Abstract
Purpose of Review
Amyloid beta (Aβ) plaque accumulation is a hallmark pathology contributing to Alzheimer’s disease (AD) and is widely hypothesized to lead to cognitive decline. Decades of research into anti-Aβ immunotherapies provide evidence for increased Aβ clearance from the brain; however, this is frequently accompanied by complicated vascular deficits. This article reviews the history of anti-Aβ immunotherapies and clinical findings and provides recommendations moving forward.
Recent Findings
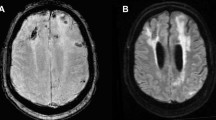
In 20 years of both animal and human studies, anti-Aβ immunotherapies have been a prevalent avenue of reducing hallmark Aβ plaques. In both models and with different anti-Aβ antibody designs, amyloid-related imaging abnormalities (ARIA) indicating severe cerebrovascular compromise have been common and concerning occurrence.
Summary
ARIA caused by anti-Aβ immunotherapy has been noted since the early 2000s, and the mechanisms driving it are still unknown. Recent approval of aducanumab comes with renewed urgency to consider vascular deficits caused by anti-Aβ immunotherapy.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hippius H, Neundorfer G. The discovery of Alzheimer’s disease. Dialogues Clin Neurosci. 2003;5(1):101–8.
Goate A, Chartier-Harlin M-C, Mullan M, Brown J, Crawford F, Fidani L, et al. Segregation of a missense mutation in the amyloid precursor protein gene with familial Alzheimer’s disease. Nature. 1991;349(6311):704–6. https://doi.org/10.1038/349704a0.
Hardy JA, Higgins GA. Alzheimer’s disease: the amyloid cascade hypothesis. Science. 1992;256(5054):184–5. https://doi.org/10.1126/science.1566067.
Selkoe DJ. Alzheimer’s disease: a central role for amyloid. J Neuropathol Exp Neurol. 1994;53(5):438–47. https://doi.org/10.1097/00005072-199409000-00003.
Pike CJ, Overman MJ, Cotman CW. Amino-terminal deletions enhance aggregation of β-amyloid peptides in vitro. J Biol Chem. 1995;270(41):23895–8. https://doi.org/10.1074/jbc.270.41.23895.
Iwatsubo T, Odaka A, Suzuki N, Mizusawa H, Nukina N, Ihara Y. Visualization of A beta 42(43) and A beta 40 in senile plaques with end-specific A beta monoclonals: evidence that an initially deposited species is A beta 42(43). Neuron. 1994;13(1):45–53. https://doi.org/10.1016/0896-6273(94)90458-8.
Niwa K, Carlson GA, Iadecola C. Exogenous Aβ1–40 reproduces cerebrovascular alterations resulting from amyloid precursor protein overexpression in mice. J Cereb Blood Flow Metab. 2000;20(12):1659–68. https://doi.org/10.1097/00004647-200012000-00005.
Gomis M, Sobrino TS, Ois A, MilláN MN, RodríGuez-Campello A, De La Ossa NPR, et al. Plasma β-amyloid 1–40 is associated with the diffuse small vessel disease subtype. Stroke. 2009;40(10):3197–201. https://doi.org/10.1161/strokeaha.109.559641.
Solomon B, Koppel R, Hanan E, Katzav T. Monoclonal antibodies inhibit in vitro fibrillar aggregation of the Alzheimer beta-amyloid peptide. Proc Natl Acad Sci. 1996;93(1):452–5. https://doi.org/10.1073/pnas.93.1.452.
Solomon B, Koppel R, Frankel D, Hanan-Aharon E. Disaggregation of Alzheimer beta-amyloid by site-directed mAb. Proc Natl Acad Sci U S A. 1997;94(8):4109–12. https://doi.org/10.1073/pnas.94.8.4109.
Schenk D, Barbour R, Dunn W, Gordon G, Grajeda H, Guido T, et al. Immunization with amyloid-beta attenuates Alzheimer-disease-like pathology in the PDAPP mouse. Nature. 1999;400(6740):173–7. https://doi.org/10.1038/22124. This paper is the first article showing effective immunization procedures to clear Aβ plaques in mice.
