Abstract
Purpose of Review
The population over age 60 is growing more rapidly than the general population. Given the projected increase and need for data that can inform treatment, this review provides a brief description of newer publications focused on mania in older-age bipolar disorder (OABD), including epidemiology, diagnosis, and treatments.
Recent Findings
Age cutoffs to define OABD range from 50 to 65 years. OABD clinical presentation and course of illness is highly variable, often characterized by mood episode recurrence, medical comorbidity, cognitive deficits, and impaired functioning. There is little pharmacotherapy data on mania in OABD. Lithium and valproate have been tested in a single randomized controlled trial and there is data of more limited quality with other compounds.
Summary
Treating OABD is challenging due to medical complexity, comorbidity, diminished tolerance to treatment, and a limited evidence base. More data is needed to keep pace with clinical demand.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
World Population Ageing: 1950–2050. United Nations, Population Division DoEaSA.
World Health Organization. http://www.who.int/mediacentre/factsheets/fs381/en/. Accessed January 14 2016.
• Sajatovic M, Strejilevich SA, Gildengers AG, Dols A, Al Jurdi RK, Forester BP, et al. A report on older-age bipolar disorder from the International Society for Bipolar Disorders Task Force. Bipolar Disord. 2015;17(7):689–704. doi:10.1111/bdi.12331. This recently published report, resulting from a task force of the International Society for Bipolar Disorders (ISBD), addresses the unique aspects of OABD including epidemiology and clinical features, neuropathology and biomarkers, physical health, cognition, and care approaches. The report describes an expert consensus summary on OABD that is intended to advance the care of patients and shed light on issues relevant to BD research across the life span.
Sajatovic M, Chen P. Geriatric bipolar disorder. Psychiatr Clin North Am. 2011;34(2):319–333, vii. doi:10.1016/j.psc.2011.02.007.
Depp CA, Jeste DV. Bipolar disorder in older adults: a critical review. Bipolar Disord. 2004;6(5):343–67. doi:10.1111/j.1399-5618.2004.00139.x.
Sajatovic M, Chen P. Geriatric bipolar disorder: epidemiology, clinical features, assessment, and diagnosis. Philadelphia: Wolters Kluwer Health. https://www.uptodate.com. Accessed Feb 2017
Tariot PN, Podgorski CA, Blazina L, Leibovici A. Mental disorders in the nursing home: another perspective. Am J Psychiatry. 1993;150(7):1063–9. doi:10.1176/ajp.150.7.1063.
Depp CA, Lindamer LA, Folsom DP, Gilmer T, Hough RL, Garcia P, et al. Differences in clinical features and mental health service use in bipolar disorder across the lifespan. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 2005;13(4):290–8. doi:10.1176/appi.ajgp.13.4.290.
• Dols A, Kupka RW, van Lammeren A, Beekman AT, Sajatovic M, Stek ML. The prevalence of late-life mania: a review. Bipolar Disord. 2014;16(2):113–8. doi:10.1111/bdi.12104. The overall prevalence of late-life mania was estimated to be 6.0% in the reported 1519 older psychiatric inpatients from six studies. In elderly inpatients with bipolar disorder, the mean prevalence of late-onset mania was 44.2%. For other relevant care facilities, no firm conclusions could be drawn. Late-life mania is not rare in older psychiatric inpatients and late-onset mania is associated with increased somatic comorbidity in patients aged 50 years and older.
Prakash O, Kumar CN, Shivakumar PT, Bharath S, Varghese M. Clinical presentation of mania compared with depression: data from a geriatric clinic in India. Int Psychogeriatr/IPA. 2009;21(4):764–7. doi:10.1017/S1041610209009466.
Preville M, Boyer R, Grenier S, Dube M, Voyer P, Punti R, et al. The epidemiology of psychiatric disorders in Quebec’s older adult population. Can J Psychiatry. 2008;53(12):822–32. doi:10.1177/070674370805301208.
Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, et al. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry. 2009;66(7):785–95. doi:10.1001/archgenpsychiatry.2009.36.
