Abstract
Purpose of Review
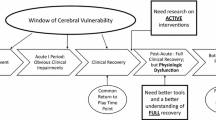
Concussion is a complex injury that may present as a variety of clinical profiles, which can overlap and reinforce one another. This review summarizes the medical management of patients with concussion and persistent post-concussive symptoms (PPCS).
Recent Findings
Management of concussion and PPCS relies on identifying underlying symptom generators. Treatment options include sub-symptom threshold aerobic exercise, cervical physical therapy, vestibular therapy, vision therapy, cognitive rehabilitation, cognitive behavioral therapy, pharmacological management, or a combination of treatments.
Summary
Evidence-based treatments have emerged to treat post-concussion symptom generators for sport-related concussion and for patients with PPCS.

Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Ellis MJ, Leddy JJ, Willer B. Physiological, vestibulo-ocular and cervicogenic post-concussion disorders: an evidence-based classification system with directions for treatment. Brain Inj. 2015;29(2):238–48.
McCrory P, Meeuwisse W, Johnston K, Dvorak J, Aubry M, Molloy M, et al. Consensus statement on Concussion in Sport–the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Br J Sports Med. 2009;43(Suppl 1):pp i76–90.
Stillman A, Madigan N, Alexander M. Factors associated with prolonged, subjective post-concussive symptoms. Neurology. 2016;86(16):3.325.
Gagnon I, Galli C, Friedman D, Grilli L, Iverson GL. Active rehabilitation for children who are slow to recover following sport-related concussion. Brain Inj. 2009;23(12):956–64.
Kontos AP, Jorgensen-Wagers K, Trbovich AM, Ernst N, Emami K, Gillie B, et al. Association of time since injury to the first clinic visit with recovery following concussion. JAMA Neurol. 2020;77(4):435–40.
Leddy JJ, Haider MN, Ellis MJ, Mannix R, Darling SR, Freitas MS, et al. Early subthreshold aerobic exercise for sport-related concussion: a randomized clinical trial. JAMA Pediatr. 2019;173(4):319–25.
Haider MN, Willer B, Leddy J, Ellis MJ. Multidisciplinary assessment and treatment. In: Silver JM, McAllister TW, Arciniegas DB, editors. Textbook of traumatic brain injury. 3rd ed: American Psychiatric Publishing, Inc. Arlington, VA; 2018.
Haider MN, Leddy JJ, Du W, A JM, Viera KB, Willer BS. Practical management: brief physical examination for sport-related concussion in the outpatient setting. Clin J Sport Med. 2018.
Leddy J, Lesh K, Haider MN, Czuczman N, Baker JG, Miecznikowski J, et al. Derivation of a focused, brief concussion physical examination for adolescents with sport-related concussion. Clin J Sport Med. 2018.
Wang DH, Kostyun RO, Trojian T, Solomito MJ. Overlapping concussion syndrome: defined in a pediatric population. Conn Med. 2017;81(7):389–94.
Weinstein E, Turner M, Kuzma BB, Feuer H. Second impact syndrome in football: new imaging and insights into a rare and devastating condition. J Neurosurg Pediatr. 2013;11(3):331–4.
McPherson JI, Saleem GT, Haider MN, Leddy JJ, Torres DM, Willer B. Practical management: telehealth examination for sport-related concussion in the outpatient setting. Clin J Sport Med. 2021.
Sutton M, Chan V, Escobar M, Mollayeva T, Hu Z, Colantonio A. Neck injury comorbidity in concussion-related emergency department visits: a population-based study of sex differences across the life span. J Womens Health. 2019;28(4):473–82.
McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838–47.
Kasamatsu T, Cleary M, Bennett J, Howard K, McLeod TV. Examining academic support after concussion for the adolescent student-athlete: perspectives of the athletic trainer. J Athl Train. 2016;51(2):153–61.
Quatman-Yates CC, Hunter-Giordano A, Shimamura KK, Landel R, Alsalaheen BA, Hanke TA, et al. Physical Therapy Evaluation and Treatment After Concussion/Mild Traumatic Brain Injury. J Orthop Sports Phys Ther. 2020;50(4):CPG1–73.
Anzalone AJ, Blueitt D, Case T, McGuffin T, Pollard K, Garrison JC, et al. A Positive Vestibular/Ocular Motor Screening (VOMS) Is Associated With Increased Recovery Time After Sports-Related Concussion in Youth and Adolescent Athletes. Am J Sports Med. 2017;45(2):474–9.
