Abstract
Purpose of Review
The aim of this review is to characterize headache as a vaccine adverse event (VAE) in clinical trials.
Recent Findings
Of the recent phase III vaccine RCTs (non-COVID-19), 53 studies reported on headache (13 infectious agents). The median rate (interquartile range) of headache was 15.6% (IQR: 9.6–37.6%). Of these, 24.5% of the RCTs reported headache greater in the vaccine group compared to the placebo/control group. In the herpes zoster vaccination trials, headache was more common in all active groups: median rate 33.9% (IQR: 29.7–40.5%) as compared to placebo: median rate 17.7% (IQR: 15.4–23.8%). Influenza and HPV vaccination trials were the 2nd and 3rd most common to have headache as a VAE. Of the 6 widely distributed COVID-19 vaccinations, median rate of post-vaccination headache was 39% (IQR: 28–50%).
Summary
Headache is a common VAE in vaccine trials. Standardized grading methods, predictors of persistence, and treatment regimens are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vaccine programs are one of the most effective public health measures to control the threat of communicable diseases. Phase III clinical trials are performed to study the effectiveness and safety of novel vaccines, with comparison to the gold standard, an established vaccine, or placebo. Vaccine adverse events (VAEs) are important to evaluate. In one meta-analysis, vaccine safety was among the top reasons for COVID-19 vaccination hesitancy in healthcare workers [1]. In post-licensure surveillance, headache is one of the most reported VAEs, which is especially relevant given the high burden of headache disorders in the general population [2].
The aim is to characterize headache as a VAE and summarize the quality of reporting in randomized controlled trials (RCTs). There is focus on COVID-19 vaccinations, due to the novelty of mRNA-based technologies and nanovaccines. As post-vaccination headache is not defined in the International Classification of Headache Disorders (ICHD-3), we also characterize a case presentation, possible mechanisms, and clinical relevance.
Methods
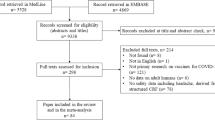
We conducted a search of RCTs involving vaccines from November 30, 2018 through November 30, 2021 which resulted in 1501 articles (PubMed). From these, 1058 were randomized controlled trials (RCTs), of which 211 were phase III RCTs. Of these 211 phase III RCTs, articles were excluded if they pertained to experimental tumor vaccines or mentioned vaccines but did not test safety and immunogenicity. According to these criteria, 185 studies were obtained. We included COVID-19 RCTs but limited our evaluation to those with FDA approval within the USA. Medians, 25th, and 75th percentiles describing rate of vaccination headache and rate of headache due to placebo were calculated.
We reviewed 11 RCTs published within the last 2 years of six widely distributed COVID-19 vaccinations.
Headache as an Adverse Event in Vaccination Trials
In the majority of the 148 RCTs (non-COVID-19) reviewed, data on headache as a VAE was either not reported or nonspecific. Ten (6.8%) of the studies reported only the most and least common VAE without mention of all VAEs that occurred.
Of the 148 reviewed studies, headache as a VAE was measured in 56. These 56 studies included testing of vaccines against 13 different infectious agents in total. Fifty-three of the studies reported the headache data (Table 1), while three did not report. Of the 53 which reported headache data, 34 RCTs had active comparison groups while the remaining 19 were placebo controlled.
Measurement and Report of Headache Occurrence and Frequency
Of these studies, about one fourth (40/148; 27.0%) reported headache as an individual VAE. Less (13/148; 8.8%) reported headache as combined with other common VAEs (including fatigue, fever, and myalgias): These were defined together as “solicited VAEs,” “solicited systemic VAEs,” “systemic events,” “solicited general symptoms,” “general symptoms,” “solicited systemic reactions,” and “systemic reaction categories.” Often, the specific frequency of headache was recorded in supplemental tables and materials (Table 1).
Measurement and Report of Headache Severity
Of the 53 studies reporting headache, 16 measured the intensity of headache as a grading scale. One study defined four grades (the most severe headache outcome as “grade 4”) [27], while all others defined three grades (the most severe and debilitating outcome as “grade 3”). Not all grading scale data was reported: One study reported grades 1, 2, and 4 but did not report grade 3 [27], and 14 studies reported grade 3 only (Table 1).
Additionally, two studies specified headache severity as “mild,” “moderate,” or “severe,” rather than using a grading scale [16, 49]. Three studies specified only when headaches were considered “severe” [13, 14, 34].
Within the RCTs with active comparison groups, 9 described headache using a grading severity system, 3 described headache using severity measures, and 22 did not specify grade/severity. Within the 19 placebo-controlled RCTs, 7 described headache using a grading system, 2 provided headache severity measures, and 10 did not specify headache grade/severity.
Measurement and Report of Headache Severity in COVID-19 Vaccination Studies
Because of significant interest due to the COVID-19 pandemic, we evaluated the FDA approved COVID-19 vaccinations separately. Among the six COVID-19 vaccine RCTs reviewed, all but one, CoronaVac, reported data on headache severity. However, the five trials that do report severity also lack consistency. The RCT involving COVID-19 vaccine BNT162b2 classified headache severity outcomes as “any,” “mild,” “moderate,” “severe,” and grade 4 among the “5 to 11,” “12 to 15,” “16 to 55,” and “55 and greater” age groups [56]. The RCT involving vaccine mRNA-1273 categorized headache severity in grades 1–4 and “any” among the “18 to 65” and “65 and greater” age groups [57, 58]. The RCT involving vaccine Ad26 CoV2.S only reported headache severity with grades 3 and 4 and these were assessed in the “18 to 59” and “59 and greater” age groups [59]. This study did not report data on headaches with a grade severity of 1 or 2. The RCT involving ChAdOx1nCoV-19/ADZ1222 vaccine also defined headache severity as “any,” “mild,” “moderate,” and “severe” but indicated whether headaches led to hospitalization across the “18 to 55,” “56–69,”, and “69 and greater” age groups [60]. Similarly, to the mRNA-1273 vaccine, the RCT involving NVX-CoV2373 also defined headache severity as “any” and grades 1–4, but these were only reported in the “18 to 84” age group [61, 62]. These severity definitions were assessed within 7 days of each vaccination dose except for the Ad26 CoV2.S vaccine RCT, which only administered one dose. All six studies reported headache as an individual VAE and were considered one of the “systemic” VAEs (Table 2).
Results
Findings on Headache Reported Post-Vaccination
Of the 148 (non-COVID-19) studies reviewed, the top five infectious agents which measured and reported headache as a VAE included herpes zoster, influenza, HPV, meningococcal, and pneumococcal. Of those using placebo as control, 8 of 13 (61.5%) herpes zoster vaccine trials, 11 of 27 (40.7%) of influenza vaccine trials, and 5 of 16 (31.4%) of HPV vaccine trials reported headache as a VAE. Of those using active control, 10 of 26 (38.5%) meningococcal vaccine trials and 3 of 10 (30.0%) of pneumococcal conjugate vaccine trials reported headache as a VAE.
Over a third (38.5%; 19 /53) of RCTs reporting headache were placebo controlled. In 13 of these, headache was more common after vaccination than placebo. These included studies of vaccines against herpes zoster, influenza, varicella, rabies, and c. difficile. In the remaining six, headache was more common in the placebo than vaccine group. These included studies of vaccines against influenza, HPV, diphtheria, HIV, and schistosomiasis (Table 1). In one study, more than one vaccine group was compared to a single placebo group [3]. Headache was greater in the quadrivalent virus-like particle vaccine group in adults 18–64 than in the placebo group. However, headache was greater in the placebo group when compared to the quadrivalent virus-like particle vaccine with adults 65 plus and quadrivalent inactivated vaccine of both age groups [3]. In another, one vaccine group was compared to two different control groups [12]. Headache was greater in the vaccine group than in the control 2 trivalent inactivated subunit group but was less than headache in the control 1 trivalent inactivated subunit group.
