Abstract
Neuronal failure leading to dementia in neurodegenerative diseases is evidenced in vivo by functional and structural changes in the brain such as reductions of glucose consumption and volume of grey matter. The earliest phase of cognitive decline and presymptomatic stages of these diseases are heralded by specific patterns of hypometabolism, even in the absence of atrophy, which are currently considered as diagnostic biomarkers. Atrophy is less consistently found as an initial marker of these diseases and is invariably present in moderate to severe stages with a disease-related topography. The relationship between these two markers is not uniform, but in the two diseases in which they have been directly compared, Alzheimer’s and Parkinson’s disease, altered hypometabolism precedes and exceeds atrophy in most regions. This suggests a two-step degenerative process. In contrast to these findings, the hippocampus skips this pattern and is more structurally than functionally affected, thereby suggesting a different pathological mechanism in this particular area. More studies are needed to disentangle the mechanisms underlying both markers and their relationship in neurodegenerative diseases.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Jack Jr CR, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9(1):119–28. doi:10.1016/S1474-4422(09)70299-6.
Korf ES, Wahlund LO, Visser PJ, Scheltens P. Medial temporal lobe atrophy on MRI predicts dementia in patients with mild cognitive impairment. Neurology. 2004;63(1):94–100.
Boutet C, Chupin M, Lehericy S, Marrakchi-Kacem L, Epelbaum S, Poupon C, et al. Detection of volume loss in hippocampal layers in Alzheimer’s disease using 7 T MRI: a feasibility study. NeuroImage Clinl. 2014;5:341–8. doi:10.1016/j.nicl.2014.07.011. Boutet et al. were able to detect atrophy in distinct hippocampal layers in AD patients using a 7T MRI-based segmentation. This is a promising new technique for AD research and future investigations in that direction are worthwhile.
Chetelat G, Fouquet M, Kalpouzos G, Denghien I, De la Sayette V, Viader F, et al. Three-dimensional surface mapping of hippocampal atrophy progression from MCI to AD and over normal aging as assessed using voxel-based morphometry. Neuropsychologia. 2008;46(6):1721–31. doi:10.1016/j.neuropsychologia.2007.11.037.
Killiany RJ, Hyman BT, Gomez-Isla T, Moss MB, Kikinis R, Jolesz F, et al. MRI measures of entorhinal cortex vs hippocampus in preclinical AD. Neurology. 2002;58(8):1188–96.
Poulin SP, Dautoff R, Morris JC, Barrett LF, Dickerson BC. Alzheimer’s disease neuroimaging I. Amygdala atrophy is prominent in early Alzheimer’s disease and relates to symptom severity. Psychiatry Res. 2011;194(1):7–13. doi:10.1016/j.pscychresns.2011.06.014.
Greene SJ, Killiany RJ. Alzheimer’s disease neuroimaging I. Subregions of the inferior parietal lobule are affected in the progression to Alzheimer’s disease. Neurobiol Aging. 2010;31(8):1304–11. doi:10.1016/j.neurobiolaging.2010.04.026.
Chou YY, Lepore N, Saharan P, Madsen SK, Hua X, Jack CR, et al. Ventricular maps in 804 ADNI subjects: correlations with CSF biomarkers and clinical decline. Neurobiol Aging. 2010;31(8):1386–400. doi:10.1016/j.neurobiolaging.2010.05.001.
Fennema-Notestine C, Hagler Jr DJ, McEvoy LK, Fleisher AS, Wu EH, Karow DS, et al. Structural MRI biomarkers for preclinical and mild Alzheimer’s disease. Hum Brain Mapp. 2009;30(10):3238–53. doi:10.1002/hbm.20744.
Karow DS, McEvoy LK, Fennema-Notestine C, Hagler Jr DJ, Jennings RG, Brewer JB, et al. Relative capability of MR imaging and FDG PET to depict changes associated with prodromal and early Alzheimer disease. Radiology. 2010;256(3):932–42. doi:10.1148/radiol.10091402.
Whitwell JL, Przybelski SA, Weigand SD, Knopman DS, Boeve BF, Petersen RC, et al. 3D maps from multiple MRI illustrate changing atrophy patterns as subjects progress from mild cognitive impairment to Alzheimer’s disease. Brain J Neurol. 2007;130(Pt 7):1777–86. doi:10.1093/brain/awm112.