Angst J, Gamma A, Sellaro R, Lavori PW, Zhang H. Recurrence of bipolar disorders and major depression. A life-long perspective. Eur Arch Psychiatry Clin Neurosci. 2003;253(5):236–40. doi:10.1007/s00406-003-0437-2.
Al Jurdi RK, Marangell LB, Petersen NJ, Martinez M, Gyulai L, Sajatovic M. Prescription patterns of psychotropic medications in elderly compared with younger participants who achieved a “recovered” status in the systematic treatment enhancement program for bipolar disorder. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 2008;16(11):922–33. doi:10.1097/JGP.0b013e318187135f.
Oostervink F, Boomsma MM, Nolen WA, Board EA. Bipolar disorder in the elderly; different effects of age and of age of onset. J Affect Disord. 2009;116(3):176–83. doi:10.1016/j.jad.2008.11.012.
Kupka RW, Luckenbaugh DA, Post RM, Leverich GS, Nolen WA. Rapid and non-rapid cycling bipolar disorder: a meta-analysis of clinical studies. J Clin Psychiatry. 2003;64(12):1483–94.
Cruz N, Vieta E, Comes M, Haro JM, Reed C, Bertsch J, et al. Rapid-cycling bipolar I disorder: course and treatment outcome of a large sample across Europe. J Psychiatr Res. 2008;42(13):1068–75. doi:10.1016/j.jpsychires.2007.12.004.
Almeida OP, McCaul K, Hankey GJ, Yeap BB, Golledge J, Flicker L. Risk of dementia and death in community-dwelling older men with bipolar disorder. Br J Psychiatry J Ment Sci. 2016;209(2):121–6. doi:10.1192/bjp.bp.115.180059.
Almeida OP, Fenner S. Bipolar disorder: similarities and differences between patients with illness onset before and after 65 years of age. Int Psychogeriatr/IPA. 2002;14(3):311–22.
Azorin JM, Kaladjian A, Adida M, Fakra E. Late-onset bipolar illness: the geriatric bipolar type VI. CNS Neurosci Ther. 2012;18(3):208–13. doi:10.1111/j.1755-5949.2011.00255.x.
Vasudev A, Thomas A. ‘Bipolar disorder’ in the elderly: what’s in a name? Maturitas. 2010;66(3):231–5. doi:10.1016/j.maturitas.2010.02.013.
Goldstein BI, Herrmann N, Shulman KI. Comorbidity in bipolar disorder among the elderly: results from an epidemiological community sample. Am J Psychiatry. 2006;163(2):319–21. doi:10.1176/appi.ajp.163.2.319.
Burt T, Prudic J, Peyser S, Clark J, Sackeim HA. Learning and memory in bipolar and unipolar major depression: effects of aging. Neuropsychiatry Neuropsychol Behav Neurol. 2000;13(4):246–53.
Broadhead J, Jacoby R. Mania in old age: a first prospective study. Int J Geriatr Psychiatry. 1990;5:215–22.
Young RC, Kiosses D, Heo M, Schulberg HC, Murphy C, Klimstra S, et al. Age and ratings of manic psychopathology. Bipolar Disord. 2007;9(3):301–4. doi:10.1111/j.1399-5618.2007.00393.x.
Forester BP, Ajilore O, Spino C, Lehmann SW. Clinical characteristics of patients with late life bipolar disorder in the community: data from the NNDC registry. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 2015;23(9):977–84. doi:10.1016/j.jagp.2015.01.001.
Gildengers AG, Butters MA, Seligman K, McShea M, Miller MD, Mulsant BH, et al. Cognitive functioning in late-life bipolar disorder. Am J Psychiatry. 2004;161(4):736–8. doi:10.1176/appi.ajp.161.4.736.
Tsai SY, Lee HC, Chen CC, Huang YL. Cognitive impairment in later life in patients with early-onset bipolar disorder. Bipolar Disord. 2007;9(8):868–75. doi:10.1111/j.1399-5618.2007.00498.x.