Of the herpes zoster vaccine trials, five of eight found post-vaccination headache to be more common in the vaccine group compared to placebo: 33.5% (active) vs. 18.6% (placebo) [17]; 74.1% (active) vs. 48.9% (placebo) [18]; 40% (active) vs. 38% (placebo) [19]; 41.8% (active) vs.14.1% (placebo), 34.3% (active) vs. 15.8% (placebo), 30.1% (active) vs. 19.0% (placebo), 28.6% (active) vs. 16.7% (placebo) [20]; 6.51% (active) vs. 3.04% (placebo) [24] while the others found no significant difference. Of the influenza vaccine trials, 27.3% (3/11): 20.1% (active) vs. 19.1% (placebo) [3]; 14.1% (active) vs. 12.3% (placebo) [12]; and 19.2% (active) vs. 6.3% (placebo) [13] found headache to be more common in the vaccine group and 9.1% (1/11): 16.4% (active) vs. 19.6% (placebo) [8] found headache to be more common in the placebo group. Of the HPV vaccine trials, 20% (1/5):14.5% (active) vs. 12.9% (placebo) [27] found headache more common in the vaccine group and 20% (1/5): 0.4% (active) vs. 1.3% (placebo) [25] found headache more common in the placebo group. Overall, median rate of headache in non-COVID-19 vaccines was 15.6% (IQR: 6.4–30.6%) (active) vs. 15.7% (IQR: 5.4–19.1%) (placebo) (Table 1).
Headache as an Adverse Event Following COVID-19 Vaccination Studies
The coronavirus disease (COVID-19) pandemic resulting from infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) has affected and continues to affect hundreds of millions of people. In response, multiple vaccines were developed, of which clinical trial and prospective data have revealed headache to be one of the most commonly reported VAEs (Table 2). Headache was the third most common symptom after vaccination [68].
The initial messenger RNA-based COVID-19 vaccines were the first of their approach to be approved [56, 57]. For these vaccines, the majority of headache events were rated as “mild” or “grade 1” across doses and age groups and systemic reactogenicity (including headache) was more common and severe after the second dose than after the first dose and among younger than older recipients [56, 57, 61]. The median rate of headache post-vaccination for mRNA COVID-19 vaccines dose one, two, and combined was 30.3% (IQR: 4.7–40.3%) (active) vs. 26.6% (IQR: 20.5–32.5%) (placebo), 49% (IQR: 40.8–60%) (active) vs. 21.4% (IQR: 18–24.3%) (placebo), and 40.5% (IQR: 27.3–52.6%) (active) vs. 24.1% (IQR: 18.5–26.2%) (placebo) respectively. When compared, median rate of headache due to placebo was lower by 3.7%, 27.6%, and 16.4%. In the BNT162b2 study, headache was one of only two systemic events reported as severe after either dose in at least 2% of recipients [57].
Data from the mRNA-1273 study reveal headache to have a mean duration of 2.1 days after the first dose and 2.3 days after the second dose, with only 4.8% persisting beyond 7 days [57]. Similarly, mean duration of headache was 1.6 days after the first and 2.0 days after the second dose in the NVX-CoV2373; no headache extended past 7 days after the second dose [61].
The median rate of headache vaccination of vaccines using a recombinant nanoparticle was calculated for dose 1, 23% (active) vs. 30% (placebo), dose 2, 46% (active) vs. 29% (placebo), and combined, 34.5% (active) vs. 29.5% (placebo). When compared, median rate of headache due to placebo was 7% higher for dose one, yet was 17% lower for dose two, and 5% lower for both doses combined [61, 62].
The median rate of headache vaccination for adenovirus vectored vaccines [59, 60] was calculated for dose 1, 45.5% (IQR: 40.5–53.8%), dose 2, 31% (IQR: 25.5–32.5%), and combined, 38.9% (IQR: 32.5–45.5%). No rate of headache due to placebo was reported for comparison.
For the COVID-19 vaccines reviewed (Table 2), overall median rate of headache vaccination and IQR was calculated among first, second, and both doses combined. This resulted in medians: 38.9% (IQR: 24.9–46%) (active) vs. 29% (IQR: 21.7–31.9%) (placebo), 42.5% (IQR: 31.8–50.3%) (active) vs. 24.1% (IQR: 18.2–24.9%) (placebo), and 39% (IQR: 28–50%) (active) vs. 24.3% (IQR: 18.8–29%) (placebo). This demonstrates a 10%, 18.4%, and 14.7% increase in headache post-vaccine when compared to placebo.
VAE Case Description: Headache Associated with COVID-19 Vaccination
A 23-year-old woman presented for follow up of migraine with aura and menstrual migraine; she had been diagnosed 3 years prior and had comorbid anxiety and irritable bowel syndrome. She had reported two migraine attacks in the 6 months prior to COVID-19 vaccination. Following vaccination, she experienced increased severity and frequency. Of note, she did have a history of chronic migraine (up to 22 headache days per month) in years prior.
The patient received the first dose of the BNT162b2 mRNA vaccine on January 14, 2021. Two days after, she experienced a series of severe migraine attacks for with pain intensity of 7–10 out of 10 on a 0–10 numeric rating scale. The attacks were lasting 7 to 8 h with reoccurrence, for 1.5 weeks. The migraine attacks alternated between unilateral and bilateral locations and were throbbing and sharp in pain quality. Symptoms occurring with her post-vaccination headache included more severe photophobia and nausea and vomiting compared to baseline, as well as her typical phonophobia, sensitivity to movement, lightheadedness, confusion, and difficulty thinking and concentrating. She reported an increased frequency of visual auras consisting of flashing lights with about half of these migraine attacks. The visual auras lasted about 4 h and were prolonged compared to her usual episodes of 45 min duration. Numbness with tingling also occurred in the face, arms, and sometimes legs during her attacks. In the past, she had experienced word substitution and weakness but had not had these symptoms for 6 years.
She treated her migraine attacks with rizatriptan, metoclopramide, and NSAIDs daily; however, they were treatment resistant. To alleviate the pain, the patient stayed in a dark room but had difficulty falling asleep. Due to the constant pain, she was not able to work or socialize. After 1.5 weeks, the migraine attacks subsided.
The patient received dose 2 of the vaccine three weeks later. A few hours after the vaccine, she experienced a mild headache in the center frontal region of the head, with pressure-like pain that lasted 2 h in duration and did not interrupt her daily activities. She did not have any associated symptoms and did not require treatment. About 15 h following the second dose, she experienced mild chills, a low-grade fever, and mild myalgias which resolved 5 h later. About 10 days after receiving dose 2, the patient reported no new symptoms or recurrences in headaches or migraine attacks.
In clinical practice, the risk of is getting a headache after vaccination is a commonly asked question. A recent systematic review and meta-analysis of 84 papers concluded that COVID-19 vaccines are associated with a two-fold risk of developing headache within 7 days from injection (compared with placebo) [68].
Similar trends have been shown in real-world, cross-sectional survey-based studies conducted after vaccine approval: “Headache/fatigue” was the most common systemic side effect (48.1% in mRNA-based vaccines and 74.4% in viral vector-based vaccines) in one [69] and the third most common (45.6%) behind fatigue in another [70]. Data according to the database of Adverse Drug Reactions in Italy has been compared to epidemiologic data according to the Global Health Data Exchange and revealed that the cumulative rate of headache/migraine episodes after receiving all COVID-19 vaccines was 2.25-fold higher than the daily frequency of headache disorders [71].