Hua X, Leow AD, Lee S, Klunder AD, Toga AW, Lepore N, et al. 3D characterization of brain atrophy in Alzheimer’s disease and mild cognitive impairment using tensor-based morphometry. Neuroimage. 2008;41(1):19–34. doi:10.1016/j.neuroimage.2008.02.010.
Leow AD, Yanovsky I, Parikshak N, Hua X, Lee S, Toga AW, et al. Alzheimer’s disease neuroimaging initiative: a one-year follow up study using tensor-based morphometry correlating degenerative rates, biomarkers and cognition. Neuroimage. 2009;45(3):645–55.
Chupin M, Gerardin E, Cuingnet R, Boutet C, Lemieux L, Lehericy S, et al. Fully automatic hippocampus segmentation and classification in Alzheimer’s disease and mild cognitive impairment applied on data from ADNI. Hippocampus. 2009;19(6):579–87. doi:10.1002/hipo.20626.
Fan Y, Batmanghelich N, Clark CM, Davatzikos C. Alzheimer’s disease neuroimaging I. Spatial patterns of brain atrophy in MCI patients, identified via high-dimensional pattern classification, predict subsequent cognitive decline. Neuroimage. 2008;39(4):1731–43. doi:10.1016/j.neuroimage.2007.10.031.
Westman E, Muehlboeck JS, Simmons A. Combining MRI and CSF measures for classification of Alzheimer’s disease and prediction of mild cognitive impairment conversion. Neuroimage. 2012;62(1):229–38. doi:10.1016/j.neuroimage.2012.04.056.
Cuingnet R, Gerardin E, Tessieras J, Auzias G, Lehericy S, Habert MO, et al. Automatic classification of patients with Alzheimer’s disease from structural MRI: a comparison of ten methods using the ADNI database. Neuroimage. 2011;56(2):766–81. doi:10.1016/j.neuroimage.2010.06.013.
Davatzikos C, Bhatt P, Shaw LM, Batmanghelich KN, Trojanowski JQ. Prediction of MCI to AD conversion, via MRI, CSF biomarkers, and pattern classification. Neurobiology of aging. 2011;32(12):2322 e19-27. doi:10.1016/j.neurobiolaging.2010.05.023.
Eskildsen SF, Coupe P, Garcia-Lorenzo D, Fonov V, Pruessner JC, Collins DL, et al. Prediction of Alzheimer’s disease in subjects with mild cognitive impairment from the ADNI cohort using patterns of cortical thinning. Neuroimage. 2013;65:511–21. doi:10.1016/j.neuroimage.2012.09.058. Eskildsen et al. used patterns of characteristic cortical thinning in disease stages of progressive MCI compared to MCI patients who remained stable for 3 years. This approach demonstrated promising results for the prediction of patients with prodromal AD progressing to probable AD.
Li Y, Rinne JO, Mosconi L, Pirraglia E, Rusinek H, DeSanti S, et al. Regional analysis of FDG and PIB-PET images in normal aging, mild cognitive impairment, and Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2008;35(12):2169–81. doi:10.1007/s00259-008-0833-y.
Mosconi L. Brain glucose metabolism in the early and specific diagnosis of Alzheimer’s disease. FDG-PET studies in MCI and AD. Eur J Nucl Med Mol Imaging. 2005;32(4):486–510. doi:10.1007/s00259-005-1762-7.
Chetelat G, Desgranges B, de la Sayette V, Viader F, Eustache F, Baron JC. Mild cognitive impairment: can FDG-PET predict who is to rapidly convert to Alzheimer’s disease? Neurology. 2003;60(8):1374–7.
Perneczky R, Hartmann J, Grimmer T, Drzezga A, Kurz A. Cerebral metabolic correlates of the clinical dementia rating scale in mild cognitive impairment. J Geriatr Psychiatry Neurol. 2007;20(2):84–8. doi:10.1177/0891988706297093.
Silverman DH, Small GW, Chang CY, Lu CS, Kung De Aburto MA, Chen W, et al. Positron emission tomography in evaluation of dementia: regional brain metabolism and long-term outcome. JAMA. 2001;286(17):2120–7.
Mosconi L, Perani D, Sorbi S, Herholz K, Nacmias B, Holthoff V, et al. MCI conversion to dementia and the APOE genotype: a prediction study with FDG-PET. Neurology. 2004;63(12):2332–40.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer's Demen J Alzheimer's Assoc. 2011;7(3):270–9. doi:10.1016/j.jalz.2011.03.008.