Samame C, Martino DJ, Strejilevich SA. A quantitative review of neurocognition in euthymic late-life bipolar disorder. Bipolar Disord. 2013;15(6):633–44. doi:10.1111/bdi.12077.
Kessing LV, Nilsson FM. Increased risk of developing dementia in patients with major affective disorders compared to patients with other medical illnesses. J Affect Disord. 2003;73(3):261–9.
Sajatovic M, Blow FC, Ignacio RV. Psychiatric comorbidity in older adults with bipolar disorder. Int J Geriatr Psychiatry. 2006;21(6):582–7. doi:10.1002/gps.1527.
Wu KY, Chang CM, Liang HY, Wu CS, Chia-Hsuan Wu E, Chen CH, et al. Increased risk of developing dementia in patients with bipolar disorder: a nested matched case-control study. Bipolar Disord. 2013;15(7):787–94. doi:10.1111/bdi.12116.
Gildengers AG, Mulsant BH, Begley A, Mazumdar S, Hyams AV, Reynolds Iii CF, et al. The longitudinal course of cognition in older adults with bipolar disorder. Bipolar Disord. 2009;11(7):744–52. doi:10.1111/j.1399-5618.2009.00739.x.
Schouws SN, Comijs HC, Dols A, Beekman AT, Stek ML. Five-year follow-up of cognitive impairment in older adults with bipolar disorder. Bipolar Disord. 2016;18(2):148–54. doi:10.1111/bdi.12374.
Lolich M, Holtzman JN, Rago CM, Vazquez GH. Neuroprogression and cognition in bipolar disorders: a systematic review of cognitive performance in euthymic patients. Vertex. 2015;26(122):265–75.
• Rise IV, Haro JM, Gjervan B. Clinical features, comorbidity, and cognitive impairment in elderly bipolar patients. Neuropsychiatr Dis Treat. 2016;12:1203–13. doi:10.2147/NDT.S100843. This systematic review described clinical characteristics, comorbidities, and cognitive impairment in patients with late-life BD. Cardiovascular and respiratory conditions, type II diabetes, and endocrinological abnormalities were observed as highly prevalent. BD is associated with a high suicide risk. Bipolar elderly had an increased risk of dementia and performed worse on cognitive screening tests compared to age-matched controls across different levels of cognition.
Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disord. 2001;3(4):181–8.
Dols A, Rhebergen D, Beekman A, Kupka R, Sajatovic M, Stek ML. Psychiatric and medical comorbidities: results from a bipolar elderly cohort study. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 2014;22(11):1066–74. doi:10.1016/j.jagp.2013.12.176.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) study. JAMA. 1990;264(19):2511–8.
Sajatovic M, Kessing LV. Bipolar disorder in the elderly. In: Yatham LN, Maj M, editors. Bipolar Disorder: CLinical and Neurobiological Foundations. West Sussex: Wiley-Blackwell; 2010. p. 488.
Yassa R, Nair V, Nastase C, Camille Y, Belzile L. Prevalence of bipolar disorder in a psychogeriatric population. J Affect Disord. 1988;14(3):197–201.
Beyer JL, Kuchibhatla M, Cassidy F, Krishnan KR. Stressful life events in older bipolar patients. Int J Geriatr Psychiatry. 2008;23(12):1271–5. doi:10.1002/gps.2062.
Depp CA, Davis CE, Mittal D, Patterson TL, Jeste DV. Health-related quality of life and functioning of middle-aged and elderly adults with bipolar disorder. J Clin Psychiatry. 2006;67(2):215–21.
Depp CA, Mausbach BT, Eyler LT, Palmer BW, Cain AE, Lebowitz BD, et al. Performance-based and subjective measures of functioning in middle-aged and older adults with bipolar disorder. J Nerv Ment Dis. 2009;197(7):471–5. doi:10.1097/NMD.0b013e3181ab5c9b.
Beyer JL, Kuchibhatla M, Looney C, Engstrom E, Cassidy F, Krishnan KR. Social support in elderly patients with bipolar disorder. Bipolar Disord. 2003;5(1):22–7.