Discussion
Pathophysiology of Headache Post-Vaccination
Headache secondary to vaccination is likely due to systemic reactogenicity, the physical and systemic manifestations of the immune response to the vaccine. Headache following vaccination is proposed to occur via prostaglandin E production, release of cytokines such as IL-6, and C-reactive protein [72] which could lead to activation of trigeminal nociceptors. In a similar fashion, immune mediators and products of inflammation could exacerbate symptoms and induce headache persistence in patients with primary headache disorder. Taken together, individuals with migraine have been shown to have clinical evidence of peripheral and central sensitization of the trigeminovascular system, in addition to enhanced sensitivity to inflammatory stimuli [73, 74]. Although inflammation is debated as a mechanism of migraine, our case suggests that the immune response to vaccination may induce cortical spreading depression in individuals with a predisposition to migraine aura. The association between headache, other non-headache symptoms of reactogenicity such as fever, fatigue, and malaise, and immunogenicity should be evaluated in future studies.
Characteristics of Post-Vaccination Headache
Prior to the emergence of COVID-19 vaccinations, specific characteristics of headache following vaccination were not systematically examined. Still, HPV vaccination had been identified as a trigger for new daily persistent headache (NDPH) [75]. In our clinical practice, persistent and unremitting headache of at least 3-month duration, consistent with NDPH following vaccination has also been seen in rare circumstances.
An understanding of the characteristics and risk factors related to post-vaccination headache has been further elucidated with recent investigations focused on COVID-19 vaccination. Three questionnaire-based studies have revealed similar timelines with mean intervals of 1.8 ± 3.5 days [76], 18.0 ± 27.0 h [77], and 14.5 ± 21.6 h [78] following vaccination. The mean duration of the attacks has been reported as 14.2 ± 21.3 h [77], 16.3 ± 30.4 h [78], and majority less than 3 days [76]. There is one published case report of status migrainosus lasting 11 days following receipt of vaccination in a patient with history of migraine [79], and status migrainosus following vaccine has also been seen in our clinical practice. According to a recent systematic review and meta-analysis, post-vaccination headache tends to develop within 24-h from injection and usually resolves in less than 24 h [68].
The characteristics of headache after vaccination included a majority with bilateral location [76,77,78] and often at the forehead and temples [77, 78]. Commonly described pain qualities included pressing, throbbing, and dull [76,77,78]. Pain intensity was reported most often as moderate (46.2%) or severe (32.1%) in one study [77] and most often as severe (38.7%) or moderate (35.2%) in another [78]. In studies of COVID-19 vaccine, migraine-like features were present in one third of the cases (pulsating quality, phonophobia, and photophobia), and in 40–60% of the cases aggravation with activity was observed [68]. Interestingly, in a cohort of individuals with prior diagnosis of migraine, over half perceived the post-vaccination headache attacks as “different” from those usually experienced; this included higher pain intensity, longer duration, and reduced responsiveness to usually effective painkillers [80].
Of note, post-vaccination headache was found to be less severe and shorter than COVID-19-related headache [76]. There is one case reporting transient unilateral hemiparesis, sensory deficit, and visual phenomenon followed by headache and lasting 5 days without evidence of cerebral insult on brain imaging which was ultimately attributed to migraine pathology with cortical spreading depression [81]. Another report describes a case of new-onset visual aura phenomenon without headache, although this occurred 127 days after injection; magnetic resonance imaging (MRI) of brain and intracranial vessel imaging were normal [82]. There is one series of 8 patients who experienced lateralized sensory deficits, motor deficits, or both, of 2–14 day duration following CoronaVac vaccination; a history of migraine, female predominance, and abnormal functional brain imaging without structural changes was found and suggestive of migraine aura as pathophysiology [83]. The incidence of aura symptoms related to post-vaccination headache remains unclear at this time.
Risk Factors for Post-Vaccination Headache
In a web-based questionnaire study, potential risk factors identified for development of headache included female sex, pre-existing primary headaches (including migraine and tension-type), thyroid disorders, headache during COVID-19, and headache related to the influenza vaccine [76]. However, our review of recent influenza vaccine RCTs includes reported results of trivalent inactivated vaccine and quadrivalent inactivated vaccine, which was mixed.
Another questionnaire-based study also found headache to be more commonly reported in participants who had a prior history of migraine or non-migraine headache compared with healthy controls [84]. Patients who reported headache were more likely to report other systemic VAEs including fever, chills, fatigue, myalgias, joint pain, and nausea or vomiting [76,77,78].
Other Secondary Etiologies
As in the evaluation of all patients presenting with headache complaint, other secondary causes for a post-vaccination headache must be thoroughly considered. Headache was the most common presenting symptom of cerebral venous sinus thrombosis (CVST) following SARS-CoV-2 vaccination, a very rare but severe and potentially fatal complication [85].
There is accumulating evidence supporting an association between (CVST) and adenovirus vector-based vaccines against SARS-CoV-2 (including ChAdOx1 nCov-19 and Ad26.COV2.S); although, one cohort study found no significant association [86]. Development of CVST following vaccination may be mediated by the development of thrombosis and thrombocytopenia syndrome (TTS); one cohort study found that over two thirds of patients who developed CVST within 28 days of SARS-CoV-2 met diagnostic criteria for TTS [87]. A meta-analysis revealed that these thrombotic complications tended to affect predominantly women (69%; 95% CI 60–77%) under age 45, even in the absence of prothrombotic risk factors [88]. Headache related to CVST tended to be delayed compared to the time interval observed in the vaccine safety studies: Studies found the development of CVST-related headache at mean intervals of 8 days [89] and 10 days (within 2 weeks) [88] after exposure.
Suspicion for such an etiology is critical as the pooled mortality rate of TTS-associated CVST was 38% (95% CI 27–49%) [88]. Healthcare providers should be familiar with “red flags” in clinical presentations and the diagnostic criteria for this potential complication and other secondary etiologies (Fig. 1). When suspected, early diagnosis including brain imaging and prompt initiation of treatment can result in more favorable neurologic outcomes.
Comparison of headache as an adverse event to common COVID-19 vaccinations in clinical trials. Legend: Headache according to grade (scoring) following vaccination with COVID-19 vaccination for middle-aged range of patients (age 16–55 years for A BNT162b2, age 18–65 years for B mRNA-1273, and age 18–55 years for C ChAdOx1 nCoV-19). The results of Ad26.COV2.S and CoronaVac (due to missing data), in addition to NVX-CoV2373 (recent emergency use authorization only), are not shown here. There were no reports of headache scored as grade 4. A Mild, does not interfere with activity; moderate, some interference with activity; severe, prevents daily activity; grade 4, emergency room visit or hospitalization for severe headache. B Grade 1, does not interfere with daily activity; grade 2, repeated use of OTC pain reliever > 24 h to some interference with activity; grade 3, any use of prescription pain reliever or prevents daily activity; grade 4, requires emergency room visit or hospitalization. C Grade 1 (mild), symptoms causing no or minimal interference with usual social and functional activities (minor headache not requiring medication); grade 2 (moderate), symptoms causing greater than minimal interference with usual social and functional activities (bad headache but able to do most activities with medication); grade 3 (severe), symptoms cause inability to perform usual social and functional activities (severe headache requiring medication and unable to do normal activities during the day); grade 4, symptoms causing inability to perform basic self-care functions OR hospitalization indicated OR headache with significant impairment of alertness or other neurologic function (emergency department or hospital admission required)
Nocebo Effects of Vaccination Trials
The frequency of headache as a VAE in vaccination trials may be associated with several additional factors, including nocebo effects inherent to clinical trials. VAEs resulting from placebo administration are called nocebo effects. Overall, 12 studies reported headache as a VAE greater within the vaccine group than the placebo. However, 6 studies reported greater headache outcomes in the placebo group than the vaccine group. This may be due to differing sample sizes between the vaccine and the placebo group, with the placebo group being considerably smaller.