Patwardhan MB, McCrory DC, Matchar DB, Samsa GP, Rutschmann OT. Alzheimer disease: operating characteristics of PET—a meta-analysis. Radiology. 2004;231(1):73–80. doi:10.1148/radiol.2311021620.
de Leon MJ, Convit A, Wolf OT, Tarshish CY, DeSanti S, Rusinek H, et al. Prediction of cognitive decline in normal elderly subjects with 2-[(18)F]fluoro-2-deoxy-D-glucose/positron-emission tomography (FDG/PET). Proc Natl Acad Sci U S A. 2001;98(19):10966–71. doi:10.1073/pnas.191044198.
Jagust W, Gitcho A, Sun F, Kuczynski B, Mungas D, Haan M. Brain imaging evidence of preclinical Alzheimer’s disease in normal aging. Ann Neurol. 2006;59(4):673–81. doi:10.1002/ana.20799.
Ewers M, Brendel M, Rizk-Jackson A, Rominger A, Bartenstein P, Schuff N, et al. Reduced FDG-PET brain metabolism and executive function predict clinical progression in elderly healthy subjects. NeuroImage Clin. 2014;4:45–52. doi:10.1016/j.nicl.2013.10.018.
Prestia A, Caroli A, Wade SK, van der Flier WM, Ossenkoppele R, Van Berckel B, et al. Prediction of AD dementia by biomarkers following the NIA-AA and IWG diagnostic criteria in MCI patients from three European memory clinics. Alzheimer's Demen J Alzheimer’s Assoc. 2015. doi:10.1016/j.jalz.2014.12.001.
Kljajevic V, Grothe MJ, Ewers M, Teipel S. Alzheimer’s disease neuroimaging I. Distinct pattern of hypometabolism and atrophy in preclinical and predementia Alzheimer’s disease. Neurobiol Aging. 2014;35(9):1973–81. doi:10.1016/j.neurobiolaging.2014.04.006. Kljajevic et al. described a temporal ordering of neuronal injury markers in sporadic AD, according to which hypometabolism generally precedes atrophy, although with partly differing regional manifestations.
Dukart J, Kherif F, Mueller K, Adaszewski S, Schroeter ML, Frackowiak RS, et al. Generative FDG-PET and MRI model of aging and disease progression in Alzheimer’s disease. PLoS Comp Biol. 2013;9(4):e1002987. doi:10.1371/journal.pcbi.1002987.
Schroeter ML, Stein T, Maslowski N, Neumann J. Neural correlates of Alzheimer’s disease and mild cognitive impairment: a systematic and quantitative meta-analysis involving 1351 patients. Neuroimage. 2009;47(4):1196–206. doi:10.1016/j.neuroimage.2009.05.037.
Chetelat G, Desgranges B, Landeau B, Mezenge F, Poline JB, de la Sayette V, et al. Direct voxel-based comparison between grey matter hypometabolism and atrophy in Alzheimer’s disease. Brain J Neurol. 2008;131(Pt 1):60–71. doi:10.1093/brain/awm288.
Apostolova LG, Zarow C, Biado K, Hurtz S, Boccardi M, Somme J, et al. Relationship between hippocampal atrophy and neuropathology markers: a 7T MRI validation study of the EADC-ADNI harmonized hippocampal segmentation protocol. Alzheimer’s Demen J Alzheimer’s Assoc. 2015. doi:10.1016/j.jalz.2015.01.001.
Pedersen KF, Larsen JP, Tysnes OB, Alves G. Prognosis of mild cognitive impairment in early Parkinson disease: the Norwegian ParkWest study. JAMA Neurol. 2013;70(5):580–6. doi:10.1001/jamaneurol.2013.2110.
Gasca-Salas C, Estanga A, Clavero P, Aguilar-Palacio I, Gonzalez-Redondo R, Obeso JA, et al. Longitudinal assessment of the pattern of cognitive decline in non-demented patients with advanced Parkinson’s disease. J Parkinson’s Dis. 2014. doi:10.3233/JPD-140398.
Duncan GW, Firbank MJ, O’Brien JT, Burn DJ. Magnetic resonance imaging: a biomarker for cognitive impairment in Parkinson’s disease? Movement Disord Offic J Movement Disord Soc. 2013. doi:10.1002/mds.25352. Duncan et al. summarized studies that have used MRI to evaluate cognitive impairment in PD. They highlighted the advantages and disadvantages of the different techniques as potential biomarkers and guide future directions of research.
