Abstract
Purpose of Review
The purpose of this review is to summarize the recently published scientific literature regarding the effects of mitochondrial function and mitochondrial genome mutations on bone phenotype and aging.
Recent Findings
While aging and sex steroid levels have traditionally been considered the most important risk factors for development of osteoporosis, mitochondrial function and genetics are being increasingly recognized as important determinants of bone health. Recent studies indicate that mitochondrial genome variants found in different human populations determine the risk of complex degenerative diseases. We propose that osteoporosis should be among such diseases. Studies have shown the deleterious effects of mitochondrial DNA mutations and mitochondrial dysfunction on bone homeostasis. Mediators of such effects include oxidative stress, mitochondrial permeability transition, and dysregulation of autophagy.
Summary
Mitochondrial health plays an important role in bone homeostasis and aging, and understanding underlying mechanisms is critical in leveraging this relationship clinically for therapeutic benefit.

Similar content being viewed by others
Data Availability
Not applicable
Code Availability
Not applicable
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• LeBoff MS, Greenspan SL, Insogna KL, Lewiecki EM, Saag KG, Singer AJ, et al. The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022;33(10):2049–102. https://doi.org/10.1007/s00198-021-05900-y. This is a comprehensive review of current state of osteoporosis research and clinical management.
Sözen T, Özışık L, Başaran N. An overview and management of osteoporosis. Eur J Rheumatol. 2017;4(1):46–56. https://doi.org/10.5152/eurjrheum.2016.048.
Rashki Kemmak A, Rezapour A, Jahangiri R, Nikjoo S, Farabi H, Soleimanpour S. Economic burden of osteoporosis in the world: a systematic review. Med J Islam Repub Iran. 2020;34:154. https://doi.org/10.34171/mjiri.34.154.
Noh JY, Yang Y, Jung H. Molecular mechanisms and emerging therapeutics for osteoporosis. Int J Mol Sci. 2020;21(20) https://doi.org/10.3390/ijms21207623.
Su N, Yang J, Xie Y, Du X, Chen H, Zhou H, et al. Bone function, dysfunction and its role in diseases including critical illness. Int J Biol Sci. 2019;15(4):776–87. https://doi.org/10.7150/ijbs.27063.
Nayak S, Greenspan SL. Osteoporosis treatment efficacy for men: a systematic review and meta-analysis. J Am Geriatr Soc. 2017;65(3):490–5. https://doi.org/10.1111/jgs.14668.
Almeida M, O'Brien CA. Basic biology of skeletal aging: role of stress response pathways. J Gerontol A Biol Sci Med Sci. 2013;68(10):1197–208. https://doi.org/10.1093/gerona/glt079.
Wallace DC. A mitochondrial bioenergetic etiology of disease. J Clin Invest. 2013;123(4):1405–12. https://doi.org/10.1172/jci61398.
•• Brown JA, Sammy MJ, Ballinger SW. An evolutionary, or “mitocentric” perspective on cellular function and disease. Redox Biol. 2020;36:101568. https://doi.org/10.1016/j.redox.2020.101568. Recent review of the role of mitochondrial genetics and function in aging of various non-skeletal tissues.
McKinney EA, Oliveira MT. Replicating animal mitochondrial DNA. Genet Mol Biol. 2013;36(3):308–15. https://doi.org/10.1590/s1415-47572013000300002.
Clay Montier LL, Deng JJ, Bai Y. Number matters: control of mammalian mitochondrial DNA copy number. J Genet Genomics. 2009;36(3):125–31. https://doi.org/10.1016/s1673-8527(08)60099-5.
Atilano SR, Malik D, Chwa M, Cáceres-Del-Carpio J, Nesburn AB, Boyer DS, et al. Mitochondrial DNA variants can mediate methylation status of inflammation, angiogenesis and signaling genes. Hum Mol Genet. 2015;24(16):4491–503. https://doi.org/10.1093/hmg/ddv173.
Kopinski PK, Janssen KA, Schaefer PM, Trefely S, Perry CE, Potluri P, et al. Regulation of nuclear epigenome by mitochondrial DNA heteroplasmy. Proc Natl Acad Sci U S A. 2019;116(32):16028–35. https://doi.org/10.1073/pnas.1906896116.