The “nocebo effect” has been defined as a negative effect experienced due to the belief that an intervention will cause harm. There is concern that this effect may occur when safety information of a vaccine is updated regularly with spontaneous VAEs, whether they are truly vaccine-related or not [90]. While the nocebo effect is more widely recognized among long-term vaccination efforts of well-described diseases, it has also been observed in recent COVID-19 vaccine trials as a potential factor for bias. In a meta-analysis of VAEs in COVID-19 RCTs, the incidence of nocebo responses was 16.4% while the magnitude was determined to be 0.3% [66]. Nocebo was attributed as a possible contribution for lowered vaccination rates in European countries due to public perception of the vaccine as less effective [91]. Additionally, a nationally representative cross-sectional survey in the UK also documented that side-effect expectation was associated with believing that COVID-19 vaccination was unsafe and ineffective [92].
Treatment Recommendations
Given the multitude of potential mediators contributing to vaccine-related headache, these events may require different treatment approaches. In the BNT162b2 mRNA COVID-19 vaccine trial, younger recipients were more likely to report taking an antipyretic or pain medication in response to a moderate or severe headache than older recipients [56]. Based on expert opinion, there is no contraindication to use of NSAIDs and acetaminophen for treatment of a headache following vaccination; triptans may also be helpful. Infusion therapies for treatment of status migrainosus may be of particular benefit; anecdotally, we have seen 30–100% response rates with intravenous dihydroergotamine and neuroleptics.
Oral corticosteroids can also be considered after expected immunogenicity is established, especially if other severe non-headache symptoms are also present. There is no consensus on the amount and duration of steroids that will result in suppression of an immunocompetent person [93] but CDC warns of active treatment with high-dose corticosteroids (i.e., 20 or more mg of prednisone or equivalent per day when administered for 2 or more weeks). Moreover, some theoretical guidance is provided by both the Pfizer-BioNTech BNT162b2 mRNA COVID-19 vaccine (28 days after dose 1 and 7 days after dose 2) and the Moderna mRNA-1273 (42 days after day 1 and 14 days after dose 2) [94, 95]. Greater occipital nerve blocks with corticosteroid may also be effective and corticosteroid sparing when administered peripherally. In general, it is reasonable to delay use for at least 2 weeks, especially in the case of live-virus vaccines [96].
Our clinical practice has shown that it may be beneficial to address the possibility of acute headache triggering after vaccination in patients with a pre-existing primary headache disorder in preparation for vaccination. In addition, for patients with migraine, there are no contraindications to the use of preventive therapies including onabotulinumtoxinA and monoclonal antibodies against calcitonin gene-related peptide [97]. It may be helpful to have a plan to escalate treatment as needed depending on response, including the potential treatment of status migrainosus. Longer term preventive therapies may be indicated for rare cases of headache persistence (e.g., amitriptyline and venlafaxine); treatment options should be guided by the headache phenotype.
Conclusion
As both passive surveillance and RCTs have shown, headache is a common although mostly mild and transient VAE following vaccination. There is heterogeneity among randomized controlled trials regarding the grading and scoring of headache severity; therefore, comparison is limited. Often, especially in pediatric trials, headache is not considered or is grouped with other systemic VAEs, which is a limiting factor towards understanding headache as a VAE post-vaccination.
There may be triggering of attacks in patients with baseline primary headache disorders or de novo headache. De novo headache post-vaccination should be considered for inclusion in the next iteration of the International Classification of Headache Disorders. Standardized grading methods, risk factors for persistence, and treatment are warranted in clinical trials, including in open-label phases.
Clinicians including headache specialists play a major role in helping people assess their personal eligibility for a vaccine and weigh the risks and benefits. Communication regarding the relative safety of vaccination and the transient and benign nature of the majority of potential systemic effects including headache can be crucial in the promotion of public health.
References
Biswas N, Mustapha T, Khubchandani J, Price JH. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021;46(6):1244–51. https://doi.org/10.1007/s10900-021-00984-3.
Stovner LJ, Hagen K, Linde M, Steiner TJ. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain. 2022;23(1):34. https://doi.org/10.1186/s10194-022-01402-2.
Ward BJ, Makarkov A, Seguin A, Pillet S, Trepanier S, Dhaliwall J, et al. Efficacy, immunogenicity, and safety of a plant-derived, quadrivalent, virus-like particle influenza vaccine in adults (18–64 years) and older adults (>/=65 years): two multicentre, randomised phase 3 trials. Lancet. 2020;396(10261):1491–503. https://doi.org/10.1016/S0140-6736(20)32014-6.
Chang LJ, Meng Y, Janosczyk H, Landolfi V, Talbot HK, Group QHDS. Safety and immunogenicity of high-dose quadrivalent influenza vaccine in adults >/=65years of age: a phase 3 randomized clinical trial. Vaccine. 2019;37(39):5825–34. https://doi.org/10.1016/j.vaccine.2019.08.016.
Vesikari T, Nauta J, Lapini G, Montomoli E, van de Witte S. Immunogenicity and safety of quadrivalent versus trivalent inactivated subunit influenza vaccine in children and adolescents: a phase III randomized study. Int J Infect Dis. 2020;92:29–37. https://doi.org/10.1016/j.ijid.2019.12.010.
Endo M, Tanishima M, Ibaragi K, Hayashida K, Fukuda T, Tanabe T, et al. Clinical phase II and III studies of an AS03-adjuvanted H5N1 influenza vaccine produced in an EB66((R)) cell culture platform. Influenza Other Respir Viruses. 2020;14(5):551–63. https://doi.org/10.1111/irv.12755.
Chu K, Xu K, Tang R, Tian X, Hu J, Yang T, et al. Immunogenicity and safety of an inactivated quadrivalent influenza vaccine: a randomized, double-blind, controlled phase III study in healthy population aged >/=3 years. Vaccine. 2020;38(37):5940–6. https://doi.org/10.1016/j.vaccine.2020.06.071.
Lan PT, Toan NT, Thang HA, Thang TC, Be LV, Thai DH, et al. A phase 2/3 double-blind, randomized, placebo-controlled study to evaluate the safety and immunogenicity of a seasonal trivalent inactivated split-virion influenza vaccine (IVACFLU-S) in healthy adults in Vietnam. Hum Vaccin Immunother. 2019;15(12):2933–9. https://doi.org/10.1080/21645515.2019.1613127.
Loebermann M, Fritzsche C, Geerdes-Fenge H, Heijnen E, Kirby D, Reisinger EC. A phase III, open-label, single-arm, study to evaluate the safety and immunogenicity of a trivalent, surface antigen inactivated subunit influenza virus vaccine produced in mammalian cell culture (Optaflu(R)) in healthy adults. Infection. 2019;47(1):105–9. https://doi.org/10.1007/s15010-018-1233-2.
