Abstract
Purpose of Review
Chronic low back pain (CLBP) is a major source of physical and psychiatric morbidity and mortality, and the current overreliance on opioid analgesics has contributed to a burgeoning epidemic in the USA. Cognitive behavioral therapy (CBT) is an empirically supported treatment for CLBP, but little information exists regarding its potential efficacy for CLBP’s precursor condition, subacute low back pain (sALBP), defined here as having a 7–12-week duration. Earlier intervention with CBT at the sALBP stage could produce larger clinical benefits. This systematic review was undertaken to characterize and highlight this knowledge gap.
Recent Findings
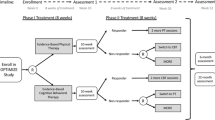
Of 240 unique articles identified by comprehensive database searches, only six prospective, sALBP-focused, randomized controlled trials (RCTs) published within the past 20 years met criteria for inclusion in this review. These studies varied widely in their sample sizes, precise definition of sALBP, nature of CBT intervention, and outcome measures. Five of the six showed significant improvements associated with CBT, but the heterogeneity of the studies prevented quantitative comparisons.
Summary
CBT has not been adequately studied as a potential early intervention treatment for sALBP patients. None of the six identified papers studied US civilians or leveraged innovations such as teletherapy—able to reach patients in remote or underserved areas—underscoring critical gaps in current back pain treatment. Given the severity of the US opioid epidemic, non-pharmacologic options such as CBT should be rigorously explored in the sALBP population.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Manchikanti L, Singh V, Falco FJ, Benyamin RM, Hirsch JA. Epidemiology of low back pain in adults. Neuromodulation. 2014;17(Suppl 2):3–10. https://doi.org/10.1111/ner.12018.
Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–24. https://doi.org/10.1016/j.jpain.2012.03.009.
Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–81. https://doi.org/10.1016/j.berh.2010.10.002.
Crombez G, Eccleston C, Van Damme S, Vlaeyen JWS, Karoly P. Fear-avoidance model of chronic pain: the next generation. Clin J Pain. 2012;28(6):475–83. https://doi.org/10.1097/ajp.0b013e3182385392.
Saunders KW, Dunn KM, Merrill JO, Sullivan M, Weisner C, Braden JB, et al. Relationship of opioid use and dosage levels to fractures in older chronic pain patients. J Gen Intern Med. 2010;25(4):310–5. https://doi.org/10.1007/s11606-009-1218-z.
Sullivan MD. Limiting the potential harms of high-dose opioid therapy: comment on “Opioid dose and drug-related mortality in patients with nonmalignant pain”. Arch Intern Med. 2011;171(7):691–3. https://doi.org/10.1001/archinternmed.2011.101.
Katz N, Mazer NA. The impact of opioids on the endocrine system. Clin J Pain. 2009;25(2):170–5. https://doi.org/10.1097/AJP.0b013e3181850df6.
Fleming MF, Davis J, Passik SD. Reported lifetime aberrant drug-taking behaviors are predictive of current substance use and mental health problems in primary care patients. Pain Med. 2008;9(8):1098–106. https://doi.org/10.1111/j.1526-4637.2008.00491.x.
Meltzer EC, Rybin D, Saitz R, Samet JH, Schwartz SL, Butler SF, et al. Identifying prescription opioid use disorder in primary care: diagnostic characteristics of the current opioid misuse measure (COMM). Pain. 2011;152(2):397–402. https://doi.org/10.1016/j.pain.2010.11.006.
Webster LR, Cochella S, Dasgupta N, Fakata KL, Fine PG, Fishman SM, et al. An analysis of the root causes for opioid-related overdose deaths in the United States. Pain Med. 2011;12(Suppl 2):S26–35. https://doi.org/10.1111/j.1526-4637.2011.01134.x.
Saunders KW, Von Korff M, Campbell CI, Banta-Green CJ, Sullivan MD, Merrill JO, et al. Concurrent use of alcohol and sedatives among persons prescribed chronic opioid therapy: prevalence and risk factors. J Pain. 2012;13(3):266–75. https://doi.org/10.1016/j.jpain.2011.11.004.
Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. https://doi.org/10.7326/0003-4819-152-2-201001190-00006.