Wallace DC. Mitochondrial genetic medicine. Nat Genet. 2018;50(12):1642–9. https://doi.org/10.1038/s41588-018-0264-z.
Balloux F, Handley LJ, Jombart T, Liu H, Manica A. Climate shaped the worldwide distribution of human mitochondrial DNA sequence variation. Proc Biol Sci. 2009;276(1672):3447–55. https://doi.org/10.1098/rspb.2009.0752.
Kazuno AA, Munakata K, Nagai T, Shimozono S, Tanaka M, Yoneda M, et al. Identification of mitochondrial DNA polymorphisms that alter mitochondrial matrix pH and intracellular calcium dynamics. PLoS Genet. 2006;2(8):e128. https://doi.org/10.1371/journal.pgen.0020128.
Wallace DC. Mitochondrial DNA variation in human radiation and disease. Cell. 2015;163(1):33–8. https://doi.org/10.1016/j.cell.2015.08.067.
Leonard WR, Sorensen MV, Galloway VA, Spencer GJ, Mosher MJ, Osipova L, et al. Climatic influences on basal metabolic rates among circumpolar populations. Am J Hum Biol. 2002;14(5):609–20. https://doi.org/10.1002/ajhb.10072.
Snodgrass JJ, Leonard WR, Sorensen MV, Tarskaia LA, Mosher MJ. The influence of basal metabolic rate on blood pressure among indigenous Siberians. Am J Phys Anthropol. 2008;137(2):145–55. https://doi.org/10.1002/ajpa.20851.
Kenney MC, Chwa M, Atilano SR, Falatoonzadeh P, Ramirez C, Malik D, et al. Molecular and bioenergetic differences between cells with African versus European inherited mitochondrial DNA haplogroups: implications for population susceptibility to diseases. Biochimica et Biophysica Acta. 2014;1842(2):208–19. https://doi.org/10.1016/j.bbadis.2013.10.016.
Barrett-Connor E, Siris ES, Wehren LE, Miller PD, Abbott TA, Berger ML, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2005;20(2):185–94. https://doi.org/10.1359/jbmr.041007.
National Diabetes Statistics Report. https://www.cdc.gov/diabetes/data/statistics-report/index.html (2022). Accessed April 25, 2023 2023.
Roshal D, Glosser D, Zangaladze A. Parieto-occipital lobe epilepsy caused by a POLG1 compound heterozygous A467T/W748S genotype. Epilepsy Behav. 2011;21(2):206–10. https://doi.org/10.1016/j.yebeh.2011.03.003.
Chan SS, Longley MJ, Copeland WC. The common A467T mutation in the human mitochondrial DNA polymerase (POLG) compromises catalytic efficiency and interaction with the accessory subunit. J Biol Chem. 2005;280(36):31341–6. https://doi.org/10.1074/jbc.M506762200.
De Block CE, De Leeuw IH, Maassen JA, Ballaux D, Martin JJ. A novel 7301-bp deletion in mitochondrial DNA in a patient with Kearns-Sayre syndrome, diabetes mellitus, and primary amenorrhoea. Exp Clin Endocrinol Diabetes. 2004;112(2):80–3. https://doi.org/10.1055/s-2004-815754.
Flanagan D, CRNA A, Hicks L. Anesthetic management of a patient with mitochondrial encephalopathy, lactic acidosis and stroke-like symptoms (MELAS): a case study. Anesth J. 2016;4(1)
Maslow A, Lisbon A. Anesthetic considerations in patients with mitochondrial dysfunction. Anesth Analg. 1993;76(4):884–6. https://doi.org/10.1213/00000539-199304000-00035.
Blair MT, Heard G. Neuraxial anaesthesia in MELAS syndrome. Anaesth Intensive Care. 2011;39(6):1152–3.
Du Y, Jiang B, Li K, Chen Y, He J. Leber hereditary optic neuropathy in a boy with fibrous boney dysplasia. Eye Sci. 2013;28(1):48–50.