Sarkar S, Bokade C, Garg K, Kumar R, Sanmukhani J, Mittal R. Immunogenicity and safety of the first indigenously developed Indian tetravalent influenza vaccine (split virion) in healthy children (6 months to 17 years of age): a randomized, multicenter, phase III clinical trial. Hum Vaccin Immunother. 2021;17(3):681–9. https://doi.org/10.1080/21645515.2020.1794683.
Ward BJ, Seguin A, Couillard J, Trepanier S, Landry N. Phase III: randomized observer-blind trial to evaluate lot-to-lot consistency of a new plant-derived quadrivalent virus like particle influenza vaccine in adults 18–49 years of age. Vaccine. 2021;39(10):1528–33. https://doi.org/10.1016/j.vaccine.2021.01.004.
Song JY, Lee J, Woo HJ, Wie SH, Lee JS, Kim SW, et al. Immunogenicity and safety of an egg-based inactivated quadrivalent influenza vaccine (GC3110A) versus two inactivated trivalent influenza vaccines with alternate B strains: a phase randomized clinical trial in adults. Hum Vaccin Immunother. 2019;15(3):710–6. https://doi.org/10.1080/21645515.2018.1536589.
Beran J, Reynales H, Poder A, Yu CY, Pitisuttithum P, Yuan LL, et al. Prevention of influenza during mismatched seasons in older adults with an MF59-adjuvanted quadrivalent influenza vaccine: a randomised, controlled, multicentre, phase 3 efficacy study. Lancet Infect Dis. 2021;21(7):1027–37. https://doi.org/10.1016/S1473-3099(20)30694-0.
Yamazaki Y, Ikeda M, Imada T, Furuno K, Mizukami T, de Solom R, et al. A phase 3, multicenter, single-arm, open-label study to assess the safety, tolerability, and immunogenicity of a single dose of 13-valent pneumococcal conjugate vaccine in Japanese participants aged 6–64 years who are considered to be at increased risk of pneumococcal disease and who are naive to pneumococcal vaccines. Vaccine. 2021;39(43):6414–21. https://doi.org/10.1016/j.vaccine.2021.08.106.
Klein NP, Peyrani P, Yacisin K, Caldwell N, Xu X, Scully IL, et al. A phase 3, randomized, double-blind study to evaluate the immunogenicity and safety of 3 lots of 20-valent pneumococcal conjugate vaccine in pneumococcal vaccine-naive adults 18 through 49 years of age. Vaccine. 2021;39(38):5428–35. https://doi.org/10.1016/j.vaccine.2021.07.004.
Song JY, Chang CJ, Andrews C, Diez-Domingo J, Oh MD, Dagan R, et al. Safety, tolerability, and immunogenicity of V114, a 15-valent pneumococcal conjugate vaccine, followed by sequential PPSV23 vaccination in healthy adults aged>/=50years: a randomized phase III trial (PNEU-PATH). Vaccine. 2021;39(43):6422–36. https://doi.org/10.1016/j.vaccine.2021.08.038.
Bastidas A, de la Serna J, El Idrissi M, Oostvogels L, Quittet P, Lopez-Jimenez J, et al. Effect of recombinant zoster vaccine on incidence of herpes zoster after autologous stem cell transplantation: a randomized clinical trial. JAMA. 2019;322(2):123–33. https://doi.org/10.1001/jama.2019.9053.
Dagnew AF, Ilhan O, Lee WS, Woszczyk D, Kwak JY, Bowcock S, et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in adults with haematological malignancies: a phase 3, randomised, clinical trial and post-hoc efficacy analysis. Lancet Infect Dis. 2019;19(9):988–1000. https://doi.org/10.1016/S1473-3099(19)30163-X.
Vink P, Delgado Mingorance I, Maximiano Alonso C, Rubio-Viqueira B, Jung KH, Rodriguez Moreno JF, et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in patients with solid tumors, vaccinated before or during chemotherapy: a randomized trial. Cancer. 2019;125(8):1301–12. https://doi.org/10.1002/cncr.31909.
Curran D, Kim JH, Matthews S, Dessart C, Levin MJ, Oostvogels L, et al. Recombinant zoster vaccine is efficacious and safe in frail individuals. J Am Geriatr Soc. 2021;69(3):744–52. https://doi.org/10.1111/jgs.16917.
Ocran-Appiah J, Boutry C, Herve C, Soni J, Schuind A, Group Z-S. Safety of the adjuvanted recombinant zoster vaccine in adults aged 50 years or older. A phase IIIB, non-randomized, multinational, open-label study in previous ZOE-50 and ZOE-70 placebo recipients. Vaccine. 2021;39(1):6–10. https://doi.org/10.1016/j.vaccine.2020.10.029.
Schmader KE, Levin MJ, Chen M, Matthews S, Riley ME, Woo W, et al. Impact of reactogenicity after two doses of recombinant zoster vaccine upon physical functioning and quality of life: an open phase III trial in older adults. J Gerontol A Biol Sci Med Sci. 2021;76(3):485–90. https://doi.org/10.1093/gerona/glaa127.
Schmader KE, Levin MJ, Grupping K, Matthews S, Butuk D, Chen M, et al. The impact of reactogenicity after the first dose of recombinant zoster vaccine on the physical functioning and quality of life of older adults: an open-label, phase III trial. J Gerontol A Biol Sci Med Sci. 2019;74(8):1217–24. https://doi.org/10.1093/gerona/gly218.
Lopez-Fauqued M, Campora L, Delannois F, El Idrissi M, Oostvogels L, De Looze FJ, et al. Safety profile of the adjuvanted recombinant zoster vaccine: pooled analysis of two large randomised phase 3 trials. Vaccine. 2019;37(18):2482–93. https://doi.org/10.1016/j.vaccine.2019.03.043.
Mikamo H, Yamagishi Y, Murata S, Yokokawa R, Han SR, Wakana A, et al. Efficacy, safety, and immunogenicity of a quadrivalent HPV vaccine in Japanese men: a randomized, phase 3, placebo-controlled study. Vaccine. 2019;37(12):1651–8. https://doi.org/10.1016/j.vaccine.2019.01.069.
Joura EA, Ulied A, Vandermeulen C, Rua Figueroa M, Seppa I, Hernandez Aguado JJ, et al. Immunogenicity and safety of a nine-valent human papillomavirus vaccine in women 27–45years of age compared to women 16–26 years of age: an open-label phase 3 study. Vaccine. 2021;39(20):2800–9. https://doi.org/10.1016/j.vaccine.2021.01.074.
Chen W, Zhao Y, Xie X, Liu J, Li J, Zhao C, et al. Safety of a quadrivalent human papillomavirus vaccine in a Phase 3, randomized, double-blind, placebo-controlled clinical trial among Chinese women during 90months of follow-up. Vaccine. 2019;37(6):889–97. https://doi.org/10.1016/j.vaccine.2018.12.030.
Thiem VD, Quang ND, Tuan NH, Cheon K, Gallagher N, Luxembourg A, et al. Immunogenicity and safety of a nine-valent human papillomavirus vaccine in Vietnamese males and females (9 to 26 years of age): an open-label, phase 3 trial. Hum Vaccin Immunother. 2021;17(7):1980–5. https://doi.org/10.1080/21645515.2020.1865739.
Su YY, Lin BZ, Zhao H, Li J, Lin ZJ, Qiao YL, et al. Lot-to-lot consistency study of an Escherichia coli-produced bivalent human papillomavirus vaccine in adult women: a randomized trial. Hum Vaccin Immunother. 2020;16(7):1636–44. https://doi.org/10.1080/21645515.2019.1691413.