Jokinen P, Scheinin N, Aalto S, Nagren K, Savisto N, Parkkola R, et al. [(11)C]PIB-, [(18)F]FDG-PET and MRI imaging in patients with Parkinson’s disease with and without dementia. Parkinsonism Relat Disord. 2010;16(10):666–70. doi:10.1016/j.parkreldis.2010.08.021.
Garcia-Garcia D, Clavero P, Gasca Salas C, Lamet I, Arbizu J, Gonzalez-Redondo R, et al. Posterior parietooccipital hypometabolism may differentiate mild cognitive impairment from dementia in Parkinson’s disease. Eur J Nucl Med Mol Imaging. 2012;39(11):1767–77. doi:10.1007/s00259-012-2198-5.
Weintraub D, Doshi J, Koka D, Davatzikos C, Siderowf AD, Duda JE, et al. Neurodegeneration across stages of cognitive decline in Parkinson disease. Arch Neurol. 2011;68(12):1562–8. doi:10.1001/archneurol.2011.725.
Hosokai Y, Nishio Y, Hirayama K, Takeda A, Ishioka T, Sawada Y, et al. Distinct patterns of regional cerebral glucose metabolism in Parkinson’s disease with and without mild cognitive impairment. Movement Disord Offic J Movement Disord Soc. 2009;24(6):854–62. doi:10.1002/mds.22444.
Pereira JB, Ibarretxe-Bilbao N, Marti MJ, Compta Y, Junque C, Bargallo N, et al. Assessment of cortical degeneration in patients with Parkinson’s disease by voxel-based morphometry, cortical folding, and cortical thickness. Hum Brain Mapp. 2012;33(11):2521–34. doi:10.1002/hbm.21378.
Pagonabarraga J, Corcuera-Solano I, Vives-Gilabert Y, Llebaria G, Garcia-Sanchez C, Pascual-Sedano B, et al. Pattern of regional cortical thinning associated with cognitive deterioration in Parkinson’s disease. PloS one. 2013;8(1):e54980. doi:10.1371/journal.pone.0054980.
Camicioli R, Moore MM, Kinney A, Corbridge E, Glassberg K, Kaye JA. Parkinson’s disease is associated with hippocampal atrophy. Movement Disord Offic J Movement Disord Soc. 2003;18(7):784–90. doi:10.1002/mds.10444.
Agosta F, Canu E, Stefanova E, Sarro L, Tomic A, Spica V, et al. Mild cognitive impairment in Parkinson’s disease is associated with a distributed pattern of brain white matter damage. Hum Brain Mapp. 2013. doi:10.1002/hbm.22302.
Song SK, Lee JE, Park HJ, Sohn YH, Lee JD, Lee PH. The pattern of cortical atrophy in patients with Parkinson’s disease according to cognitive status. Movement Disord Offic J Movement Disord Soc. 2011;26(2):289–96. doi:10.1002/mds.23477.
Choi SH, Jung TM, Lee JE, Lee SK, Sohn YH, Lee PH. Volumetric analysis of the substantia innominata in patients with Parkinson’s disease according to cognitive status. Neurobiol Aging. 2012;33(7):1265–72. doi:10.1016/j.neurobiolaging.2010.11.015.
Compta Y, Pereira JB, Rios J, Ibarretxe-Bilbao N, Junque C, Bargallo N, et al. Combined dementia-risk biomarkers in Parkinson’s disease: a prospective longitudinal study. Parkinsonism Relat Disord. 2013;19(8):717–24. doi:10.1016/j.parkreldis.2013.03.009.
Lee JE, Cho KH, Song SK, Kim HJ, Lee HS, Sohn YH, et al. Exploratory analysis of neuropsychological and neuroanatomical correlates of progressive mild cognitive impairment in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2014;85(1):7–16. doi:10.1136/jnnp-2013-305062.
Goldman JG, Stebbins GT, Bernard B, Stoub TR, Goetz CG, de Toledo-Morrell L. Entorhinal cortex atrophy differentiates Parkinson’s disease patients with and without dementia. Movement Disord Offic J Movement Disord Soc. 2012;27(6):727–34. doi:10.1002/mds.24938.
Yong SW, Yoon JK, An YS, Lee PH. A comparison of cerebral glucose metabolism in Parkinson’s disease, Parkinson’s disease dementia and dementia with Lewy bodies. Eur J Neurol Offic J Eur Fed Neurol Soc. 2007;14(12):1357–62. doi:10.1111/j.1468-1331.2007.01977.x.