Morgan D, Diamond DM, Gottschall PE, Ugen KE, Dickey C, Hardy J, et al. Aβ peptide vaccination prevents memory loss in an animal model of Alzheimer’s disease. Nature. 2000;408(6815):982–5. https://doi.org/10.1038/35050116.
Janus C, Pearson J, McLaurin J, Mathews PM, Jiang Y, Schmidt SD, et al. Aβ peptide immunization reduces behavioural impairment and plaques in a model of Alzheimer’s disease. Nature. 2000;408(6815):979–82. https://doi.org/10.1038/35050110.
Chishti MA, Yang DS, Janus C, Phinney AL, Horne P, Pearson J, et al. Early-onset amyloid deposition and cognitive deficits in transgenic mice expressing a double mutant form of amyloid precursor protein 695. J Biol Chem. 2001;276(24):21562–70. https://doi.org/10.1074/jbc.M100710200.
Bard F, Cannon C, Barbour R, Burke RL, Games D, Grajeda H, et al. Peripherally administered antibodies against amyloid beta-peptide enter the central nervous system and reduce pathology in a mouse model of Alzheimer disease. Nat Med. 2000;6(8):916–9. https://doi.org/10.1038/78682. The authors show the first murine demonstration that peripheral immunization of anti-Aβ antibodies can cross the cerebrovasculature to mitigate Aβ plaque.
Vidarsson G, Dekkers G, Rispens T. IgG subclasses and allotypes: from structure to effector functions. Front Immunol. 2014;5:520. https://doi.org/10.3389/fimmu.2014.00520.
De Taeye SW, Rispens T, Vidarsson G. The ligands for human IgG and their effector functions. Antibodies. 2019;8(2):30. https://doi.org/10.3390/antib8020030.
Bacskai BJ, Kajdasz ST, McLellan ME, Games D, Seubert P, Schenk D, et al. Non-Fc-mediated mechanisms are involved in clearance of amyloid-beta in vivo by immunotherapy. J Neurosci. 2002;22(18):7873–8.
Bard F, Barbour R, Cannon C, Carretto R, Fox M, Games D, et al. Epitope and isotype specificities of antibodies to β-amyloid peptide for protection against Alzheimer’s disease-like neuropathology. Proc Natl Acad Sci. 2003;100(4):2023–8. https://doi.org/10.1073/pnas.0436286100.
Lightle S, Aykent S, Lacher N, Mitaksov V, Wells K, Zobel J, et al. Mutations within a human IgG2 antibody form distinct and homogeneous disulfide isomers but do not affect Fc gamma receptor or C1q binding. Protein Sci. 2010;19(4):753–62. https://doi.org/10.1002/pro.352.
Wilcock DM, DiCarlo G, Henderson D, Jackson J, Clarke K, Ugen KE, et al. Intracranially administered anti-Abeta antibodies reduce beta-amyloid deposition by mechanisms both independent of and associated with microglial activation. J Neurosci. 2003;23(9):3745–51.
Wilcock DM, Munireddy SK, Rosenthal A, Ugen KE, Gordon MN, Morgan D. Microglial activation facilitates Abeta plaque removal following intracranial anti-Abeta antibody administration. Neurobiol Dis. 2004;15(1):11–20. https://doi.org/10.1016/j.nbd.2003.09.015.
DeWitt DA, Perry G, Cohen M, Doller C, Silver J. Astrocytes regulate microglial phagocytosis of senile plaque cores of Alzheimer’s disease. Exp Neurol. 1998;149(2):329–40. https://doi.org/10.1006/exnr.1997.6738.
Wyss-Coray T, Loike JD, Brionne TC, Lu E, Anankov R, Yan F, et al. Adult mouse astrocytes degrade amyloid-beta in vitro and in situ. Nat Med. 2003;9(4):453–7. https://doi.org/10.1038/nm838.
DeMattos RB, Bales KR, Cummins DJ, Dodart JC, Paul SM, Holtzman DM. Peripheral anti-A beta antibody alters CNS and plasma A beta clearance and decreases brain A beta burden in a mouse model of Alzheimer’s disease. Proc Natl Acad Sci U S A. 2001;98(15):8850–5. https://doi.org/10.1073/pnas.151261398.