Martire LM, Hinrichsen GA, Morse JQ, Reynolds CF 3rd, Gildengers AG, Mulsant BH, et al. The Mood Disorder Burden Index: a scale for assessing the burden of caregivers to adults with unipolar or bipolar disorder. Psychiatry Res. 2009;168(1):67–77. doi:10.1016/j.psychres.2008.04.010.
• Kendler KS. The clinical features of mania and their representation in modern diagnostic criteria. Psychol Med. 2016:1–17. doi:10.1017/S0033291716003238. Clinical descriptions of mania appearing in 18 textbooks published between 1899 and 1956 were reviewed and compared to the criteria for mania from six modern operationalized diagnostic systems. Twenty-two prominent symptoms and signs were reported by five or more authors. Two symptoms (elevated mood and grandiosity) and four signs (hyperactivity, pressured speech, irritability, and new activities with painful consequences) were reported by every author. A strong relationship was seen between the frequency with which the clinical features was reported and the likelihood of their inclusion in modern diagnostic systems. However, many symptoms and signs including impulsivity, hypersexuality, mood lability, altered moral standards, increased humor, hypergraphia, and a vigorous physical appearance were not included in any modern criteria. Indeed, DSM-5 contains only eight of the historically noted clinical features. We conclude that modern operationalized criteria for mania well reflect symptoms and signs frequently reported by historical experts. This suggests that the clinical construct of mania has been relatively stable in western psychiatry since the turn of the twentieth century. However, many useful clinical features of mania described in these textbooks are missing from these criteria thereby illustrating the limitations of clinical evaluations restricted to the assessment of the only current diagnostic criteria. The disorders we study and treat are considerably richer clinically than are reflected in the DSM criteria which we use to diagnose them .
Kendler KS. The clinical features of mania and their representation in modern diagnostic criteria. Psychol Med. 2017;47(6):1013–29. doi:10.1017/S0033291716003238.
• Machado-Vieira R, Luckenbaugh DA, Ballard ED, Henter ID, Tohen M, Suppes T, et al. Increased activity or energy as a primary criterion for the diagnosis of bipolar mania in DSM-5: findings from the STEP-BD Study. Am J Psychiatry. 2017;174(1):70–76. The authors compared prevalence, clinical characteristics, validators, and outcome in patients meeting the DSM-5 criteria (i.e., DSM-IV criteria plus the DSM-5 criterion of increased activity or energy) and those who did not meet the new DSM-5 criterion (i.e., who only met DSM-IV criteria). All 4360 participants met the DSM-IV criteria for bipolar disorder, and 310 met the DSM-IV criteria for a manic or hypomanic episode. When the new DSM-5 criterion of increased activity or energy was added as a coprimary symptom, the prevalence of mania and hypomania was reduced. Although minor differences were noted in clinical and concurrent validators, no changes were observed in longitudinal outcomes. CONCLUSIONS: The findings confirm that including increased activity or energy as part of DSM-5 criterion A decreases the prevalence of manic and hypomanic episodes but does not affect longitudinal clinical outcomes. doi:10.1176/appi.ajp.2016.15091132.
Kilbourne AM, Cornelius JR, Han X, Pincus HA, Shad M, Salloum I, et al. Burden of general medical conditions among individuals with bipolar disorder. Bipolar Disord. 2004;6(5):368–73. doi:10.1111/j.1399-5618.2004.00138.x.
Perron BE, Howard MO, Nienhuis JK, Bauer MS, Woodward AT, Kilbourne AM. Prevalence and burden of general medical conditions among adults with bipolar I disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2009;70(10):1407–15. doi:10.4088/JCP.08m04586yel.
Lehmann SW, Rabins PV. Factors related to hospitalization in elderly manic patients with early and late-onset bipolar disorder. Int J Geriatr Psychiatry. 2006;21(11):1060–4. doi:10.1002/gps.1607.