Hayashi S, Okamoto K. Leber’s hereditary optic neuropathy after head trauma: a case report. Rinsho Shinkeigaku. 2011;51(10):781–3. https://doi.org/10.5692/clinicalneurol.51.781.
Manickam AH, Michael MJ, Ramasamy S. Mitochondrial genetics and therapeutic overview of Leber’s hereditary optic neuropathy. Indian J Ophthalmol. 2017;65(11):1087–92. https://doi.org/10.4103/ijo.IJO_358_17.
Diab M. Self-inflicted orodental injury in a child with Leigh disease. Int J Paediatr Dent. 2004;14(1):73–7. https://doi.org/10.1111/j.1365-263x.2004.00472.x.
Schubert Baldo M, Vilarinho L. Molecular basis of Leigh syndrome: a current look. Orphanet J. Rare Dis. 2020;15(1):31. https://doi.org/10.1186/s13023-020-1297-9.
Monroy N, Macías Kauffer LR, Mutchinick OM. Mitochondrial neurogastrointestinal encephalomyopathy (MNGIE) in two Mexican brothers harboring a novel mutation in the ECGF1 gene. Eur J Med Genet. 2008;51(3):245–50. https://doi.org/10.1016/j.ejmg.2007.12.007.
Fetterman JL, Zelickson BR, Johnson LW, Moellering DR, Westbrook DG, Pompilius M, et al. Mitochondrial genetic background modulates bioenergetics and susceptibility to acute cardiac volume overload. Biochem J. 2013;455(2):157–67. https://doi.org/10.1042/bj20130029.
Guntur AR, Le PT, Farber CR, Rosen CJ. Bioenergetics during calvarial osteoblast differentiation reflect strain differences in bone mass. Endocrinology. 2014;155(5):1589–95. https://doi.org/10.1210/en.2013-1974.
Latorre-Pellicer A, Moreno-Loshuertos R, Lechuga-Vieco AV, Sánchez-Cabo F, Torroja C, Acín-Pérez R, et al. Mitochondrial and nuclear DNA matching shapes metabolism and healthy ageing. Nature. 2016;535(7613):561–5. https://doi.org/10.1038/nature18618.
Bouxsein ML, Myers KS, Shultz KL, Donahue LR, Rosen CJ, Beamer WG. Ovariectomy-induced bone loss varies among inbred strains of mice. J Bone Miner Res. 2005;20(7):1085–92. https://doi.org/10.1359/jbmr.050307.
Buie HR, Moore CP, Boyd SK. Postpubertal architectural developmental patterns differ between the L3 vertebra and proximal tibia in three inbred strains of mice. J Bone Miner Res. 2008;23(12):2048–59. https://doi.org/10.1359/jbmr.080808.
Dunham-Snary KJ, Sandel MW, Sammy MJ, Westbrook DG, Xiao R, McMonigle RJ, et al. Mitochondrial - nuclear genetic interaction modulates whole body metabolism, adiposity and gene expression in vivo. EBioMedicine. 2018;36:316–28. https://doi.org/10.1016/j.ebiom.2018.08.036.
Harman D. The biologic clock: the mitochondria? J Am Geriatr Soc. 1972;20(4):145–7. https://doi.org/10.1111/j.1532-5415.1972.tb00787.x.
•• Amorim JA, Coppotelli G, Rolo AP, Palmeira CM, Ross JM, Sinclair DA. Mitochondrial and metabolic dysfunction in ageing and age-related diseases. Nat Rev Endocrinol. 2022;18(4):243–58. https://doi.org/10.1038/s41574-021-00626-7. Important review of cellular and whole tissue metabolic changes associated with aging.
Trifunovic A, Wredenberg A, Falkenberg M, Spelbrink JN, Rovio AT, Bruder CE, et al. Premature ageing in mice expressing defective mitochondrial DNA polymerase. Nature. 2004;429(6990):417–23. https://doi.org/10.1038/nature02517.
Mito T, Ishizaki H, Suzuki M, Morishima H, Ota A, Ishikawa K, et al. Transmitochondrial mito-miceΔ and mtDNA mutator mice, but not aged mice, share the same spectrum of musculoskeletal disorders. Biochem Biophys Res Commun. 2015;456(4):933–7. https://doi.org/10.1016/j.bbrc.2014.12.009.
