Abstract
Purpose of Review
Since the beginning of the coronavirus disease 2019 pandemic, many lasting neurological sequelae including cognitive impairment have been recognized as part of the so-called long COVID syndrome. This narrative review summarizes the cognitive aspects of COVID-19.
Recent Findings
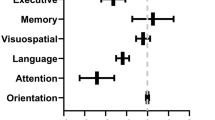
Studies have consistently identified attention, memory, and executive functions as the cognitive domains most often affected by COVID-19 infection. Many studies have also reported neuroimaging, biofluid, and neurophysiological abnormalities that could potentially reflect the pathophysiological aspects of post-COVID cognitive impairment. While patients suffering from dementia have an elevated risk of COVID-19 infection, increasing evidence has also indicated that COVID-19 infection may increase the risks of Alzheimer’s disease, suggesting bidirectional relationships.
Summary
Post-COVID cognitive dysfunction is a pervasive and multifaceted problem and we are surely in our infancy of understanding. Future elucidation into the long-term effects, mechanisms, and therapies will depend on a concerted effort from clinicians, researchers, patients, and policy-makers alike.
Similar content being viewed by others
Data Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
WHO coronavirus (COVID-19) dashboard with vaccination data [Cited 20 May 2023.] Available from URL: https://covid19.who.int/
• Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27:601–15. https://doi.org/10.1038/s41591-021-01283-z. This comprehensive review summarized the epidemiology, organ-specific manifestations, and interdisciplinary comprehensive management considerations for post-acute COVID-19 syndrome.
Long COVID or post-COVID conditions. https://www.cdc.gov/coronavirus/2019-ncov/long-termeffects/index.html?s_cid=11840:long/20covid/20definition:sem.ga:p:RG:GM:gen: PTN:FY23
• Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms, and recommendations. Nat Rev Microbiol. 2023;21:133–46. https://doi.org/10.1038/s41579-022-00846-2. This review article summarized the current knowledge base of long COVID and misconceptions surrounding long COVID.
Liotta EM, Batra A, Clark JR, Shlobin NA, Hoffman SC, Orban ZS, et al. Frequent neurologic manifestations and encephalopathy-associated morbidity in COVID-19 patients. Ann Clin Transl Neurol. 2020;7:2221–30. https://doi.org/10.1002/acn3.51210.
Xu E, Xie Y, Al-Aly Z. Long-term neurologic outcomes of COVID-19. Nat Med. 2022;28:2406–15. https://doi.org/10.1038/s41591-022-02001-z.
Rass V, Beer R, Schiefecker AJ, Lindner A, Kofler M, Andre Ianosi B, et al. Neurological outcomes 1 year after COVID-19 diagnosis: a prospective longitudinal cohort study. Eur J Neurol. 2022;29:1685–96. https://doi.org/10.1111/ene.15307.
Kubota T, Kuroda N, Sone D. Neuropsychiatric aspects of long COVID: a comprehensive review. Psychiatry Clin Neurosci. 2023;77:84–93. https://doi.org/10.1111/pcn.13508.
•• Monje M, Iwasaki A. The neurobiology of long COVID. Neuron. 2022;110:3484–96. https://doi.org/10.1016/j.neuron.2022.10.006. This comprehensive review proposed six potential mechanisms of COVID-19-induced neural injury.
Leng A, Shah M, Ahmad SA, Premraj L, Wildi K, Li Bassi G, et al. Pathogenesis underlying neurological manifestations of long COVID syndrome and potential therapeutics. Cells. 2023;12:816. https://doi.org/10.3390/cells12050816.
García-Grimshaw M, Chirino-Pérez A, Flores-Silva FD, Valdés-Ferrer SI, Vargas-Martínez MLA, Jiménez-Ávila AI, et al. Critical role of acute hypoxemia on the cognitive impairment after severe COVID-19 pneumonia: a multivariate causality model analysis. Neurol Sci. 2022;43:2217–29. https://doi.org/10.1007/s10072-021-05798-8.
•• Fernández-Castañeda A, Lu P, Geraghty AC, Song E, Lee MH, Wood J, et al. Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation. Cell. 2022;185:2452-2468.e16. https://doi.org/10.1016/j.cell.2022.06.008. This is a milestone study that reported evidence of impaired hippocampal neurogenesis, decreased oligodendrocytes, myelin loss, and elevated CSF cytokines/chemokines in mice with mild respiratory COVID.
Venkataramani V, Winkler F. Cognitive deficits in long COVID-19. N Engl J Med. 2022;387:1813–5. https://doi.org/10.1056/NEJMcibr2210069.
Soung AL, Vanderheiden A, Nordvig AS, Sissoko CA, Canoll P, Mariani MB, et al. COVID-19 induces CNS cytokine expression and loss of hippocampal neurogenesis. Brain. 2022;145:4193–201. https://doi.org/10.1093/brain/awac270.
•• Crivelli L, Palmer K, Calandri I, Guekht A, Beghi E, Carroll W, et al. Changes in cognitive functioning after COVID-19: a systematic review and meta-analysis. Alzheimers Dement. 2022;18:1047–66. https://doi.org/10.1002/alz.12644. This article provided a comprehensive systematic review and meta-analysis of COVID-19-associated cognitive dysfunction including literature up to the end of 2021.