Krauthammer C, Klerman GL. Secondary mania: manic syndromes associated with antecedent physical illness or drugs. Arch Gen Psychiatry. 1978;35(11):1333–9.
Van Gerpen MW, Johnson JE, Winstead DK. Mania in the geriatric patient population: a review of the literature. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 1999;7(3):188–202.
Brooks JO 3rd, Hoblyn JC. Secondary mania in older adults. Am J Psychiatry. 2005;162(11):2033–8. doi:10.1176/appi.ajp.162.11.2033.
Puryear LJ, Kunik ME, Workman R Jr. Tolerability of divalproex sodium in elderly psychiatric patients with mixed diagnoses. J Geriatr Psychiatry Neurol. 1995;8(4):234–7. doi:10.1177/089198879500800407.
Woodward M, Jacova C, Black SE, Kertesz A, Mackenzie IR, Feldman H, et al. Differentiating the frontal variant of Alzheimer’s disease. Int J Geriatr Psychiatry. 2010;25(7):732–8. doi:10.1002/gps.2415.
Staekenborg SS, Su T, van Straaten EC, Lane R, Scheltens P, Barkhof F, et al. Behavioural and psychological symptoms in vascular dementia; differences between small- and large-vessel disease. J Neurol Neurosurg Psychiatry. 2010;81(5):547–51. doi:10.1136/jnnp.2009.187500.
Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain J Neurol. 2011;134(Pt 9):2456–77. doi:10.1093/brain/awr179.
Roman GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC, Garcia JH, et al. Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology. 1993;43(2):250–60.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement J Alzheimers Assoc. 2011;7(3):263–9. doi:10.1016/j.jalz.2011.03.005.
• Sajatovic M, Dines P, Fuentes-Casiano E, Athey M, Cassidy KA, Sams J, et al. Asenapine in the treatment of older adults with bipolar disorder. Int J Geriatr Psychiatry. 2015;30(7):710–9. doi:10.1002/gps.4213. This was a 12-week open-label trial of asenapine in the treatment for older adults with bipolar disorder ( n = 15). The study found improvements in a variety of psychiatric symptom scales, including the brief psychiatric rating scale, the clinical global impression depression and mania subscales .
Vorspan F, Bertoux M, Brichant-Petitjean C, Dubois B, Lepine JP. Relapsing-remitting behavioural variant of frontotemporal dementia in a bipolar patient. Funct Neurol. 2012;27(3):193–6.
Kerstein AH, Schroeder RW, Baade LE, Lincoln J, Khan AY. Frontotemporal dementia mimicking bipolar disorder. J Psychiatr Pract. 2013;19(6):498–500. doi:10.1097/01.pra.0000438190.04786.16.
Cerami C, Marcone A, Galimberti D, Villa C, Scarpini E, Cappa SF. From genotype to phenotype: two cases of genetic frontotemporal lobar degeneration with premorbid bipolar disorder. J Alzheimers Dis. 2011;27(4):791–7. doi:10.3233/JAD-2011-110788.
Pavlovic A, Marley J, Sivakumar V. Development of frontotemporal dementia in a case of bipolar affective disorder: is there a link? BMJ Case Rep. 2011; doi:10.1136/bcr.09.2010.3303.
Lois G, Linke J, Wessa M. Altered functional connectivity between emotional and cognitive resting state networks in euthymic bipolar I disorder patients. PLoS One. 2014;9(10):e107829. doi:10.1371/journal.pone.0107829.
Rashid B, Damaraju E, Pearlson GD, Calhoun VD. Dynamic connectivity states estimated from resting fMRI identify differences among schizophrenia, bipolar disorder, and healthy control subjects. Front Hum Neurosci. 2014;8:897. doi:10.3389/fnhum.2014.00897.
Zhou J, Seeley WW. Network dysfunction in Alzheimer’s disease and frontotemporal dementia: implications for psychiatry. Biol Psychiatry. 2014;75(7):565–73. doi:10.1016/j.biopsych.2014.01.020.