Lyoo CH, Jeong Y, Ryu YH, Rinne JO, Lee MS. Cerebral glucose metabolism of Parkinson’s disease patients with mild cognitive impairment. Eur Neurol. 2010;64(2):65–73. doi:10.1159/000315036.
Bohnen NI, Koeppe RA, Minoshima S, Giordani B, Albin RL, Frey KA, et al. Cerebral glucose metabolic features of Parkinson disease and incident dementia: longitudinal study. J Nucl Med Offic Pub Soc Nucl Med. 2011;52(6):848–55. doi:10.2967/jnumed.111.089946.
Huang C, Mattis P, Tang C, Perrine K, Carbon M, Eidelberg D. Metabolic brain networks associated with cognitive function in Parkinson’s disease. Neuroimage. 2007;34(2):714–23. doi:10.1016/j.neuroimage.2006.09.003.
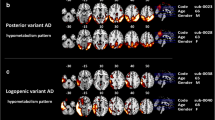
Gonzalez-Redondo R, Garcia-Garcia D, Clavero P, Gasca-Salas C, Garcia-Eulate R, Zubieta JL, et al. Grey matter hypometabolism and atrophy in Parkinson’s disease with cognitive impairment: a two-step process. Brain J Neurol. 2014;137(Pt 8):2356–67. doi:10.1093/brain/awu159. Gonzalez-Redondo et al. studied cerebral metabolism with FDG PET and grey matter volume with MRI in three groups of PD patients: cognitively normal, PD-MCI and PDD patients. The results showed a pattern of hypometabolism preceding atrophy in most of the affected brain areas, suggesting that there is a gradient of severity in cortical changes associated with the development of cognitive impairment in PD.
Colloby SJ, O’Brien JT, Taylor JP. Patterns of cerebellar volume loss in dementia with Lewy bodies and Alzheimer’s disease: a VBM-DARTEL study. Psychiatry Res. 2014;223(3):187–91. doi:10.1016/j.pscychresns.2014.06.006.
Warr L, Walker Z. Identification of biomarkers in Lewy-body disorders. Q J Nucl Med Mol Imaging. 2012;56(1):39–54. Warr and Walker provided an extensive review of specific biomarkers to distinguish DLB from other dementias. They included a review of the most important findings from studies using structural and functional imaging techniques.
Delli Pizzi S, Franciotti R, Tartaro A, Caulo M, Thomas A, Onofrj M, et al. Structural alteration of the dorsal visual network in DLB patients with visual hallucinations: a cortical thickness MRI study. PloS one. 2014;9(1):e86624. doi:10.1371/journal.pone.0086624.
Ishii K, Soma T, Kono AK, Sofue K, Miyamoto N, Yoshikawa T, et al. Comparison of regional brain volume and glucose metabolism between patients with mild dementia with Lewy bodies and those with mild Alzheimer’s disease. J Nucl Med Offic Pub Soc Nucl Med. 2007;48(5):704–11. doi:10.2967/jnumed.106.035691.
Burton EJ, McKeith IG, Burn DJ, Williams ED, O’Brien JT. Cerebral atrophy in Parkinson’s disease with and without dementia: a comparison with Alzheimer’s disease, dementia with Lewy bodies and controls. Brain J Neurol. 2004;127(Pt 4):791–800. doi:10.1093/brain/awh088.
Beyer MK, Larsen JP, Aarsland D. Gray matter atrophy in Parkinson disease with dementia and dementia with Lewy bodies. Neurology. 2007;69(8):747–54. doi:10.1212/01.wnl.0000269666.62598.1c.
Barber R, Ballard C, McKeith IG, Gholkar A, O’Brien JT. MRI volumetric study of dementia with Lewy bodies: a comparison with AD and vascular dementia. Neurology. 2000;54(6):1304–9.
Watson R, O’Brien JT, Barber R, Blamire AM. Patterns of gray matter atrophy in dementia with Lewy bodies: a voxel-based morphometry study. Int Psychogeriat / IPA. 2012;24(4):532–40. doi:10.1017/S1041610211002171.
Rodriguez MJ, Potter E, Shen Q, Barker W, Greig-Custo M, Agron J, et al. Cognitive and structural magnetic resonance imaging features of Lewy body dementia and Alzheimer’s disease. Alzheimer’s Demen J Alzheimer’s Assoc. 2012;8(3):211–8. doi:10.1016/j.jalz.2011.04.008.
Kantarci K, Ferman TJ, Boeve BF, Weigand SD, Przybelski S, Vemuri P, et al. Focal atrophy on MRI and neuropathologic classification of dementia with Lewy bodies. Neurology. 2012;79(6):553–60. doi:10.1212/WNL.0b013e31826357a5.