Velichkovsky BB, Razvaliaeva AY, Khlebnikova AA, Manukyan PA, Kasatkin VN. Attention and memory after COVID-19 as measured by neuropsychological tests: systematic review and meta-analysis. Acta Psychol (Amst). 2023;233:103838. https://doi.org/10.1016/j.actpsy.2023.103838.
Tavares-Júnior JWL, de Souza ACC, Borges JWP, Oliveira DN, Siqueira-Neto JI, Sobreira-Neto MA, et al. COVID-19 associated cognitive impairment: a systematic review. Cortex. 2022;152:77–97. https://doi.org/10.1016/j.cortex.2022.04.006.
Bertuccelli M, Ciringione L, Rubega M, Bisiacchi P, Masiero S, Del Felice A. Cognitive impairment in people with previous COVID-19 infection: a scoping review. Cortex. 2022;154:212–30. https://doi.org/10.1016/j.cortex.2022.06.002.
Biagianti B, Di Liberto A, NicolòEdoardo A, Lisi I, Nobilia L, de Ferrabonc GD, et al. Cognitive assessment in SARS-CoV-2 patients: a systematic review. Front Aging Neurosci. 2022;14:909661. https://doi.org/10.3389/fnagi.2022.909661.
Badenoch JB, Rengasamy ER, Watson C, Jansen K, Chakraborty S, Sundaram RD, et al. Persistent neuropsychiatric symptoms after COVID-19: a systematic review and meta-analysis. Brain Commun. 2021;4:fcab297. https://doi.org/10.1093/braincomms/fcab297.
Houben S, Bonnechère B. The impact of COVID-19 infection on cognitive function and the implication for rehabilitation: a systematic review and meta-analysis. Int J Environ Res Public Health. 2022;19:7748. https://doi.org/10.3390/ijerph19137748.
Serena S, Deborah P, Anja F, Gwendolyn G, Puhan MA, Albanese E. Association between serologically confirmed COVID-19 infection and cognitive functioning in community dwelling older adults. Front Neurol. 2023;14:1093852. https://doi.org/10.3389/fneur.2023.1093852.
•• Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022;604(7907):697–707. https://doi.org/10.1038/s41586-022-04569-5. This is a milestone study that demonstrated MRI evidence of structural brain change including reduction of global brain volume, gray matter thickness, and markers of brain damage in selected brain areas in patients with COVID-19 compared to control cases.
Cecchetti G, Agosta F, Canu E, Basaia S, Barbieri A, Cardamone R, et al. Cognitive, EEG, and MRI features of COVID-19 survivors: a 10-month study. J Neurol. 2022;269:3400–12. https://doi.org/10.1007/s00415-022-11047-5.
Petersen M, N€agele FL, Mayer C, Schell, M, Petersen E, K€uhn S, et al. Brain imaging and neuropsychological assessment of individuals recovered from mild to moderate SARS-CoV-2 infection. Proc Natl Acad Sci USA. 2023; 120: e2217232120. https://doi.org/10.1073/pnas.2217232120.
Caroli A, Capelli S, Napolitano A, Cabrini G, Arrigoni A, Pezzetti G, et al. Brain diffusion alterations in patients with COVID-19 pathology and neurological manifestations. Neuroimage Clin. 2023;37:103338. https://doi.org/10.1016/j.nicl.2023.103338.
Ortelli P, Ferrazzoli D, Sebastianelli L, Maestri R, Dezi S, Spampinato D, et al. Altered motor cortex physiology and dysexecutive syndrome in patients with fatigue and cognitive difficulties after mild COVID-19. Eur J Neurol. 2022;29:1652–62. https://doi.org/10.1111/ene.15278.
Ajčević M, Iscra K, Furlanis G, Michelutti M, Miladinović A, Buoite Stella A, et al. Cerebral hypoperfusion in post-COVID-19 cognitively impaired subjects revealed by arterial spin labeling MRI. Sci Rep. 2023;13:5808. https://doi.org/10.1038/s41598-023-32275-3.
de Paula JJ, Paiva RERP, Souza-Silva NG, Rosa DV, Duran FLS, Coimbra RS, et al. Selective visuoconstructional impairment following mild COVID-19 with inflammatory and neuroimaging correlation findings. Mol Psychiatry. 2023;28:553–63. https://doi.org/10.1038/s41380-022-01632-5.
Franke C, Boesl F, Goereci Y, Gerhard A, Schweitzer F, Schroeder M, et al. Association of cerebrospinal fluid brain-binding autoantibodies with cognitive impairment in post-COVID-19 syndrome. Brain Behav Immun. 2023;109:139–43. https://doi.org/10.1016/j.bbi.2023.01.006.
Apple AC, Oddi A, Peluso MJ, Asken BM, Henrich TJ, Kelly JD, et al. Risk factors and abnormal cerebrospinal fluid associate with cognitive symptoms after mild COVID-19. Ann Clin Transl Neurol. 2022;9:221–6. https://doi.org/10.1002/acn3.51498.