Khan BK, Yokoyama JS, Takada LT, Sha SJ, Rutherford NJ, Fong JC, et al. Atypical, slowly progressive behavioural variant frontotemporal dementia associated with C9ORF72 hexanucleotide expansion. J Neurol Neurosurg Psychiatry. 2012;83(4):358–64. doi:10.1136/jnnp-2011-301883.
Meisler MH, Grant AE, Jones JM, Lenk GM, He F, Todd PK, et al. C9ORF72 expansion in a family with bipolar disorder. Bipolar Disord. 2013;15(3):326–32. doi:10.1111/bdi.12063.
Floris G, Di Stefano F, Pisanu C, Chillotti C, Murru MR, Congiu D, et al. C9ORF72 repeat expansion and bipolar disorder—is there a link? No mutation detected in a Sardinian cohort of patients with bipolar disorder. Bipolar Disord. 2014;16(6):667–8. doi:10.1111/bdi.12210.
Floris G, Borghero G, Cannas A, Stefano FD, Murru MR, Corongiu D, et al. Bipolar affective disorder preceding frontotemporal dementia in a patient with C9ORF72 mutation: is there a genetic link between these two disorders? J Neurol. 2013;260(4):1155–7. doi:10.1007/s00415-013-6833-2.
Davies RR, Kipps CM, Mitchell J, Kril JJ, Halliday GM, Hodges JR. Progression in frontotemporal dementia: identifying a benign behavioral variant by magnetic resonance imaging. Arch Neurol. 2006;63(11):1627–31. doi:10.1001/archneur.63.11.1627.
Kipps CM, Hodges JR, Hornberger M. Nonprogressive behavioural frontotemporal dementia: recent developments and clinical implications of the ‘bvFTD phenocopy syndrome’. Curr Opin Neurol. 2010;23(6):628–32. doi:10.1097/WCO.0b013e3283404309.
• Dols A, Krudop W, Moller C, Shulman K, Sajatovic M, Pijnenburg YA. Late life bipolar disorder evolving into frontotemporal dementia mimic. Neuropsychiatr Dis Treat. 2016;12:2207–12. doi:10.2147/NDT.S99229. From our neuropsychiatric outpatient clinic, we describe four cases with bipolar disorder gradually developing a clinical syndrome, including apathy, disinhibition, loss of empathy, stereotypical behavior, and compulsiveness, fulfilling the criteria for possible behavioral variant frontotemporal dementia. All cases were diagnosed with bipolar 1 disorder at least 10 years before the onset of the current symptoms, which was not due to recent mood episodes or switches of medication. In all cases, 3–7 years of follow-up yielded no progression. Repeated neuroimaging was within normal limits. Cerebrospinal fluid biomarker studies were not supportive of underlying neurodegenerative pathology. C9orf72 mutation status was negative in all cases. Symptoms fitting the criteria for possible behavioral variant frontotemporal dementia may be present in end stage of bipolar disorder. An alternative neurodegenerative nature seems unlikely based on repeated normal neuroimaging and the absence of clinical progression. Functional involvement of the frontal-subcortical networks might play a role.
• Mendez MF. Mania in neurologic disorders. Curr Psychiatry Rep. 2000;2(5):440–5. Neurologic disorders can produce “secondary” mania. Clinicians must distinguish secondary mania from primary, idiopathic manic-depressive illness (MBI). In addition to medical and drug-induced causes of secondary mania, neurologic causes usually develop in older patients who may lack a strong family history of MDI. Neurologic causes of mania include focal strokes in the right basotemporal or inferofrontal region, strokes or tumors in the perihypothalamic region, Huntington’s disease and other movement disorders, multiple sclerosis and other white matter diseases, head trauma, infections such as neurosyphilis and Creutzfeldt-Jakob disease, and frontotemporal dementia. Patients with new-onset mania require an evaluation that includes a thorough history, a neurologic examination, neuroimaging, and other selected tests. The management of patients with neurologic mania involves correcting the underlying disorder when possible and the judicious use of drugs such as anticonvulsant medications.