Mito T, Tani H, Suzuki M, Ishikawa K, Nakada K, Hayashi JI. Mito-mice∆ and mitochondrial DNA mutator mice as models of human osteoporosis caused not by aging but by hyperparathyroidism. Exp Anim. 2018;67(4):509–16. https://doi.org/10.1538/expanim.18-0060.
Dobson PF, Dennis EP, Hipps D, Reeve A, Laude A, Bradshaw C, et al. Mitochondrial dysfunction impairs osteogenesis, increases osteoclast activity, and accelerates age related bone loss. Sci Rep. 2020;10(1):11643. https://doi.org/10.1038/s41598-020-68566-2.
Lin PI, Tai YT, Chan WP, Lin YL, Liao MH, Chen RM. Estrogen/ERα signaling axis participates in osteoblast maturation via upregulating chromosomal and mitochondrial complex gene expressions. Oncotarget. 2018;9(1):1169–86. https://doi.org/10.18632/oncotarget.23453.
Goropashnaya AV, Tøien Ø, Ramaraj T, Sundararajan A, Schilkey FD, Barnes BM, et al. Transcriptional changes and preservation of bone mass in hibernating black bears. Sci Rep. 2021;11(1):8281. https://doi.org/10.1038/s41598-021-87785-9.
Feigenson M, Eliseev RA, Jonason JH, Mills BN, O'Keefe RJ. PGE2 Receptor Subtype 1 (EP1) Regulates mesenchymal stromal cell osteogenic differentiation by modulating cellular energy metabolism. J Cell Biochem. 2017;118(12):4383–93. https://doi.org/10.1002/jcb.26092.
Shares BH, Busch M, White N, Shum L, Eliseev RA. Active mitochondria support osteogenic differentiation by stimulating β-catenin acetylation. J Biol Chem. 2018;293(41):16019–27. https://doi.org/10.1074/jbc.RA118.004102.
• Hollenberg AM, Smith CO, Shum LC, Awad H, Eliseev RA. Lactate dehydrogenase inhibition with oxamate exerts bone anabolic effect. J Bone Miner Res. 2020;35(12):2432–43. https://doi.org/10.1002/jbmr.4142. This study demonstrated a glycolytic shift and mitochondrial dysfunction in aged bone. Targeting these changes pharmacologically reversed bone loss during aging.
Huang T, Liu R, Fu X, Yao D, Yang M, Liu Q, et al. Aging reduces an ERRalpha-directed mitochondrial glutaminase expression suppressing glutamine anaplerosis and osteogenic differentiation of mesenchymal stem cells. Stem Cells. 2017;35(2):411–24. https://doi.org/10.1002/stem.2470.
Ling W, Krager K, Richardson KK, Warren AD, Ponte F, Aykin-Burns N, et al. Mitochondrial Sirt3 contributes to the bone loss caused by aging or estrogen deficiency. JCI Insight. 2021;6(10) https://doi.org/10.1172/jci.insight.146728.
Richardson KK, Ling W, Krager K, Fu Q, Byrum SD, Pathak R, et al. Ionizing radiation activates mitochondrial function in osteoclasts and causes bone loss in young adult male mice. Int J Mol Sci. 2022;23(2) https://doi.org/10.3390/ijms23020675.
Lee SH, Lee SH, Lee JH, Park JW, Kim JE. IDH2 deficiency increases bone mass with reduced osteoclastogenesis by limiting RANKL expression in osteoblasts. Bone. 2019;129:115056. https://doi.org/10.1016/j.bone.2019.115056.
Takeshima K, Nishiwaki Y, Suda Y, Niki Y, Sato Y, Kobayashi T, et al. A missense single nucleotide polymorphism in the ALDH2 gene, rs671, is associated with hip fracture. Sci Rep. 2017;7(1):428. https://doi.org/10.1038/s41598-017-00503-2.
Hoshi H, Monoe F, Ohsawa I, Ohta S, Miyamoto T. Astaxanthin improves osteopenia caused by aldehyde-stress resulting from Aldh2 mutation due to impaired osteoblastogenesis. Biochem Biophys Res Commun. 2020;527(1):270–5. https://doi.org/10.1016/j.bbrc.2020.04.013.