Dhingra MS, Peterson J, Hedrick J, Pan J, Neveu D, Jordanov E. Immunogenicity, safety and inter-lot consistency of a meningococcal conjugate vaccine (MenACYW-TT) in adolescents and adults: a phase III randomized study. Vaccine. 2020;38(33):5194–201. https://doi.org/10.1016/j.vaccine.2020.06.013.
Esteves-Jaramillo A, Koehler T, Jeanfreau R, Neveu D, Jordanov E, Singh DM. Immunogenicity and safety of a quadrivalent meningococcal tetanus toxoid-conjugate vaccine (MenACYW-TT) in >/=56-year-olds: a phase III randomized study. Vaccine. 2020;38(28):4405–11. https://doi.org/10.1016/j.vaccine.2020.04.067.
Group MMRS. A second dose of a measles-mumps-rubella vaccine administered to healthy four-to-six-year-old children: a phase III, observer-blind, randomized, safety and immunogenicity study comparing GSK MMR and MMR II with and without DTaP-IPV and varicella vaccines co-administration. Hum Vaccin Immunother. 2019;15(4):786–99. https://doi.org/10.1080/21645515.2018.1554971.
Baccarini CI, Simon MW, Brandon D, Christensen S, Jordanov E, Dhingra MS. Safety and immunogenicity of a quadrivalent meningococcal conjugate vaccine in healthy meningococcal-naive children 2–9 years of age: a phase III, randomized study. Pediatr Infect Dis J. 2020;39(10):955–60. https://doi.org/10.1097/INF.0000000000002832.
Nolan T, Santolaya ME, de Looze F, Marshall H, Richmond P, Henein S, et al. Antibody persistence and booster response in adolescents and young adults 4 and 7.5 years after immunization with 4CMenB vaccine. Vaccine. 2019;37(9):1209–18. https://doi.org/10.1016/j.vaccine.2018.12.059.
Vesikari T, Peyrani P, Webber C, Van Der Wielen M, Cheuvart B, De Schrevel N, et al. Ten-year antibody persistence and booster response to MenACWY-TT vaccine after primary vaccination at 1–10 years of age. Hum Vaccin Immunother. 2020;16(6):1280–91. https://doi.org/10.1080/21645515.2020.1746110.
Anez G, Hedrick J, Simon MW, Christensen S, Jeanfreau R, Yau E, et al. Immunogenicity and safety of a booster dose of a quadrivalent meningococcal tetanus toxoid-conjugate vaccine (MenACYW-TT) in adolescents and adults: a phase III randomized study. Hum Vaccin Immunother. 2020;16(6):1292–8. https://doi.org/10.1080/21645515.2020.1733867.
Vesikari T, Ostergaard L, Beeslaar J, Absalon J, Eiden JJ, Jansen KU, et al. Persistence and 4-year boosting of the bactericidal response elicited by two- and three-dose schedules of MenB-FHbp: a phase 3 extension study in adolescents. Vaccine. 2019;37(12):1710–9. https://doi.org/10.1016/j.vaccine.2018.11.073.
Tipton M, Daly W, Senders S, Block SL, Lattanzi M, Mzolo T, et al. MenACWY-CRM conjugate vaccine booster dose given 4–6years after priming: results from a phase IIIb, multicenter, open label study in adolescents and adults. Vaccine. 2019;37(42):6171–9. https://doi.org/10.1016/j.vaccine.2019.08.065.
Nolan T, Booy R, Marshall HS, Richmond P, Nissen M, Ziegler JB, et al. Immunogenicity and safety of a quadrivalent meningococcal ACWY-tetanus toxoid conjugate vaccine 6 years after MenC priming as toddlers. Pediatr Infect Dis J. 2019;38(6):643–50. https://doi.org/10.1097/INF.0000000000002334.
Jiang F, Zhang R, Guan Q, Mu Q, He P, Ye X, et al. Immunogenicity and safety of a live attenuated varicella vaccine in children 1–12 years of age: a randomized, blinded, controlled, non-inferiority phase 3 clinical trial. Contemp Clin Trials. 2021;107:106489. https://doi.org/10.1016/j.cct.2021.106489.
Asatryan A, Meyer N, Scherbakov M, Romanenko V, Osipova I, Galustyan A, et al. Immunogenicity, safety, and reactogenicity of combined reduced-antigen-content diphtheria-tetanus-acellular pertussis vaccine administered as a booster vaccine dose in healthy Russian participants: a phase III, open-label study. Hum Vaccin Immunother. 2021;17(3):723–30. https://doi.org/10.1080/21645515.2020.1796423.
Vesikari T, Langley JM, Segall N, Ward BJ, Cooper C, Poliquin G, et al. Immunogenicity and safety of a tri-antigenic versus a mono-antigenic hepatitis B vaccine in adults (PROTECT): a randomised, double-blind, phase 3 trial. Lancet Infect Dis. 2021;21(9):1271–81. https://doi.org/10.1016/S1473-3099(20)30780-5.
Chaparro M, Gordillo J, Domenech E, Esteve M, Barreiro-de Acosta M, Villoria A, et al. Fendrix vs Engerix-B for primo-vaccination against hepatitis B infection in patients with inflammatory bowel disease: a randomized clinical trial. Am J Gastroenterol. 2020;115(11):1802–11. https://doi.org/10.14309/ajg.0000000000000926.
Lee J, Choi JH, Wie SH, Park SH, Choi SM, Lee MS, et al. A phase III study to evaluate the immunogenicity and safety of GC1107 (adult tetanus diphtheria vaccine) in healthy adults. J Korean Med Sci. 2019;34(4):e31. https://doi.org/10.3346/jkms.2019.34.e31.
Arredondo JL, Villagomez Martinez SM, Concepcion Morales M, Meyer S, Toh ML, Zocchetti C, et al. Immunogenicity and safety of a tetravalent dengue vaccine and a bivalent HPV vaccine given concomitantly or sequentially in girls aged 9 to 14 years in Mexico. Vaccine. 2021;39(25):3388–96. https://doi.org/10.1016/j.vaccine.2021.04.064.
Shen H, Wang Z, Yang B, Cai K, Jiang C, Xie R, et al. Immunogenicity and safety of purified vero cell-cultured rabies vaccine under Zagreb 2–1-1 or 5-dose Essen regimen in the healthy Chinese subjects: a randomized, double-blind, positive controlled phase 3 clinical trial. Hum Vaccin Immunother. 2021;17(2):351–7. https://doi.org/10.1080/21645515.2020.1778408.
Matson MA, Schenker E, Stein M, Zamfirova V, Nguyen HB, Bergman GE. Safety and efficacy results of simulated post-exposure prophylaxis with human immune globulin (HRIG; KEDRAB) co-administered with active vaccine in healthy subjects: a comparative phase 2/3 trial. Hum Vaccin Immunother. 2020;16(2):452–9. https://doi.org/10.1080/21645515.2019.1656967.
de Bruyn G, Gordon DL, Steiner T, Tambyah P, Cosgrove C, Martens M, et al. Safety, immunogenicity, and efficacy of a Clostridioides difficile toxoid vaccine candidate: a phase 3 multicentre, observer-blind, randomised, controlled trial. Lancet Infect Dis. 2021;21(2):252–62. https://doi.org/10.1016/S1473-3099(20)30331-5.
McCarty JM, Lock MD, Bennett S, Hunt KM, Simon JK, Gurwith M. Age-related immunogenicity and reactogenicity of live oral cholera vaccine CVD 103-HgR in a randomized, controlled clinical trial. Vaccine. 2019;37(11):1389–97. https://doi.org/10.1016/j.vaccine.2019.01.077.