DeMattos RB, Bales KR, Cummins DJ, Paul SM, Holtzman DM. Brain to plasma amyloid-beta efflux: a measure of brain amyloid burden in a mouse model of Alzheimer’s disease. Science. 2002;295(5563):2264–7. https://doi.org/10.1126/science.1067568.
Pfeifer M, Boncristiano S, Bondolfi L, Stalder A, Deller T, Staufenbiel M, et al. Cerebral hemorrhage after passive anti-Abeta immunotherapy. Science. 2002;298(5597):1379. https://doi.org/10.1126/science.1078259.
Wilcock DM, Rojiani A, Rosenthal A, Subbarao S, Freeman MJ, Gordon MN, et al. Passive immunotherapy against Abeta in aged APP-transgenic mice reverses cognitive deficits and depletes parenchymal amyloid deposits in spite of increased vascular amyloid and microhemorrhage. J Neuroinflammation. 2004;1(1):24. https://doi.org/10.1186/1742-2094-1-24.
Racke MM, Boone LI, Hepburn DL, Parsadainian M, Bryan MT, Ness DK, et al. Exacerbation of cerebral amyloid angiopathy-associated microhemorrhage in amyloid precursor protein transgenic mice by immunotherapy is dependent on antibody recognition of deposited forms of amyloid beta. J Neurosci. 2005;25(3):629–36. https://doi.org/10.1523/JNEUROSCI.4337-04.2005.
Jellinger KA. Alzheimer disease and cerebrovascular pathology: an update. J Neural Transm. 2002;109(5–6):813–36. https://doi.org/10.1007/s007020200068.
Janota C, Lemere CA, Brito MA. Dissecting the contribution of vascular alterations and aging to Alzheimer’s disease. Mol Neurobiol. 2016;53(6):3793–811. https://doi.org/10.1007/s12035-015-9319-7.
Schenk D. Amyloid-β immunotherapy for Alzheimer’s disease: the end of the beginning. Nat Rev Neurosci. 2002;3(10):824–8. https://doi.org/10.1038/nrn938.
Buckwalter MS, Coleman BS, Buttini M, Barbour R, Schenk D, Games D, et al. Increased T cell recruitment to the CNS after amyloid beta1-42 immunization in Alzheimer’s mice overproducing transforming growth factor-beta1. J Neurosci. 2006;26(44):11437–41. https://doi.org/10.1523/jneurosci.2436-06.2006.
Ferrer I, Rovira MB, Guerra MLS, Rey MJ, Costa-Jussá F. Neuropathology and pathogenesis of encephalitis following amyloid β immunization in Alzheimer’s disease. Brain Pathol. 2004;14(1):11–20. https://doi.org/10.1111/j.1750-3639.2004.tb00493.x.
Nicoll JAR, Wilkinson D, Holmes C, Steart P, Markham H, Weller RO. Neuropathology of human Alzheimer disease after immunization with amyloid-β peptide: a case report. Nat Med. 2003;9(4):448–52. https://doi.org/10.1038/nm840.
Nicoll JAR, Barton E, Boche D, Neal JW, Ferrer I, Thompson P, et al. Aβ species removal after Aβ<sub>42</sub>immunization. J Neuropathol Exp Neurol. 2006;65(11):1040–8. https://doi.org/10.1097/01.jnen.0000240466.10758.ce.
Boche D, Zotova E, Weller RO, Love S, Neal JW, Pickering RM, et al. Consequence of Abeta immunization on the vasculature of human Alzheimer’s disease brain. Brain. 2008;131(Pt 12):3299–310. https://doi.org/10.1093/brain/awn261.
Salloway S, Sperling R, Gilman S, Fox NC, Blennow K, Raskind M, et al. A phase 2 multiple ascending dose trial of bapineuzumab in mild to moderate Alzheimer disease. Neurology. 2009;73(24):2061–70. https://doi.org/10.1212/wnl.0b013e3181c67808.
Salloway S, Sperling R, Fox NC, Blennow K, Klunk W, Raskind M, et al. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s disease. N Engl J Med. 2014;370(4):322–33. https://doi.org/10.1056/nejmoa1304839.