Bernardi P, Rasola A, Forte M, Lippe G. The mitochondrial permeability transition pore: channel formation by F-ATP synthase, integration in signal transduction, and role in pathophysiology. Physiol Rev. 2015;95(4):1111–55. https://doi.org/10.1152/physrev.00001.2015.
Zhen YF, Wang GD, Zhu LQ, Tan SP, Zhang FY, Zhou XZ, et al. P53 dependent mitochondrial permeability transition pore opening is required for dexamethasone-induced death of osteoblasts. J Cell Physiol. 2014;229(10):1475–83. https://doi.org/10.1002/jcp.24589.
Shum LC, White NS, Nadtochiy SM, Bentley KL, Brookes PS, Jonason JH, et al. Cyclophilin D Knock-out mice show enhanced resistance to osteoporosis and to metabolic changes observed in aging bone. PLoS One. 2016;11(5):e0155709. https://doi.org/10.1371/journal.pone.0155709.
• Shares BH, Smith CO, Sheu TJ, Sautchuk R Jr, Schilling K, Shum LC, et al. Inhibition of the mitochondrial permeability transition improves bone fracture repair. Bone. 2020;137:115391. https://doi.org/10.1016/j.bone.2020.115391. This study has shown that inhibition of the mitochondrial permeability transition pore accelerates bone fracture repair.
Shum LC, Hollenberg AM, Baldwin AL, Kalicharan BH, Maqsoodi N, Rubery PT, et al. Role of oxidative metabolism in osseointegration during spinal fusion. PLoS One. 2020;15(11):e0241998. https://doi.org/10.1371/journal.pone.0241998.
•• Sautchuk R, Kalicharan BH, Escalera-Rivera K, Jonason JH, Porter GA, Awad HA, et al. Transcriptional regulation of cyclophilin D by BMP/Smad signaling and its role in osteogenic differentiation. Elife. 2022;11 https://doi.org/10.7554/eLife.75023. This work demonstrates how osteogenic signaling (BMP) modulates mitochondrial integrity and function (MPTP activity) and why such a modulation is important for osteoprogenitors.
Sautchuk R Jr, Yu C, McArthur M, Massie C, Brookes PS, Porter GA Jr, et al. Role of the mitochondrial permeability transition in bone metabolism and aging. J Bone Miner Res. 2023;38(4):522–40. https://doi.org/10.1002/jbmr.4787.
Singh K, Krug L, Basu A, Meyer P, Treiber N, Vander Beken S, et al. Alpha-ketoglutarate curbs differentiation and induces cell death in mesenchymal stromal precursors with mitochondrial dysfunction. Stem Cells. 2017;35(7):1704–18. https://doi.org/10.1002/stem.2629.
Kobayashi K, Nojiri H, Saita Y, Morikawa D, Ozawa Y, Watanabe K, et al. Mitochondrial superoxide in osteocytes perturbs canalicular networks in the setting of age-related osteoporosis. Sci Rep. 2015;5:9148. https://doi.org/10.1038/srep09148.
• Behera J, Ison J, Rai H, Tyagi N. Allyl sulfide promotes osteoblast differentiation and bone density via reducing mitochondrial DNA release mediated Kdm6b/H3K27me3 epigenetic mechanism. Biochem Biophys Res Commun. 2021;543:87–94. https://doi.org/10.1016/j.bbrc.2021.01.016. This work connects mitochondrial activity in osteoblasts with epigenetic signaling.
Ucer S, Iyer S, Kim HN, Han L, Rutlen C, Allison K, et al. The effects of aging and sex steroid deficiency on the murine skeleton are independent and mechanistically distinct. J Bone Miner Res. 2017;32(3):560–74. https://doi.org/10.1002/jbmr.3014.
Jiang Z, Wang H, Qi G, Jiang C, Chen K, Yan Z. Iron overload-induced ferroptosis of osteoblasts inhibits osteogenesis and promotes osteoporosis: an in vitro and in vivo study. IUBMB Life. 2022;74(11):1052–69. https://doi.org/10.1002/iub.2656.