Robinson RG, Boston JD, Starkstein SE, Price TR. Comparison of mania and depression after brain injury: causal factors. Am J Psychiatry. 1988;145(2):172–8. doi:10.1176/ajp.145.2.172.
Jorge RE, Robinson RG, Starkstein SE, Arndt SV, Forrester AW, Geisler FH. Secondary mania following traumatic brain injury. Am J Psychiatry. 1993;150(6):916–21. doi:10.1176/ajp.150.6.916.
Braun CM, Larocque C, Daigneault S, Montour-Proulx I. Mania, pseudomania, depression, and pseudodepression resulting from focal unilateral cortical lesions. Neuropsychiatry Neuropsychol Behav Neurol. 1999;12(1):35–51.
Steffens DC, Krishnan KR. Structural neuroimaging and mood disorders: recent findings, implications for classification, and future directions. Biol Psychiatry. 1998;43(10):705–12.
Abou-Saleh MT, Coppen A. Subjective side-effects of amitriptyline and lithium in affective disorders. Br J Psychiatry J Ment Sci. 1983;142:391–7.
Chen ST, Altshuler LL, Melnyk KA, Erhart SM, Miller E, Mintz J. Efficacy of lithium vs. valproate in the treatment of mania in the elderly: a retrospective study. J Clin Psychiatry. 1999;60(3):181–6.
Goldberg JF, Sacks MH, Kocsis JH. Low-dose lithium augmentation of divalproex in geriatric mania. J Clin Psychiatry. 2000;61(4):304.
Murray N, Hopwood S, Balfour DJ, Ogston S, Hewick DS. The influence of age on lithium efficacy and side-effects in out-patients. Psychol Med. 1983;13(1):53–60.
Schaffer CB, Garvey M. Use of lithium in acutely manic elderly patients. Clin Gerontol J Aging Ment Health. 1984;3(1):58–60. doi:10.1300/J018v03n01_06.
Van der Velde C. Effectiveness of lithium carbonate in the treatment of manic-depressive illness. Am J Psychiatry. 1970;127(3):345–51.
Kando JC, Tohen M, Castillo J, Zarate CA Jr. The use of valproate in an elderly population with affective symptoms. J Clin Psychiatry. 1996;57(6):238–40.
McFarland BH, Miller MR, Straumfjord AA. Valproate use in the older manic patient. J Clin Psychiatry. 1990;51(11):479–81.
Niedermier JA, Nasrallah HA. Clinical correlates of response to valproate in geriatric inpatients. Ann Clin Psychiatry Off J Am Acad Clin Psychiatr. 1998;10(4):165–8.
Noaghiul S, Narayan M, Nelson JC. Divalproex treatment of mania in elderly patients. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 1998;6(3):257–62.
Sharma V, Persad E, Mazmanian D, Karunaratne K. Treatment of rapid cycling bipolar disorder with combination therapy of valproate and lithium. Can J Psychiatry. 1993;38(2):137–9.
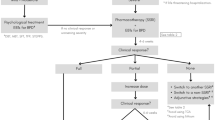
Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Beaulieu S, Alda M, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2013. Bipolar Disord. 2013;15(1):1–44. doi:10.1111/bdi.12025.
Sajatovic M, Calabrese JR, Mullen J. Quetiapine for the treatment of bipolar mania in older adults. Bipolar Disord. 2008;10(6):662–71. doi:10.1111/j.1399-5618.2008.00614.x.
Sajatovic M, Coconcea N, Ignacio RV, Blow FC, Hays RW, Cassidy KA, et al. Aripiprazole therapy in 20 older adults with bipolar disorder: a 12-week, open-label trial. J Clin Psychiatry. 2008;69(1):41–6.
Baruch Y, Tadger S, Plopski I, Barak Y. Asenapine for elderly bipolar manic patients. J Affect Disord. 2013;145(1):130–2. doi:10.1016/j.jad.2012.05.027.
Madhusoodanan S, Brenner R, Araujo L, Abaza A. Efficacy of risperidone treatment for psychoses associated with schizophrenia, schizoaffective disorder, bipolar disorder, or senile dementia in 11 geriatric patients: a case series. J Clin Psychiatry. 1995;56(11):514–8.