Vandenberghe R, Rinne JO, Boada M, Katayama S, Scheltens P, Vellas B, et al. Bapineuzumab for mild to moderate Alzheimer’s disease in two global, randomized, phase 3 trials. Alzheimer’s Res Ther. 2016;8(1). https://doi.org/10.1186/s13195-016-0189-7.
Black RS, Sperling RA, Safirstein B, Motter RN, Pallay A, Nichols A, et al. A single ascending dose study of bapineuzumab in patients with Alzheimer disease. Alzheimer Dis Assoc Disord. 2010;24(2):198–203. https://doi.org/10.1097/wad.0b013e3181c53b00.
Rinne JO, Brooks DJ, Rossor MN, Fox NC, Bullock R, Klunk WE, et al. 11C-PiB PET assessment of change in fibrillar amyloid-beta load in patients with Alzheimer’s disease treated with bapineuzumab: a phase 2, double-blind, placebo-controlled, ascending-dose study. Lancet Neurol. 2010;9(4):363–72. https://doi.org/10.1016/S1474-4422(10)70043-0.
Doody RS, Thomas RG, Farlow M, Iwatsubo T, Vellas B, Joffe S, et al. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s disease. N Engl J Med. 2014;370(4):311–21. https://doi.org/10.1056/nejmoa1312889.
Sperling RA, Jack CR Jr, Black SE, Frosch MP, Greenberg SM, Hyman BT, et al. Amyloid-related imaging abnormalities in amyloid-modifying therapeutic trials: recommendations from the Alzheimer’s Association Research Roundtable Workgroup. Alzheimers Dement. 2011;7(4):367–85. https://doi.org/10.1016/j.jalz.2011.05.2351.
Tampi RR, Forester BP, Agronin M. Aducanumab: evidence from clinical trial data and controversies. Drugs in Context. 2021;10:1–9. https://doi.org/10.7573/dic.2021-7-3.
Food and Drug Administration, Biogen. Peripheral and Central Nervous System (PCNS) Drugs Advisory Committee Meeting. 2020.
Sevigny J, Chiao P, Bussière T, Weinreb PH, Williams L, Maier M, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature. 2016;537(7618):50–6. https://doi.org/10.1038/nature19323.
Khan TK. Chapter 2 - Clinical diagnosis of Alzheimer’s disease. In: Khan TK, editor. Biomarkers in Alzheimer’s Disease. Academic Press; 2016. p. 27–48.
Knopman DS, Jones DT, Greicius MD. Failure to demonstrate efficacy of aducanumab: an analysis of the EMERGE and ENGAGE trials as reported by Biogen, December 2019. Alzheimers Dement. 2021;17(4):696–701. https://doi.org/10.1002/alz.12213. This paper outlines the timeline of clinical trials for aducanumab and FDA statements as well as highlights the areas where outcome measures fell short statistically and translationally. This subjective piece details the need for a third clinical trial since EMERGE and ENGAGE failed to provide evidence of efficacy.
Haeberlein SB, Von Hehn C, Tian Y, Chalkias S, Muralidharan KK, Chen T, et al. Emerge and Engage topline results: phase 3 studies of aducanumab in early Alzheimer’s disease. Alzheimer's & Dementia. 2020;16(S9). https://doi.org/10.1002/alz.047259.
Cummings J, Aisen P, Apostolova LG, Atri A, Salloway S, Weiner M. Aducanumab: appropriate use recommendations. J Prev Alzheimers Dis. 2021;8(4):398–410. https://doi.org/10.14283/jpad.2021.41.
Cummings J, Rabinovici GD, Atri A, Aisen P, Apostolova LG, Hendrix S, et al. Aducanumab: appropriate use recommendations update. J Prev Alzheimers Dis. 2022;9(2):221–30. https://doi.org/10.14283/jpad.2022.34. This article updates the appropriate use of aducanumab in the clinic. The authors outline the recommendations of patient population selection and clinical safety monitoring of ARIA events.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Dementia
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Foley, K.E., Wilcock, D.M. Vascular Considerations for Amyloid Immunotherapy. Curr Neurol Neurosci Rep 22, 709–719 (2022). https://doi.org/10.1007/s11910-022-01235-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-022-01235-1