ, Kavanaugh A, et al. Efficacy and safety of rilonacept (interleukin-1 Trap) in patients with cryopyrin-associated periodic syndromes: results from two sequential placebo-controlled studies. Arthritis Rheum. 2008;58(8):2443–52. https://doi.org/10.1002/art.23687.
Goldbach-Mansky R, Shroff SD, Wilson M, Snyder C, Plehn S, Barham B, et al. A pilot study to evaluate the safety and efficacy of the long-acting interleukin-1 inhibitor rilonacept (interleukin-1 Trap) in patients with familial cold autoinflammatory syndrome. Arthritis Rheum. 2008;58(8):2432–42. https://doi.org/10.1002/art.23620.
Sack GH Jr. Serum amyloid A - a review. Mol Med. 2018;24(1):46. https://doi.org/10.1186/s10020-018-0047-0.
Dember LM, Hawkins PN, Hazenberg BP, Gorevic PD, Merlini G, Butrimiene I, et al. Eprodisate for the treatment of renal disease in AA amyloidosis. N Engl J Med. 2007;356(23):2349–60. https://doi.org/10.1056/NEJMoa065644.
(2016) Bellus Health: Phase 3 Results of Kiacta for AA Amyloidosis. https://www.drugdiscoverytrends.com/bellus-health-phase-3-results-of-kiacta-for-aa-amyloidosis/. Accessed February 9, 2024.
Tennent GA, Lovat LB, Pepys MB. Serum amyloid P component prevents proteolysis of the amyloid fibrils of Alzheimer disease and systemic amyloidosis. Proc Natl Acad Sci U S A. 1995;92(10):4299–303. https://doi.org/10.1073/pnas.92.10.4299.
Gillmore JD, Tennent GA, Hutchinson WL, Gallimore JR, Lachmann HJ, Goodman HJ, et al. Sustained pharmacological depletion of serum amyloid P component in patients with systemic amyloidosis. Br J Haematol. 2010;148(5):760–7. https://doi.org/10.1111/j.1365-2141.2009.08036.x.
Richards DB, Cookson LM, Berges AC, Barton SV, Lane T, Ritter JM, et al. Therapeutic clearance of amyloid by antibodies to serum amyloid p component. N Engl J Med. 2015;373(12):1106–14. https://doi.org/10.1056/NEJMoa1504942. Phase 1 trial of anti-SAP antibodies that are aimed to clear amyloid deposits from the affected tissues.
Richards DB, Cookson LM, Barton SV, Liefaard L, Lane T, Hutt DF, et al. Repeat doses of antibody to serum amyloid P component clear amyloid deposits in patients with systemic amyloidosis. Sci Transl Med. 2018;10(422). https://doi.org/10.1126/scitranslmed.aan3128.
Richards D, Bamford M, Liefaard L, Haque N, Lewis G, Storey J, et al. Identification, preclinical profile, and clinical proof of concept of an orally bioavailable pro-drug of miridesap. Br J Pharmacol. 2020;177(8):1853–64. https://doi.org/10.1111/bph.14956.
Kluve-Beckerman B, Du Hardwick, L, Benson MD. AA amyloidosis: potential therapy with antisense oligonucleotides. Amyloid. 2011;18(Suppl 1):200–2. https://doi.org/10.3109/13506129.2011.574354075.
Bollée G, Guery B, Joly D, Snanoudj R, Terrier B, Allouache M, et al. Presentation and outcome of patients with systemic amyloidosis undergoing dialysis. Clin J Am Soc Nephrol. 2008;3(2):375–81. https://doi.org/10.2215/cjn.02470607.
Gursu M, Yelken B, Caliskan Y, Kazancioglu R, Yazici H, Kilicaslan I, et al. Outcome of patients with amyloidosis after renal transplantation: a single-center experience. Int J Artif Organs. 2012;35(6):444–9. https://doi.org/10.5301/ijao.5000091.
Sarihan I, Caliskan Y, Mirioglu S, Ozluk Y, Senates B, Seyahi N, et al. Amyloid A amyloidosis after renal transplantation: an important cause of mortality. Transplantation. 2020;104(8):1703–11. https://doi.org/10.1097/tp.0000000000003043.
Schwarz C, Georgin-Lavialle S, Lombardi Y, Marion O, Jambon F, Legendre C, et al. Kidney transplantation in patients with AA amyloidosis: outcomes in a French multicenter cohort. Am J Kidney Dis. 2023. https://doi.org/10.1053/j.ajkd.2023.07.020. A very recent report showing the decline of recurrent AA amyloidosis in allografts due to better diagnosis and treatment of the underlying disorders.
Haq A, Hussain S, Meskat B, Mohan P, Conlon P, Hickey DP. Complications of renal transplantation in patients with amyloidosis. Transplant Proc. 2007;39(1):120–4. https://doi.org/10.1016/j.transproceed.2006.10.021.
Garrouste C, Anglicheau D, Kamar N, Bachelier C, Rivalan J, Pereira B, et al. Anti-TNFα therapy for chronic inflammatory disease in kidney transplant recipients: clinical outcomes. Medicine (Baltimore). 2016;95(41): e5108. https://doi.org/10.1097/md.0000000000005108.
Mirioglu S, Dirim AB, Bektas M, Demir E, Tor YB, Ozluk Y, et al. Efficacy and safety of interleukin-1 blockers in kidney transplant recipients with familial Mediterranean fever: a propensity score-matched cohort study. Nephrol Dial Transplant. 2023;38(5):1327–36. https://doi.org/10.1093/ndt/gfac335. The largest study on the efficacy and safety of IL-1 blockers in kidney transplant recipients suffering from FMF and AA amyloidosis.
Wason S, Digiacinto JL, Davis MW. Effect of cyclosporine on the pharmacokinetics of colchicine in healthy subjects. Postgrad Med. 2012;124(4):189–96. https://doi.org/10.3810/pgm.2012.07.2579.
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
SM designed the work. SM, OU, OH, GK, IB and SAD drafted the first version of the article. Critical revisions were led by EF and AG. All authors significantly contributed to the content and approved the final version to be submitted.
Corresponding author
Ethics declarations
Conflict of Interest
Outside the submitted work, SM received support for attending meetings and travel from Amgen and Sanofi Genzyme. GK received honoraria from Baxter, and support for attending meetings and travel from Amgen and Abdi Ibrahim Otsuka. AG received honoraria for advisory board meetings and speaker’s fees from Novartis, Sobi, and R-Pharm. Remaining authors have no disclosures.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mirioglu, S., Uludag, O., Hurdogan, O. et al. AA Amyloidosis: A Contemporary View. Curr Rheumatol Rep 26, 248–259 (2024). https://doi.org/10.1007/s11926-024-01147-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11926-024-01147-8