Teune LK, Bartels AL, de Jong BM, Willemsen AT, Eshuis SA, de Vries JJ, et al. Typical cerebral metabolic patterns in neurodegenerative brain diseases. Movement Disord Offic J Movement Disord Soc. 2010;25(14):2395–404. doi:10.1002/mds.23291.
Fujishiro H, Iseki E, Kasanuki K, Murayama N, Ota K, Suzuki M, et al. Glucose hypometabolism in primary visual cortex is commonly associated with clinical features of dementia with Lewy bodies regardless of cognitive conditions. Int J Geriatr Psychiatry. 2012;27(11):1138–46. doi:10.1002/gps.2836.
Perneczky R, Haussermann P, Diehl-Schmid J, Boecker H, Forstl H, Drzezga A, et al. Metabolic correlates of brain reserve in dementia with Lewy bodies: an FDG PET study. Dement Geriatr Cogn Disord. 2007;23(6):416–22. doi:10.1159/000101956.
Huang SH, Chang CC, Lui CC, Chen NC, Lee CC, Wang PW, et al. Cortical metabolic and nigrostriatal abnormalities associated with clinical stage-specific dementia with Lewy bodies. Clin Nucl Med. 2015;40(1):26–31. doi:10.1097/RLU.0000000000000620.
Fujishiro H, Iseki E, Kasanuki K, Chiba Y, Ota K, Murayama N, et al. A follow up study of non-demented patients with primary visual cortical hypometabolism: prodromal dementia with Lewy bodies. J Neurol Sci. 2013;334(1–2):48–54. doi:10.1016/j.jns.2013.07.013.
Kasanuki K, Iseki E, Fujishiro H, Yamamoto R, Higashi S, Minegishi M, et al. Neuropathological investigation of the hypometabolic regions on positron emission tomography with [18F] fluorodeoxyglucose in patients with dementia with Lewy bodies. J Neurol Sci. 2012;314(1–2):111–9. doi:10.1016/j.jns.2011.10.010.
Mak E, Su L, Williams GB, Watson R, Firbank M, Blamire AM, et al. Longitudinal assessment of global and regional atrophy rates in Alzheimer’s disease and dementia with Lewy bodies. NeuroImage Clin. 2015;7:456–62. doi:10.1016/j.nicl.2015.01.017.
Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51(6):1546–54.
Kipps CM, Hodges JR, Fryer TD, Nestor PJ. Combined magnetic resonance imaging and positron emission tomography brain imaging in behavioural variant frontotemporal degeneration: refining the clinical phenotype. Brain J Neurol. 2009;132(Pt 9):2566–78. doi:10.1093/brain/awp077.
Powers JP, Massimo L, McMillan CT, Yushkevich PA, Zhang H, Gee JC, et al. White matter disease contributes to apathy and disinhibition in behavioral variant frontotemporal dementia. Cognit Behav Neurol Offic J Soc Behav Cognit Neurol. 2014;27(4):206–14. doi:10.1097/WNN.0000000000000044.
Kipps CM, Davies RR, Mitchell J, Kril JJ, Halliday GM, Hodges JR. Clinical significance of lobar atrophy in frontotemporal dementia: application of an MRI visual rating scale. Dement Geriatr Cogn Disord. 2007;23(5):334–42. doi:10.1159/000100973.
Galton CJ, Patterson K, Graham K, Lambon-Ralph MA, Williams G, Antoun N, et al. Differing patterns of temporal atrophy in Alzheimer’s disease and semantic dementia. Neurology. 2001;57(2):216–25.
Chan D, Fox N, Rossor M. Differing patterns of temporal atrophy in Alzheimer’s disease and semantic dementia. Neurology. 2002;58(5):838.
Rohrer JD, Ridgway GR, Crutch SJ, Hailstone J, Goll JC, Clarkson MJ, et al. Progressive logopenic/phonological aphasia: erosion of the language network. Neuroimage. 2010;49(1):984–93. doi:10.1016/j.neuroimage.2009.08.002.
Suri S, Topiwala A, Mackay CE, Ebmeier KP, Filippini N. Using structural and diffusion magnetic resonance imaging to differentiate the dementias. Curr Neurol Neurosci Rep. 2014;14(9):475. doi:10.1007/s11910-014-0475-3.