Gray GE, Bekker LG, Laher F, Malahleha M, Allen M, Moodie Z, et al. Vaccine efficacy of ALVAC-HIV and bivalent subtype C gp120-MF59 in adults. N Engl J Med. 2021;384(12):1089–100. https://doi.org/10.1056/NEJMoa2031499.
Brogan PA, Hofer M, Kuemmerle-Deschner JB, Kone-Paut I, Roesler J, Kallinich T, et al. Rapid and sustained long-term efficacy and safety of canakinumab in patients with cryopyrin-associated periodic syndrome ages five years and younger. Arthritis Rheumatol. 2019;71(11):1955–63. https://doi.org/10.1002/art.41004.
Riveau G, Schacht AM, Dompnier JP, Deplanque D, Seck M, Waucquier N, et al. Safety and efficacy of the rSh28GST urinary schistosomiasis vaccine: a phase 3 randomized, controlled trial in Senegalese children. PLoS Negl Trop Dis. 2018;12(12):e0006968. https://doi.org/10.1371/journal.pntd.0006968.
Markman J, Resnick M, Greenberg S, Katz N, Yang R, Scavone J, et al. Efficacy of pregabalin in post-traumatic peripheral neuropathic pain: a randomized, double-blind, placebo-controlled phase 3 trial. J Neurol. 2018;265(12):2815–24. https://doi.org/10.1007/s00415-018-9063-9.
Song JY, Jeong HW, Yun JW, Lee J, Woo HJ, Bae JY, et al. Immunogenicity and safety of a modified three-dose priming and booster schedule for the Hantaan virus vaccine (Hantavax): a multi-center phase III clinical trial in healthy adults. Vaccine. 2020;38(50):8016–23. https://doi.org/10.1016/j.vaccine.2020.10.035.
Halperin SA, Das R, Onorato MT, Liu K, Martin J, Grant-Klein RJ, et al. Immunogenicity, lot consistency, and extended safety of rVSVDeltaG-ZEBOV-GP vaccine: a phase 3 randomized, double-blind, placebo-controlled study in healthy adults. J Infect Dis. 2019;220(7):1127–35. https://doi.org/10.1093/infdis/jiz241.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–15. https://doi.org/10.1056/NEJMoa2034577.
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–16. https://doi.org/10.1056/NEJMoa2035389.
Moderna TX I. Vaccines and related biological products advisory committee meeting, December 17, 2020: FDA Briefing Document 2020. Available from: https://www.fda.gov/media/144434/download.
Sadoff J, Gray G, Vandebosch A, Cardenas V, Shukarev G, Grinsztejn B, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. 2021;384(23):2187–201. https://doi.org/10.1056/NEJMoa2101544.
Ramasamy MN, Minassian AM, Ewer KJ, Flaxman AL, Folegatti PM, Owens DR, et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet. 2021;396(10267):1979–93. https://doi.org/10.1016/S0140-6736(20)32466-1.
Heath PT, Galiza EP, Baxter DN, Boffito M, Browne D, Burns F, et al. Safety and efficacy of NVX-CoV2373 Covid-19 vaccine. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2107659.
Keech C, Albert G, Cho I, Robertson A, Reed P, Neal S, et al. Phase 1–2 trial of a SARS-CoV-2 recombinant spike protein nanoparticle vaccine. N Engl J Med. 2020;383(24):2320–32. https://doi.org/10.1056/NEJMoa2026920.
Pfizer-BioNTech COVID-19 vaccine BNT162, P-. Vaccines and related biological products advisory committee briefing document. 2020. Available from: https://www.fda.gov/media/144434/download.
Pfizer-BioNTech COVID-19 Vaccine Reactions & Adverse Events. https://www.cdc.gov/vaccines/covid-19/info-by-product/pfizer/reactogenicity.html (2021). Accessed 28 Nov 2021.
Frenck RW Jr, Klein NP, Kitchin N, Gurtman A, Absalon J, Lockhart S, et al. Safety, immunogenicity, and efficacy of the BNT162b2 Covid-19 vaccine in adolescents. N Engl J Med. 2021;385(3):239–50. https://doi.org/10.1056/NEJMoa2107456.
Lee YH, Song GG. Nocebo responses in randomized controlled trials of COVID-19 vaccines. Int J Clin Pharmacol Ther. 2021. https://doi.org/10.5414/CP204028.
Tanriover MD, Doganay HL, Akova M, Guner HR, Azap A, Akhan S, et al. Efficacy and safety of an inactivated whole-virion SARS-CoV-2 vaccine (CoronaVac): interim results of a double-blind, randomised, placebo-controlled, phase 3 trial in Turkey. Lancet. 2021;398(10296):213–22. https://doi.org/10.1016/S0140-6736(21)01429-X.
Castaldo M, Waliszewska-Prosół M, Koutsokera M, Robotti M, Straburzyński M, Apostolakopoulou L, et al. Headache onset after vaccination against SARS-CoV-2: a systematic literature review and meta-analysis. J Headache Pain. 2022;23(1):41. https://doi.org/10.1186/s10194-022-01400-4.
Klugar M, Riad A, Mekhemar M, Conrad J, Buchbender M, Howaldt HP, et al. Side effects of mRNA-based and viral vector-based COVID-19 vaccines among German healthcare workers. Biology. 2021;10(8):752.
Riad A, Pokorna A, Attia S, Klugarova J, Koscik M, Klugar M. Prevalence of COVID-19 vaccine side effects among healthcare workers in the Czech Republic. J Clin Med. 2021;10(7).
Mattiuzzi C, Lippi G. Headache after COVID-19 vaccination: updated report from the Italian Medicines Agency database. Neurol Sci. 2021;42(9):3531–2. https://doi.org/10.1007/s10072-021-05354-4.
Herve C, Laupeze B, Del Giudice G, Didierlaurent AM, Tavares Da Silva F. The how’s and what’s of vaccine reactogenicity. NPJ Vaccines. 2019;4:39. https://doi.org/10.1038/s41541-019-0132-6.
Goadsby PJ, Holland PR. An update: pathophysiology of migraine. Neurol Clin. 2019;37(4):651–71. https://doi.org/10.1016/j.ncl.2019.07.008.
Ferrari MD, Goadsby PJ, Burstein R, Kurth T, Ayata C, Charles A, et al. Migraine Nat Rev Dis Primers. 2022;8(1):2. https://doi.org/10.1038/s41572-021-00328-4.
Robbins MS, Grosberg BM, Napchan U, Crystal SC, Lipton RB. Clinical and prognostic subforms of new daily-persistent headache. Neurology. 2010;74(17):1358–64. https://doi.org/10.1212/WNL.0b013e3181dad5de.
Ekizoglu E, Gezegen H, Yalinay Dikmen P, Orhan EK, Ertas M, Baykan B. The characteristics of COVID-19 vaccine-related headache: clues gathered from the healthcare personnel in the pandemic. Cephalalgia. 2021:3331024211042390. https://doi.org/10.1177/03331024211042390.
Gobel CH, Heinze A, Karstedt S, Morscheck M, Tashiro L, Cirkel A, et al. Clinical characteristics of headache after vaccination against COVID-19 (coronavirus SARS-CoV-2) with the BNT162b2 mRNA vaccine: a multicentre observational cohort study. Brain Commun. 2021;3(3):fcab169. https://doi.org/10.1093/braincomms/fcab169.
Gobel CH, Heinze A, Karstedt S, Morscheck M, Tashiro L, Cirkel A, et al. Headache attributed to vaccination against COVID-19 (coronavirus SARS-CoV-2) with the ChAdOx1 nCoV-19 (AZD1222) vaccine: a multicenter observational cohort study. Pain Ther. 2021;10(2):1309–30. https://doi.org/10.1007/s40122-021-00296-3.