Giza CC, Hovda DA. The new neurometabolic cascade of concussion. Neurosurgery. 2014;75(suppl_4):S24–33.
Kozlowski KF, Graham J, Leddy JJ, Devinney-Boymel L, Willer BS. Exercise intolerance in individuals with postconcussion syndrome. J Athl Train. 2013;48(5):627–35.
Clausen M, Pendergast DR, Wilier B, Leddy J. Cerebral blood flow during treadmill exercise is a marker of physiological postconcussion syndrome in female athletes. J Head Trauma Rehabil. 2016;31(3):215–24.
Leddy JJ, Baker JG, Kozlowski K, Bisson L, Willer B. Reliability of a graded exercise test for assessing recovery from concussion. Clin J Sport Med. 2011;21(2):89–94.
Haider MN, Johnson SL, Mannix R, Macfarlane AJ, Constantino D, Johnson BD, et al. The buffalo concussion bike test for concussion assessment in adolescents. Sports Health. 2019;11(6):492–7.
Bezherano I, Haider MN, Willer BS, Leddy JJ. Practical management: prescribing subsymptom threshold aerobic exercise for sport-related concussion in the outpatient setting. Clin J Sport Med. 2021;31:465–68.
Leddy JJ, Haider MN, Ellis M, Willer BS. Exercise is medicine for concussion. Curr Sports Med Rep. 2018;17(8):262–70.
Majerske CW, Mihalik JP, Ren D, Collins MW, Reddy CC, Lovell MR, et al. Concussion in sports: postconcussive activity levels, symptoms, and neurocognitive performance. J Athl Train. 2008;43(3):265–74.
Maerlender A, Rieman W, Lichtenstein J, Condiracci C. Programmed physical exertion in recovery from sports-related concussion: a randomized pilot study. Dev Neuropsychol. 2015;40(5):273–8.
Peres G, Vandewalle H, Havette P. Heart rate, maximal heart rate and pedal rate. J Sports Med Phys Fitness. 1987;27(2):205.
Society HCCotIH. The international classification of headache disorders,(beta version). Cephalalgia. 2013;33(9):629–808.
Register-Mihalik JK, Vander Vegt CB, Cools M, Carnerio K. Factors Associated with Sport-Related Post-concussion Headache and Opportunities for Treatment. Curr Pain Headache Rep. 2018;22(11):75.
Marshall S, Bayley M, McCullagh S, Velikonja D, Berrigan L, Ouchterlony D, et al. Updated clinical practice guidelines for concussion/mild traumatic brain injury and persistent symptoms. Brain Inj. 2015;29(6):688–700.
Petrelli T, Farrokhyar F, McGrath P, Sulowski C, Sobhi G, DeMatteo C, et al. The use of ibuprofen and acetaminophen for acute headache in the postconcussive youth: a pilot study. Paediatr Child Health. 2017;22(1):2–6.
Nicolas S, Nicolas D. Triptans. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2020.
Navratilova E, Rau J, Oyarzo J, Tien J, Mackenzie K, Stratton J, et al. CGRP-dependent and independent mechanisms of acute and persistent post-traumatic headache following mild traumatic brain injury in mice. Cephalalgia. 2019;39(14):1762–75.
Baker JG, Willer BS, Dwyer MG, Leddy JJ. A preliminary investigation of cognitive intolerance and neuroimaging among adolescents returning to school after concussion. Brain Inj. 2020;34(6):818–27.
Macnow T, Curran T, Tolliday C, Martin K, McCarthy M, Ayturk D, et al. Effect of Screen Time on Recovery From Concussion: a Randomized Clinical Trial. JAMA Pediatrics. 2021.
Wasserman EB, Bazarian JJ, Mapstone M, Block R, van Wijngaarden E. Academic dysfunction after a concussion among US high school and college students. Am J Public Health. 2016;106(7):1247–53.
Reddy CC, Collins M, Lovell M, Kontos AP. Efficacy of amantadine treatment on symptoms and neurocognitive performance among adolescents following sports-related concussion. J Head Trauma Rehabil. 2013;28(4):260–5.