Das BK, Wang L, Fujiwara T, Zhou J, Aykin-Burns N, Krager KJ, et al. Transferrin receptor 1-mediated iron uptake regulates bone mass in mice via osteoclast mitochondria and cytoskeleton. Elife. 2022;11:e73539. https://doi.org/10.7554/eLife.73539.
Gan X, Huang S, Yu Q, Yu H, Yan SS. Blockade of Drp1 rescues oxidative stress-induced osteoblast dysfunction. Biochem Biophys Res Commun. 2015;468(4):719–25. https://doi.org/10.1016/j.bbrc.2015.11.022.
Danics L, Abbas AA, Kis B, Pircs K. Fountain of youth—targeting autophagy in aging. Front Aging Neurosci. 2023;15:1125739. https://doi.org/10.3389/fnagi.2023.1125739.
Manolagas SC. From estrogen-centric to aging and oxidative stress: a revised perspective of the pathogenesis of osteoporosis. Endocr Rev. 2010;31(3):266–300. https://doi.org/10.1210/er.2009-0024.
Yang YH, Li B, Zheng XF, Chen JW, Chen K, Jiang SD, et al. Oxidative damage to osteoblasts can be alleviated by early autophagy through the endoplasmic reticulum stress pathway—implications for the treatment of osteoporosis. Free Radic Biol Med. 2014;77:10–20. https://doi.org/10.1016/j.freeradbiomed.2014.08.028.
Li W, Jiang WS, Su YR, Tu KW, Zou L, Liao CR, et al. PINK1/Parkin-mediated mitophagy inhibits osteoblast apoptosis induced by advanced oxidation protein products. Cell Death Dis. 2023;14(2):88. https://doi.org/10.1038/s41419-023-05595-5.
Sun X, Yang X, Zhao Y, Li Y, Guo L. Effects of 17β-estradiol on mitophagy in the murine MC3T3-E1 osteoblast cell line is mediated via G protein-coupled estrogen receptor and the ERK1/2 signaling pathway. Med Sci Monit. 2018;24:903–11. https://doi.org/10.12659/msm.908705.
Kim HN, Ponte F, Nookaew I, Ucer Ozgurel S, Marques-Carvalho A, Iyer S, et al. Estrogens decrease osteoclast number by attenuating mitochondria oxidative phosphorylation and ATP production in early osteoclast precursors. Sci Rep. 2020;10(1):11933. https://doi.org/10.1038/s41598-020-68890-7.
Piemontese M, Onal M, Xiong J, Han L, Thostenson JD, Almeida M, et al. Low bone mass and changes in the osteocyte network in mice lacking autophagy in the osteoblast lineage. Sci Rep. 2016;6:24262. https://doi.org/10.1038/srep24262.
Aoki S, Shimizu K, Ito K. Autophagy-dependent mitochondrial function regulates osteoclast differentiation and maturation. Biochem Biophys Res Commun. 2020;527(4):874–80. https://doi.org/10.1016/j.bbrc.2020.04.155.
Chen YH, Peng SY, Cheng MT, Hsu YP, Huang ZX, Cheng WT, et al. Different susceptibilities of osteoclasts and osteoblasts to glucocorticoid-induced oxidative stress and mitochondrial alterations. Chin J Physiol. 2019;62(2):70–9. https://doi.org/10.4103/cjp.Cjp_7_19.
Funding
R. A. E. is supported by NIH grants R01 AR072601, R01 AG076786, and R21 AR080291.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
All reported data coming from human and animal studies performed by the authors have been previously published and complied with all applicable ethical standards including the Helsinki declaration and its amendments, institutional/national research committee standards, and guidelines.
Additional information
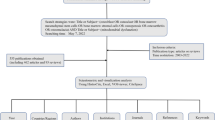
All figures and tables are original and never published before. Parts of Fig. 1 were made using Biorender.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Catheline, S.E., Kaiser, E. & Eliseev, R.A. Mitochondrial Genetics and Function as Determinants of Bone Phenotype and Aging. Curr Osteoporos Rep 21, 540–551 (2023). https://doi.org/10.1007/s11914-023-00816-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-023-00816-4