Abstract
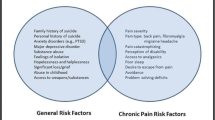
Chronic pain disorders can exert major negative effects on virtually every aspect of an individual’s life. It is not surprising then that many chronic pain sufferers find themselves at a point of emotional fragility where they experience thoughts of ending their life. Suicidal behavior encompasses a spectrum of experience, from “life weariness” or passive suicidal ideation, to more active suicidal intent and suicide completion. A range of risk factors for suicidal behavior in the general population have been identified, and these apply equally to the chronic pain population: a family history of mental illness, past history of suicide attempts, and the presence of comorbid depression. With regard specifically to chronic pain patients, elevated suicide risk is also associated with severe or recurrent headache, ambiguous diagnoses (psychogenic pain, abdominal pain), and medicolegal issues related to the pain. A number of suggestions for clinicians managing chronic pain patients with regards to managing suicide risk are given.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Webster LR. Pain and Suicide: the other side of the opioid story. Pain Med. 2014;15:345–6.
O’Donovan A. Managing risk. In: O’Donovan A, Casey L, van der Veen M, Boschen M, editors. Psychotherapy: An Australian Perspective. East Hawthorn, Victoria: IP Communications; 2013. p. 302–18.
Renberg ES. Self-reported life-weariness, death wishes, suicidal ideation, suicidal plans and suicide attempts in general population surveys in the north of Sweden 1986 and 1996. Sock Psychiatry Psychiatr Epidemiol. 2001;36:429–36.
Fishbain DA, Burns D, Disrobe JM, Lewis JE. Risk for five forms of suicidality in acute pain patients and chronic pain patients vs pain‐free community controls. Pain Med. 2009;10:1095–105.
Rockett IR, Regier MD, Kapusta ND, Coben JH, Miller TR, Hanzlick RL, et al. Leading causes of unintentional and intentional injury mortality: United States, 2000–2009. Am J Public Health. 2012;102:e84–92.
Bagge CL, Lamis DA, Nadorff M, Osman A. Relations between hopelessness, depressive symptoms and suicidality: mediation by reasons for living. J Clin Psychol. 2014;70:18–31. Outlines the protective factors for suicidal ideation, with the Reasons for Living construct of primary importance.
McPhedran S, Baker J. Recent Australian suicide trends for males and females at the national level: has the rate of decline differed? Health Policy. 2008;87:350–8.
Mendoza J Rosenberg S. Suicide and suicide prevention in Australia breaking the silence. Lifeline Australia: Suicide Prevention Australia. 2010. http://suicidepreventionaust.org/Resources.aspx.
Hawton K, van Heeringen K. Suicide. Lancet. 2009;373:1372–81. Comprehensive overview of the major risk factors for suicide in the general population.
Moscicki E. Gender differences in completed and attempted suicides. Ann Epidemiol. 1994;4:152–8.
Callanan VJ, Davis MS. Gender differences in suicide methods. Soc Psychiatry Psychiatr Epidemiol. 2012;47:857–69.
Garlow SJ, Purselle D, Heninger M. Ethnic differences in patterns of suicide across the life cycle. Am J Psychiatry. 2005;162:319–23.
Smith JC, Mercy JA, Conn JM. Marital status and the risk of suicide. Am J Public Health. 1988;78:78–80.
Picardi A, Lega I, Tarolla E. Suicide risk in skin disorders. Clin Dermatol. 2013;31:47–56.
Blakely TA, Collings SC, Atkinson J. Unemployment and suicide. Evidence for a causal association? J Epidemiol Community Health. 2003;57:594–600.
Enns MW, Cox BJ, Afifi TO, De Graaf R, ten Have M, Sareen J. Childhood adversities and risk for suicidal ideation and attempts: a longitudinal population-based study. Psychol Med. 2006;36:1769–78.
Bruffaerts R, Demyttenaere K, Borges G, Haro JM, Chiu WT, Hwang I, et al. Childhood adversities as risk factors for onset and persistence of suicidal behavior. Br J Psychiatry. 2010;197:20–7.
Hawton K, Casañas i Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147:17–28.
Hirokawa S, Matsumoto T, Katsumata Y, Kitani M, Akazawa M, Takahashi Y, et al. Psychosocial and psychiatric characteristics of suicide completers with psychiatric treatment before death: a psychological autopsy study of 76 cases. Psychiatry Clin Neurosci. 2012;66:292–302.
Brady J. The association between alcohol misuse and suicidal behavior. Alcohol Alcohol. 2006;41:473–8.
Stack S. Suicide: a 15-year review of the sociological literature. Part II: modernization and social integration perspectives. Suicide Life Threat Behav. 2000;30:163–76.
Nielsen DA, Virkkunen M, Lappaleinen J, et al. A tryptophan hydroxylase gene marker for suicidality and alcoholism. Arch Gen Psychiatry. 1998;55:593–602.
Liu RT, Miller I. Life events and suicidal ideation and behavior: a systematic review. Clin Psychol Rev. 2014;4(34):181–92.
Borges G, Nock MK, Abad JMH, Hwang I, Sampson NA, Alonso J, et al. Twelve month prevalence of and risk factors for suicide attempts in the WHO World Mental Health Surveys. J Clin Psychiatry. 2010;71:1617.