Moller C, Dieleman N, van der Flier WM, Versteeg A, Pijnenburg Y, Scheltens P, et al. More atrophy of deep gray matter structures in frontotemporal dementia compared to Alzheimer’s disease. J Alzheimer’s Dis JAD. 2015;44(2):635–47. doi:10.3233/JAD-141230.
Salmon E, Garraux G, Delbeuck X, Collette F, Kalbe E, Zuendorf G, et al. Predominant ventromedial frontopolar metabolic impairment in frontotemporal dementia. Neuroimage. 2003;20(1):435–40.
Diehl J, Grimmer T, Drzezga A, Riemenschneider M, Forstl H, Kurz A. Cerebral metabolic patterns at early stages of frontotemporal dementia and semantic dementia. A PET study. Neurobiol Aging. 2004;25(8):1051–6. doi:10.1016/j.neurobiolaging.2003.10.007.
Garraux G, Salmon E, Degueldre C, Lemaire C, Laureys S, Franck G. Comparison of impaired subcortico-frontal metabolic networks in normal aging, subcortico-frontal dementia, and cortical frontal dementia. Neuroimage. 1999;10(2):149–62. doi:10.1006/nimg.1999.0463.
Hoffmann M. Frontal network syndrome testing: clinical tests and positron emission tomography brain imaging help distinguish the 3 most common dementia subtypes. Am J Alzheimers Dis Other Demen. 2013;28(5):477–84. doi:10.1177/1533317513488920.
Grimmer T, Diehl J, Drzezga A, Forstl H, Kurz A. Region-specific decline of cerebral glucose metabolism in patients with frontotemporal dementia: a prospective 18F-FDG-PET study. Dement Geriatr Cogn Disord. 2004;18(1):32–6. doi:10.1159/000077732.
Diehl-Schmid J, Grimmer T, Drzezga A, Bornschein S, Riemenschneider M, Forstl H, et al. Decline of cerebral glucose metabolism in frontotemporal dementia: a longitudinal 18F-FDG-PET-study. Neurobiol Aging. 2007;28(1):42–50. doi:10.1016/j.neurobiolaging.2005.11.002.
Schroeter ML, Neumann J. Combined imaging markers dissociate Alzheimer’s disease and frontotemporal lobar degeneration—an ALE meta-analysis. Front Aging Neurosci. 2011;3:10. doi:10.3389/fnagi.2011.00010.
Frisch S, Dukart J, Vogt B, Horstmann A, Becker G, Villringer A, et al. Dissociating memory networks in early Alzheimer’s disease and frontotemporal lobar degeneration—a combined study of hypometabolism and atrophy. PloS one. 2013;8(2):e55251. doi:10.1371/journal.pone.0055251.
Drzezga A, Grimmer T, Henriksen G, Stangier I, Perneczky R, Diehl-Schmid J, et al. Imaging of amyloid plaques and cerebral glucose metabolism in semantic dementia and Alzheimer’s disease. Neuroimage. 2008;39(2):619–33. doi:10.1016/j.neuroimage.2007.09.020.
Tripathi M, Tripathi M, Damle N, Kushwaha S, Jaimini A, D’Souza MM, et al. Differential diagnosis of neurodegenerative dementias using metabolic phenotypes on F-18 FDG PET/CT. Neuroradiol J. 2014;27(1):13–21.
Kerklaan BJ, van Berckel BN, Herholz K, Dols A, van der Flier WM, Scheltens P, et al. The added value of 18-fluorodeoxyglucose-positron emission tomography in the diagnosis of the behavioral variant of frontotemporal dementia. Am J Alzheimers Dis Other Demen. 2014;29(7):607–13. doi:10.1177/1533317514524811. Kerklaan et al. studied the diagnostic value of FDG PET in bvFTD without structural neuroimaging changes after 2 years. They established that this technique had a sensitivity of 47 % and a specificity of 92 %.
Esmaeilzadeh M, Ciarmiello A, Squitieri F. Seeking brain biomarkers for preventive therapy in Huntington disease. CNS Neurosci Ther. 2011;17(5):368–86. doi:10.1111/j.1755-5949.2010.00157.x.
Risacher SL, Saykin AJ. Neuroimaging biomarkers of neurodegenerative diseases and dementia. Semin Neurol. 2013;33(4):386–416. doi:10.1055/s-0033-1359312.
Rees EM, Scahill RI, Hobbs NZ. Longitudinal neuroimaging biomarkers in Huntington’s disease. J Huntington’s Dis. 2013;2(1):21–39. doi:10.3233/JHD-120030.