Passik SD, Lowery A. Psychological variables potentially implicated in opioid-related mortality as observed in clinical practice. Pain Med. 2011;12(Suppl 2):S36–42. https://doi.org/10.1111/j.1526-4637.2011.01130.x.
Von Korff M. Opioids for chronic musculoskeletal pain: putting patient safety first. Pain. 2013;154(12):2583–5. https://doi.org/10.1016/j.pain.2013.09.017.
Ingvar M. Learning mechanisms in pain chronification—teachings from placebo research. Pain. 2015;156(Suppl 1):S18–23. https://doi.org/10.1097/j.pain.0000000000000093.
Baliki MN, Petre B, Torbey S, Herrmann KM, Huang L, Schnitzer TJ, et al. Corticostriatal functional connectivity predicts transition to chronic back pain. Nat Neurosci. 2012;15(8):1117–9. https://doi.org/10.1038/nn.3153.
Mansour AR, Baliki MN, Huang L, Torbey S, Herrmann KM, Schnitzer TJ, et al. Brain white matter structural properties predict transition to chronic pain. Pain. 2013;154(10):2160–8. https://doi.org/10.1016/j.pain.2013.06.044.
Loggia ML, Kim J, Gollub RL, Vangel MG, Kirsch I, Kong J, et al. Default mode network connectivity encodes clinical pain: an arterial spin labeling study. Pain. 2013;154(1):24–33. https://doi.org/10.1016/j.pain.2012.07.029.
Institute for Clinical Systems Improvement (ICSI). Adult acute and subacute low back pain. In: National Guideline Clearinghouse (NGC). Rockville (MD): Agency for Healthcare Research and Quality (AHRQ). 2012. https://www.guideline.gov/summaries/summary/39319/adult-acute-and-subacute-low-back-pain. Accessed 10 Oct 2017.
Cunningham NR, Kashikar-Zuck S. Nonpharmacologic treatment of pain in rheumatic diseases and other musculoskeletal pain conditions. Curr Rheumatol Rep. 2013;15(2):306. https://doi.org/10.1007/s11926-012-0306-y.
Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624. https://doi.org/10.1037/0033-2909.133.4.581.
Hassett AL, Williams DA. Non-pharmacological treatment of chronic widespread musculoskeletal pain. Best Pract Res Clin Rheumatol. 2011;25(2):299–309. https://doi.org/10.1016/j.berh.2011.01.005.
Kerns RD, Sellinger J, Goodin BR. Psychological treatment of chronic pain. Annu Rev Clin Psychol. 2011;7(1):411–34. https://doi.org/10.1146/annurev-clinpsy-090310-120430.
Reid MC, Otis J, Barry LC, Kerns RD. Cognitive-behavioral therapy for chronic low back pain in older persons: a preliminary study. Pain Med. 2003;4(3):223–30. https://doi.org/10.1046/j.1526-4637.2003.03030.x.
• Sveinsdottir V, Eriksen HR, Reme SE. Assessing the role of cognitive behavioral therapy in the management of chronic nonspecific back pain. J Pain Res. 2012;5(10):371–80. https://doi.org/10.2147/JPR.S25330. Review describing the efficacy of CBT in CLBP.
•• Richmond H, Hall AM, Copsey B, Hansen Z, Williamson E, Hoxey-Thomas N, et al. The effectiveness of cognitive behavioural treatment for non-specific low back pain: a systematic review and meta-analysis. PLoS One. 2015;10(8):e0134192. https://doi.org/10.1371/journal.pone.0134192. A systematic review and meta-analysis of the efficacy of CBT in CLBP.
Linton SJ. A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976). 2000;25(9):1148–56. https://doi.org/10.1097/00007632-200005010-00017.
• Storheim K, Brox JI, Koller AK, Bø K. Intensive group training versus cognitive intervention in sub-acute low back pain: short term results of a single blind randomized controlled trial. J Rehabil Med. 2003;35(3):132–40. https://doi.org/10.1080/16501970310010484. Original RCT conducted in Norway and included in systematic review.