Plenger PM, Dixon CE, Castillo RM, Frankowski RF, Yablon SA, Levin HS. Subacute methylphenidate treatment for moderate to moderately severe traumatic brain injury: a preliminary double-blind placebo-controlled study. Arch Phys Med Rehabil. 1996;77(6):536–40.
Jaffee MS, Winter WC, Jones CC, Ling G. Sleep disturbances in athletic concussion. Brain Inj. 2015;29(2):221–7.
Barlow KM, Kirk V, Brooks B, Esser MJ, Yeates KO, Zemek R, et al. Efficacy of melatonin for sleep disturbance in children with persistent post-concussion symptoms: secondary analysis of a randomized controlled trial. J Neurotrauma. 2021;38(8):950–9.
Kamins J, Bigler E, Covassin T, Henry L, Kemp S, Leddy JJ, et al. What is the physiological time to recovery after concussion? Systematic review. Br J Sports Med. 2017:bjsports-2016–097464.
Whooley MA, Simon GE. Managing depression in medical outpatients. N Engl J Med. 2000;343(26):1942–50.
Trojian TH, Wang DH, Leddy JJ. Nutritional supplements for the treatment and prevention of sports-related concussion-evidence still lacking. Curr Sports Med Rep. 2017;16(4):247–55.
Barrett EC, McBurney MI, Ciappio ED. ω-3 fatty acid supplementation as a potential therapeutic aid for the recovery from mild traumatic brain injury/concussion. Adv Nutr. 2014;5(3):268–77.
McCrea M, Broglio SP, McAllister TW, Gill J, Giza CC, Huber DL, et al. Association of blood biomarkers with acute sport-related concussion in collegiate athletes: findings from the NCAA and department of defense CARE consortium. JAMA Netw Open. 2020;3(1):e1919771.
Haider MN, Leddy JJ, Pavlesen S, Kluczynski M, Baker JG, Miecznikowski JC, et al. A systematic review of criteria used to define recovery from sport-related concussion in youth athletes. Br J Sports Med. 2017:bjsports-2016–096551.
Funding
Research reported in this publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health (NIH) under award number 1R01NS094444 and the National Center for Advancing Translational Sciences of the NIH under award number UL1TR001412 to the University at Buffalo, SUNY. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
John J Leddy, MD: University at Buffalo, SUNY: Conception, design, and writing of the manuscript.
M Nadir Haider, MD: University at Buffalo, SUNY: Conception, design, and writing of the manuscript.
James M Noble, MD: Columbia University: Conception, design, and writing of the manuscript.
Brian Rieger, PhD: SUNY Upstate: Conception, design, and writing of the manuscript.
Steven Flanagan, MD: New York University: Conception, design, and writing of the manuscript.
Jacob I McPherson, DPT: University at Buffalo, SUNY: Design and writing of the manuscript.
Kenneth Shubin Stein, MD: Department of Neurology, Zucker School of Medicine: Design and writing of the manuscript.
Ghazala T Saleem, EdD, MS: University at Buffalo, SUNY: Design and writing of the manuscript.
Lou Corsaro, MD: Northern Westchester and Southern Putnam County School Districts.: Design and writing of the manuscript.
Barry S Willer, PhD: University at Buffalo, SUNY: Conception, design, and writing of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
John J Leddy, Flanagan Steven, Jacob I McPherson, Kenneth Shubin-Stein, Ghazala T. Saleem, Louis Corsaro, and Barry Willer each declare no potential conflicts of interest.
James M. Noble is the co-founder and chief medical officer of NoMo Diagnostics, which aims to develop an EEG-based concussion diagnostic tool; he has stock options in the company. Dr. Noble is co-inventor of a device with patent under review (Columbia University). Its use is not discussed or advised in the manuscript. In addition, Dr. Noble has a patent US20190298262A1 pending. The patent's use is licensed to NoMo Diagnostics.
Mohammad Nadir Haider has received personal fees from BlinkCNS and Oculogica Inc.
Brian Rieger reports equity interest in Quadrant Biosciences (Motion Intelligence), and is Co-Chair, Brain Injury Association of New York State—Concussion Initiative.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurotrauma
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Leddy, J.J., Haider, M.N., Noble, J.M. et al. Management of Concussion and Persistent Post-Concussive Symptoms for Neurologists. Curr Neurol Neurosci Rep 21, 72 (2021). https://doi.org/10.1007/s11910-021-01160-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s11910-021-01160-9