Furlanis G, Buoite Stella A, Biaduzzini F, Bellavita G, Frezza NA, et al. Cognitive deficit in post-acute COVID-19: an opportunity for EEG evaluation? Neurol Sci. 2023;44:1491–8. https://doi.org/10.1007/s10072-023-06615-0.
Hariyanto TI, Putri C, Arisa J, Situmeang RFV, Kurniawan A. Dementia and outcomes from coronavirus disease 2019 (COVID-19) pneumonia: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2021;93:104299. https://doi.org/10.1016/j.archger.2020.104299.
Rolland Y, Baziard M, De Mauleon A, Dubus E, Saidlitz P, Soto ME. Coronavirus disease-2019 in older people with cognitive impairment. Clin Geriatr Med. 2022;38:501–17. https://doi.org/10.1016/j.cger.2022.03.002.
•• Toniolo S, Scarioni M, Di Lorenzo F, Hort J, Georges J, Tomic S, et al. Dementia and COVID-19, a bidirectional liaison: risk factors, biomarkers, and optimal health care. J Alzheimers Dis. 2021;82:883–98. https://doi.org/10.3233/JAD-210335. This article reviewed literature with evidence indicating COVID-19 may be more prevalent in patients with dementia and cognitive impairment and COVID-19 may increase risks of developing Alzheimer’s disease and related dementia and the potential mechanisms.
• Wang Y, Li M, Kazis LE, Xia W. Clinical outcomes of COVID-19 infection among patients with Alzheimer’s disease or mild cognitive impairment. Alzheimers Dement. 2022;18:911–23. https://doi.org/10.1002/alz.12665. This cohort study of 436,823 veterans demonstrated increased risks of COVID-19 infection and mortality among subjects with Alzheimer’s disease.
Matsui T, Mitsuma S, Nagata A, Matsushita A, Asahi T. Accelerated cognitive decline after the COVID-19 pandemic in a community population of older persons with cognitive impairment: a 4-year time series analysis in the Tokyo Metropolis area. Geriatr Gerontol Int. 2023;23:200–4. https://doi.org/10.1111/ggi.14543.
Merla L, Montesi MC, Ticali J, Bais B, Cavarape A, Colussi G. COVID-19 accelerated cognitive decline in elderly patients with pre-existing dementia followed up in an outpatient memory care facility. J Clin Med. 2023;12:1845. https://doi.org/10.3390/jcm12051845.
• Olivera E, Sáez A, Carniglia L, Caruso C, Lasaga M, Durand D. Alzheimer’s disease risk after COVID-19: a view from the perspective of the infectious hypothesis of neurodegeneration. Neural Regen Res. 2023;18:1404–10. https://doi.org/10.4103/1673-5374.360273. This review article summarized literature with evidence indicating COVID-19 infection may increase the risks of Alzheimer’s disease and the potential pathophysiological mechanisms.
Ciaccio M, Lo Sasso B, Scazzone C, Gambino CM, Ciaccio AM, Bivona G, et al. COVID-19 and Alzheimer’s Disease. Brain Sci. 2021;11:305. https://doi.org/10.3390/brainsci11030305.
Rahman MA, Islam K, Rahman S, Alamin M. Neurobiochemical cross-talk between COVID-19 and Alzheimer’s disease. Mol Neurobiol. 2021;58:1017–23. https://doi.org/10.1007/s12035-020-02177-w.
•• Reiken S, Sittenfeld L, Dridi H, Liu Y, Liu X, Marks AR. Alzheimer’s-like signaling in brains of COVID-19 patients. Alzheimers Dement. 2022;18:955–65. https://doi.org/10.1002/alz.12558. This original study provided evidence linking SARS-CoV-2 infection to neuropathological abnormalities typically associated with AD, including activation of TGF-β signaling and oxidative overload, as well as tau hyperphosphorylation.
Kuo CL, Pilling LC, Atkins JL, Masoli JAH, Delgado J, Kuchel GA, et al. APOE e4 genotype predicts severe COVID-19 in the UK Biobank Community Cohort. J Gerontol A Biol Sci Med Sci. 2020;75:2231–2. https://doi.org/10.1093/gerona/glaa131.
Nouraeinejad A. The functional and structural changes in the hippocampus of COVID-19 patients. Acta Neurol Belg. 2023;25:1–10. https://doi.org/10.1007/s13760-023-02291-1.
Wang L, Davis PB, Volkow ND, Berger NA, Kaelber DC, Xu R. Association of COVID-19 with new-onset Alzheimer’s disease. J Alzheimers Dis. 2022;89:411–4. https://doi.org/10.3233/JAD-220717.
Funding
This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Ezekiel Gonzalez-Fernandez and Juebin Huang wrote the main manuscript text. Juebin Huang reviewed and finalized the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonzalez-Fernandez, E., Huang, J. Cognitive Aspects of COVID-19. Curr Neurol Neurosci Rep 23, 531–538 (2023). https://doi.org/10.1007/s11910-023-01286-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-023-01286-y