• Schiltenwolf M, Buchner M, Heindl B, Reumont J, Müller A, Eich W. Comparison of a biopsychosocial therapy (BT) with a conventional biomedical therapy (MT) of subacute low back pain in the first episode of sick leave: a randomized controlled trial. Eur Spine J. 2006;15(7):1083–92. https://doi.org/10.1007/s00586-005-0008-5. Original RCT conducted in Germany and included in systematic review.
• Lindell O, Johansson SE, Strender LE. Subacute and chronic non-specific back and neck pain: cognitive-behavioural rehabilitation versus primary care. A randomized controlled trial. BMC Musculoskeletal Disorders. 2008;9(1):172. https://doi.org/10.1186/1471-2474-9-172. Original RCT conducted in Sweden and included in systematic reviewBlinded US DoD study included in systematic review.
•• Slater MA, Weickgenant AL, Greenberg MA, Wahlgren DR, Williams RA, Carter C, et al. Preventing progression to chronicity in first onset, subacute low back pain: an exploratory study. Arch Phys Med Rehabil. 2009;90(4):545–52. https://doi.org/10.1016/j.apmr.2008.10.032. Blinded US DoD study included in systematic review.
• Lamb SE, Hansen Z, Lall R, Castelnuovo E, Withers EJ, Nichols V, et al. Group cognitive behavioural treatment for low-back pain in primary care: a randomised controlled trial and cost-effectiveness analysis. Lancet. 2010;375(9718):916–23. https://doi.org/10.1016/S0140-6736(09)62164-4. Original RCT conducted in England and included in systematic review.
•• Werner EL, Storheim K, Løchting I, Wisløff T, Grotle M. Cognitive patient education for low back pain in primary care: a cluster randomized controlled trial and cost-effectiveness analysis. Spine. 2016;41(6):455–62. https://doi.org/10.1097/BRS.0000000000001268. Recent original cluster RCT conducted in Norway and included in systematic review.
Turner JA, Mancl L, Aaron LA. Short- and long-term efficacy of brief cognitive-behavioral therapy for patients with chronic temporomandibular disorder pain: a randomized, controlled trial. Pain. 2006;121(3):181–94. https://doi.org/10.1016/j.pain.2005.11.017.
Lazaridou A, Kim J, Cahalan CM, Loggia ML, Franceschelli O, Berna C, et al. Effects of cognitive-behavioral therapy (CBT) on brain connectivity supporting catastrophizing in fibromyalgia. Clin J Pain. 2017;33(3):215–21. https://doi.org/10.1097/AJP.0000000000000422.
• Linton SJ. Early identification and intervention in the prevention of musculoskeletal pain. Am J Ind Med. 2002;41(5):433–42. https://doi.org/10.1002/ajim.10052. Demonstrated feasibility of CBT early intervention in back pain.
IASP (International Association for the Study of Pain). IASP Taxonomy. In: Classification of Chronic Pain, Second Edition. IASP Task Force on Taxonomy. 1994. Updated 2017. http://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698&&navItemNumber=576. Accessed 4 Aug 2016.
Kaye AD, Jones MR, Kaye AM, Ripoll JG, Galan V, Beakley BD, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 1. Pain Physician. 2017;20(2S):S93–S109.
Kaye AD, Jones MR, Kaye AM, Ripoll JG, Jones DE, Galan V, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse (part 2). Pain Physician. 2017;20(2S):S111–33.
Acknowledgements
The authors thank Anne Fladger, Dalton Tuggle, and Limeng Wan for their assistance.
Funding
TYM was partially supported by a 2015 NARSAD Young Investigator Grant and a 2017 Harvard Medical School Norman E. Zinberg Fellowship in Addiction Psychiatry Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Richard D. Urman, Catherine A. Hutchison, Robert N. Jamison, and Robert R. Edwards declare no conflict of interest. Dr. Mariano was on an advisory board of Janssen Pharmaceuticals for treatment-resistant depression in 12/2016, both outside of this work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Other Pain
Rights and permissions
About this article
Cite this article
Mariano, T.Y., Urman, R.D., Hutchison, C.A. et al. Cognitive Behavioral Therapy (CBT) for Subacute Low Back Pain: a Systematic Review. Curr Pain Headache Rep 22, 15 (2018). https://doi.org/10.1007/s11916-018-0669-5
Published:
DOI: https://doi.org/10.1007/s11916-018-0669-5