Meier DE, Emmons CA, Litke A, Wallenstein S, Morrison RS. Characteristics of patients requesting and receiving physician-assisted death. Arch Intern Med. 2003;163:1537–42.
Smith MT, Edwards RR, Robinson RC, Dworkin RH. Suicidal ideation, plans, and attempts in chronic pain patients: factors associated with increased risk. Pain. 2004;111:201–8.
Hitchcock LS, Ferrell BR, McCaffery M. The experience of chronic nonmalignant pain. J Pain Symptom Manag. 1994;9:312–8.
Tang NK, Crane C. Suicidality in chronic pain: a review of the prevalence, risk factors and psychological links. Psychol Med. 2006;36:575–86.
Fishbain DA, Goldberg M, Rosomoff RS, Rosomoff H. Completed suicide in chronic pain. Clin J Pain. 1991;7:29–36.
Ilgen MA, Kleinberg F, Ignacio RV, Bohnert AS, Valenstein M, McCarthy JF, et al. Noncancer pain conditions and risk of suicide. JAMA Psychiatry. 2013;70:692–7. Large epidemiologic investigation of risk factors for completed suicide in the chronic pain population.
Marzuk PM, Leon AC, Tardiff K, Morgan EB, Stajic M, Mann JJ. The effect of access to lethal methods of injury on suicide rates. Arch Gen Psychiatry. 1992;49:451–8.
Saffier K, Colombo C, Brown D, Mundt MP, Fleming MF. Addiction Severity Index in a chronic pain sample receiving opioid therapy. J Subst Abus Treat. 2007;33:303–11.
Ho PT, Li CF, Ng YK, Tsui SL, Ng KFJ. Prevalence of and factors associated with psychiatric morbidity in chronic pain patients. J Psychosom Res. 2011;70:541–7.
Salazar A, Dueñas M, Mico JA, Ojeda B, Agüera‐Ortiz L, Cervilla JA, et al. Undiagnosed mood disorders and sleep disturbances in primary care patients with chronic musculoskeletal pain. Pain Med. 2013;14:1416–25.
Braden JB, Sullivan MD. Suicidal thoughts and behavior among adults with self-reported pain conditions in the national comorbidity survey replication. J Pain. 2008;9:1106–15.
Ilgen MA, Zivin K, McCammon RJ, Valenstein M. Pain and suicidal thoughts, plans and attempts in the United States. Gen Hosp Psychiatry. 2008;30:521–7.
Rainville J, Sobel JB, Hartigan C, Wright A. The effect of compensation involvement on the reporting of pain and disability by patients referred for rehabilitation of chronic low back pain. Spine. 1997;22:2016–24.
Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner Jr TE. The interpersonal theory of suicide. Psychol Rev. 2010;117:575.
Wilson KG, Kowal J, Henderson PR, McWilliams LA, Péloquin K. Chronic pain and the interpersonal theory of suicide. Rehabil Psychol. 2013;58:111. Important addition to the chronic pain risk factor research, as this study provides a conceptual understanding of suicidal ideation in this patient group.
Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Int Med. 2003;163:2433–45.
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92.
Gould MS, Marrocco FA, Kleinman M, Thomas JG, Mostkoff K, Cote J, et al. Evaluating iatrogenic risk of youth suicide screening programs: a randomized controlled trial. JAMA. 2005;293:1635–43.
Linehan MM, Goodstein JL, Nielsen SL, Chiles JA. Reasons for staying alive when you are thinking of killing yourself: the reasons for living inventory. J Consult Clin Psychol. 1983;51:276.
Gutierrez PM, Osman A, Barrios FX, Kopper BA, Baker MT, Haraburda CM. Development of the reasons for living inventory for young adults. J Clin Psychol. 2002;58:339–57.
Dogra AK, Basu S, Das S. Impact of meaning in life and reasons for living to hope and suicidal ideation: a study among college students. SIS J Project Psychol Ment Health. 2011;18(1):89–102.
Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44:1–25.
McCracken LM, Vowles KE. Acceptance and commitment therapy and mindfulness for chronic pain: model, process, and progress. Am Psychol. 2014;69:178. Detailed overview of the ACT approach as applied to chronic pain, and a summary of the outcome literature as it currently stands.
Kabat-Zinn J. Mindfulness‐based interventions in context: past, present, and future. Clin Psychol Sci Pract. 2003;10:144–56.
Veehof MM, Oskam MJ, Schreurs KMG, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: a systematic review and meta-analysis. Pain. 2011;152:533–42.
Vowles KE, McCracken LM, Zhao-O’Brien J. Acceptance and values-based action in chronic pain: a three year follow-up analysis of treatment effectiveness and process. Behav Res Ther. 2011;49:748–55.
You S, Van Orden KA, Conner KR. Social connections and suicidal thoughts and behavior. Psychol Addict Behav. 2011;25:180.
Compliance with Ethics Guidelines
Conflict of Interest
Toby Newton-John declares that he has no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Psychiatric Management of Pain
Rights and permissions
About this article
Cite this article
Newton-John, T.R.O. Negotiating the Maze: Risk Factors for Suicidal Behavior in Chronic Pain Patients. Curr Pain Headache Rep 18, 447 (2014). https://doi.org/10.1007/s11916-014-0447-y
Published:
DOI: https://doi.org/10.1007/s11916-014-0447-y