Consoli S, Dono F, Evangelista G, D’Apolito M, Travaglini D, Onofrj M, et al. Status migrainosus: a potential adverse reaction to Comirnaty (BNT162b2, BioNtech/Pfizer) COVID-19 vaccine-a case report. Neurol Sci. 2021. https://doi.org/10.1007/s10072-021-05741-x.
Silvestro M, Tessitore A, Orologio I, Sozio P, Napolitano G, Siciliano M, et al. Headache worsening after COVID-19 vaccination: an online questionnaire-based study on 841 patients with migraine. J Clin Med. 2021;10(24).
Rattanawong W, Akaratanawat W, Tepmongkol S, Chutinet A, Tantivatana J, Suwanwela NC. Acute prolonged motor aura resembling ischemic stroke after COVID - 19 vaccination (CoronaVac): the first case report. J Headache Pain. 2021;22(1):93. https://doi.org/10.1186/s10194-021-01311-w.
Salai G, Bilic E, Primorac D, Lakusic DM, Bilic H, Lazibat I, et al. Benign fasciculation syndrome and migraine aura without headache: possible rare side effects of the BNT162b2 mRNA vaccine? A case report and a potential hypothesis. Vaccines (Basel). 2022;10(1).
Suwanwela NC, Kijpaisalratana N, Tepmongkol S, Rattanawong W, Vorasayan P, Charnnarong C, et al. Prolonged migraine aura resembling ischemic stroke following CoronaVac vaccination: an extended case series. J Headache Pain. 2022;23(1):13. https://doi.org/10.1186/s10194-022-01385-0.
Sekiguchi K, Watanabe N, Miyazaki N, Ishizuchi K, Iba C, Tagashira Y, et al. Incidence of headache after COVID-19 vaccination in patients with history of headache: a cross-sectional study. Cephalalgia. 2021:3331024211038654. https://doi.org/10.1177/03331024211038654.
Sharifian-Dorche M, Bahmanyar M, Sharifian-Dorche A, Mohammadi P, Nomovi M, Mowla A. Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis post COVID-19 vaccination; a systematic review. J Neurol Sci. 2021;428:117607. https://doi.org/10.1016/j.jns.2021.117607.
Pawlowski C, Rincon-Hekking J, Awasthi S, Pandey V, Lenehan P, Venkatakrishnan AJ, et al. Cerebral venous sinus thrombosis is not significantly linked to COVID-19 vaccines or non-COVID vaccines in a large multi-state health system. J Stroke Cerebrovasc Dis. 2021;30(10):105923. https://doi.org/10.1016/j.jstrokecerebrovasdis.2021.105923.
Sanchez van Kammen M, Aguiar de Sousa D, Poli S, Cordonnier C, Heldner MR, van de Munckhof A, et al. Characteristics and outcomes of patients with cerebral venous sinus thrombosis in SARS-CoV-2 vaccine-induced immune thrombotic thrombocytopenia. JAMA Neurol. 2021;78(11):1314–23. https://doi.org/10.1001/jamaneurol.2021.3619.
Palaiodimou L, Stefanou MI, Katsanos AH, Aguiar de Sousa D, Coutinho JM, Lagiou P, et al. Cerebral venous sinus thrombosis and thrombotic events after vector-based COVID-19 vaccines: a systematic review and meta-analysis. Neurology. 2021;97(21):e2136-e47. https://doi.org/10.1212/WNL.0000000000012896.
Garcia-Azorin D, Do TP, Gantenbein AR, Hansen JM, Souza MNP, Obermann M, et al. Delayed headache after COVID-19 vaccination: a red flag for vaccine induced cerebral venous thrombosis. J Headache Pain. 2021;22(1):108. https://doi.org/10.1186/s10194-021-01324-5.
Okais C, Gay C, Seon F, Buchaille L, Chary E, Soubeyrand B. Disease-specific adverse events following nonlive vaccines: a paradoxical placebo effect or a nocebo phenomenon? Vaccine. 2011;29(37):6321–6. https://doi.org/10.1016/j.vaccine.2011.05.045.
Amanzio M, Cipriani GE, Bartoli M. How do nocebo effects in placebo groups of randomized controlled trials provide a possible explicative framework for the COVID-19 pandemic? Expert Rev Clin Pharmacol. 2021;14(4):439–44. https://doi.org/10.1080/17512433.2021.1900728.
Smith LE, Sim J, Amlot R, Cutts M, Dasch H, Sevdalis N, et al. Side-effect expectations from COVID-19 vaccination: findings from a nationally representative cross-sectional survey (CoVAccS - wave 2). J Psychosom Res. 2021;152:110679. https://doi.org/10.1016/j.jpsychores.2021.110679.
Rubin LG, Levin MJ, Ljungman P, Davies EG, Avery R, Tomblyn M, et al. 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clin Infect Dis. 2014;58(3):e44-100. https://doi.org/10.1093/cid/cit684.
Hong SM, Park YW, Choi EJ. Steroid injections in pain management: influence on coronavirus disease 2019 vaccines. Korean J Pain. 2022;35(1):14–21. https://doi.org/10.3344/kjp.2022.35.1.14.
Spine Intervention Society. Preliminary recommendations on corticosteroid injections and COVID-19 vaccinations friday, January 22, 2021. Available from: https://www.spineintervention.org/news/548668/Preliminary-Recommendations-on-Corticosteroid-Injections-and-COVID-19-Vaccinations.htm.
Chow RM, Rajput K, Howie BA, Varhabhatla N. The COVID-19 vaccine and interventional procedures: exploring the relationship between steroid administration and subsequent vaccine efficacy. Pain Pract. 2021;21(8):966–73. https://doi.org/10.1111/papr.13062.
Gelfand AA, Poland G. Migraine treatment and COVID-19 vaccines: no cause for concern. Headache. 2021;61(3):409–11. https://doi.org/10.1111/head.14086.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kimberly Garces and Alexandra Cocores do not report any significant disclosures or conflicts of interest. Peter James Goadsby reports, over the last 36 months, grants and personal fees from Eli-Lilly and Company, grant from Celgene, and personal fees from Aeon Biopharma, Allergan/Abbvie, Amgen, Biodelivery Sciences International, Biohaven Pharmaceuticals Inc., CoolTech LLC, Dr Reddys, Epalex, GlaxoSmithKline, Impel Neuropharma, Lundbeck, Novartis, Praxis, Sanofi, Satsuma and Teva Pharmaceuticals, and personal fees for advice through Gerson Lehrman Group, Guidepoint, SAI Med Partners, Vector Metric, and fees for educational materials from CME Outfitters, Omnia Education, WebMD, and publishing royalties or fees from Massachusetts Medical Society, Oxford University Press, UptoDate and Wolters Kluwer, and for medicolegal advice in headache. Teshamae Monteith has received personal compensation for serving on advisory boards for Biohaven, Allegan/Abbvie, Lundbeck, Amgen, Teva, Linpharma and Impel Neuropharmaceuticals. She has also served as a site principal investigator without direct compensation for Teva, Eli Lilly, Electrocore, Amgen, Novartis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of Topical Collection on Secondary Headache
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garces, K.N., Cocores, A.N., Goadsby, P.J. et al. Headache After Vaccination: An Update on Recent Clinical Trials and Real-World Reporting. Curr Pain Headache Rep 26, 895–918 (2022). https://doi.org/10.1007/s11916-022-01094-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-022-01094-y