Aylward EH, Sparks BF, Field KM, Yallapragada V, Shpritz BD, Rosenblatt A, et al. Onset and rate of striatal atrophy in preclinical Huntington disease. Neurology. 2004;63(1):66–72.
Tabrizi SJ, Scahill RI, Durr A, Roos RA, Leavitt BR, Jones R, et al. Biological and clinical changes in premanifest and early stage Huntington’s disease in the TRACK-HD study: the 12-month longitudinal analysis. Lancet Neurol. 2011;10(1):31–42. doi:10.1016/S1474-4422(10)70276-3.
Tabrizi SJ, Reilmann R, Roos RA, Durr A, Leavitt B, Owen G, et al. Potential endpoints for clinical trials in premanifest and early Huntington’s disease in the TRACK-HD study: analysis of 24 month observational data. Lancet Neurol. 2012;11(1):42–53. doi:10.1016/S1474-4422(11)70263-0. Tabrizi et al. performed a longitudinal study (2 years) on premanifest gene carriers and patients with early HD, demonstrating a progressive atrophy (GM and whole-brain) associated with cognitive decline in both patient populations. Higher rates of brain atrophy and cognitive deterioration were exhibited by pre-HD subjects with progression.
Tabrizi SJ, Langbehn DR, Leavitt BR, Roos RA, Durr A, Craufurd D, et al. Biological and clinical manifestations of Huntington’s disease in the longitudinal TRACK-HD study: cross-sectional analysis of baseline data. Lancet Neurol. 2009;8(9):791–801. doi:10.1016/S1474-4422(09)70170-X.
Ciarmiello A, Cannella M, Lastoria S, Simonelli M, Frati L, Rubinsztein DC, et al. Brain white-matter volume loss and glucose hypometabolism precede the clinical symptoms of Huntington’s disease. J Nucl Med Offic Pub Soc Nucl Med. 2006;47(2):215–22.
Feigin A, Leenders KL, Moeller JR, Missimer J, Kuenig G, Spetsieris P, et al. Metabolic network abnormalities in early Huntington’s disease: an [(18)F]FDG PET study. J Nucl Med Offic Pub Soc Nucl Med. 2001;42(11):1591–5.
Kuwert T, Lange HW, Langen KJ, Herzog H, Aulich A, Feinendegen LE. Cortical and subcortical glucose consumption measured by PET in patients with Huntington’s disease. Brain J Neurol. 1990;113(Pt 5):1405–23.
Feigin A, Tang C, Ma Y, Mattis P, Zgaljardic D, Guttman M, et al. Thalamic metabolism and symptom onset in preclinical Huntington’s disease. Brain J Neurol. 2007;130(Pt 11):2858–67. doi:10.1093/brain/awm217.
Tang CC, Feigin A, Ma Y, Habeck C, Paulsen JS, Leenders KL, et al. Metabolic network as a progression biomarker of premanifest Huntington’s disease. J Clin Invest. 2013;123(9):4076–88. doi:10.1172/JCI69411. Tang et al. described a metabolic network characterized by progressive changes in striato-thalamic and cortical metabolic activity in a premanifest HD carrier cohort. This pattern of activity increased over 7 years and was not influenced by phenoconversion.
Acknowledgments
This work was supported by CIBERNED, Health Research Institute Carlos III grant PI081539, Basque Country Government grant 2011111074 (to M.C. R-O), Basque Country fellowships (to H. J-U. and M. D-A.), and Fundación Jesús de Gangoiti Barrera fellowship (to M. D-A.).
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Belen Gago, Pedro Clavero, Manuel Delgado-Alvarado, David Garcia-Garcia, and Haritz Jimenez-Urbieta declare that they have no conflict of interest.
María C. Rodriguez-Oroz reports non-financial support from UCB, non-financial support from Lundbeck, non-financial support from Boston Scientific, personal fees and non-financial support from Abbvie, grants from CIBERNED, grants from the Government of Basque Country and Guipuzcoa, grants from Spanish Health Institute, and grants from Era-net.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Neuroimaging
Rights and permissions
About this article
Cite this article
Rodriguez-Oroz, M.C., Gago, B., Clavero, P. et al. The Relationship Between Atrophy and Hypometabolism: Is It Regionally Dependent in Dementias?. Curr Neurol Neurosci Rep 15, 44 (2015). https://doi.org/10.1007/s11910-015-0562-0
Published:
DOI: https://doi.org/10.1007/s11910-015-0562-0