Shulman R, Singh A, Shulman K. Treatment of elderly institutionalized bipolar patients with clozapine. Psychopharmacol Bull. 1997;33(1):113–8.
Sethi MA, Mehta R, Devanand DP. Gabapentin in geriatric mania. J Geriatr Psychiatry Neurol. 2003;16(2):117–20. doi:10.1177/0891988703016002010.
Cullen M, Mitchell P, Brodaty H, Boyce P, Parker G, Hickie I, et al. Carbamazepine for treatment-resistant melancholia. J Clin Psychiatry. 1991;52(11):472–6.
• Young RC. Lithium and divalproex in the treatment of mania in older patients with bipoalr disorder: a randomized clinical trial. Am Soc Clin Psychopharmacol. 2015; Miami, Florida. This was a large 3-week RCT of valproate vs. lithium for mania and hypomania in older-age bipolar disorder patients ( n > 200). This is the only RCT for older age bipolar disorder. The authors found both lithium and valproate effective in acute mania/hypomania, with similar short-term tolerability overall American Journal Psychiatry (In Press).
Bartels SJ, Pratt SI, Mueser KT, Forester BP, Wolfe R, Cather C, et al. Long-term outcomes of a randomized trial of integrated skills training and preventive healthcare for older adults with serious mental illness. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 2014;22(11):1251–61. doi:10.1016/j.jagp.2013.04.013.
Sajatovic M, Forester BP, Gildengers A, Mulsant BH. Aging changes and medical complexity in late-life bipolar disorder: emerging research findings that may help advance care. Neuropsychiatry (London). 2013;3(6):621–33. doi:10.2217/npy.13.78.
Dols A, Sienaert P, van Gerven H, Schouws S, Stevens A, Kupka R, et al. The prevalence and management of side effects of lithium and anticonvulsants as mood stabilizers in bipolar disorder from a clinical perspective: a review. Int Clin Psychopharmacol. 2013;28(6):287–96. doi:10.1097/YIC.0b013e32836435e2.
Ng F, Mammen OK, Wilting I, Sachs GS, Ferrier IN, Cassidy F, et al. The International Society for Bipolar Disorders (ISBD) consensus guidelines for the safety monitoring of bipolar disorder treatments. Bipolar Disord. 2009;11(6):559–95. doi:10.1111/j.1399-5618.2009.00737.x.
Parikh SV, Zaretsky A, Beaulieu S, Yatham LN, Young LT, Patelis-Siotis I, et al. A randomized controlled trial of psychoeducation or cognitive-behavioral therapy in bipolar disorder: a Canadian Network for Mood and Anxiety treatments (CANMAT) study [CME]. J Clin Psychiatry. 2012;73(6):803–10. doi:10.4088/JCP.11m07343.
Kilbourne AM, Barbaresso MM, Lai Z, Nord KM, Bramlet M, Goodrich DE, et al. Improving physical health in patients with chronic mental disorders: twelve-month results from a randomized controlled collaborative care trial. J Clin Psychiatry. 2017;78(1):129–37. doi:10.4088/JCP.15m10301.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Peijun Chen, Annemiek Dols, and Soham Rej each declare no potential conflicts of interest.
Martha Sajatovic has received grant support from Alkermes, Janssen, Pfizer, and Merck and royalties from Springer Press, Johns Hopkins University Press, and Oxford Press and served as consultant for Bracket, Pfizer, Otsuka, Sunovion, Neurocrine, Supernus, and Health Analytics.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Geriatric Disorders
Rights and permissions
About this article
Cite this article
Chen, P., Dols, A., Rej, S. et al. Update on the Epidemiology, Diagnosis, and Treatment of Mania in Older-Age Bipolar Disorder. Curr Psychiatry Rep 19, 46 (2017). https://doi.org/10.1007/s11920-017-0804-8
Published:
DOI: https://doi.org/10.1007/s11920-017-0804-8