Abstract
Migraine is a disabling and prevalent disorder. Migraine is most effectively treated with a stepped care approach, where patients initially receive a broad level of care (primary care) and proceed to receive increasingly specialized care throughout the course of treatment. Behavioral treatments for migraine modify behaviors of people with migraine with the intention to prevent migraine episodes and secondary consequence of migraine. Behavioral treatments can be incorporated into each level of the stepped care approach for migraine treatment. In this article, we provide a rationale for including behavioral treatment strategies in the treatment of migraine. We then describe and review the evidence for behavioral treatment strategies for migraine, including patient education, relaxation strategies, biofeedback, and cognitive behavioral treatment strategies. Finally, we describe how behavioral treatments can be integrated into a stepped care approach for migraine care.

Similar content being viewed by others
References
Lipton RB et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–9.
Smitherman TA et al. The prevalence, impact, and treatment of migraine and severe headaches in the United States: a review of statistics from national surveillance studies. Headache. 2013;53(3):427–36. Provides a review of epidemiologic investigations of migraine and severe headaches in the United States, including information about prevalence, impact of migraine on patient’s lives, and treatment of migraine.
Murray C. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Los Angeles: Harvard University Press; 1996.
Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency. Narrative literature review. Br J Psychiatry. 2005;186:11–7.
Campbell J, Penzien D, Wall E. Evidence-based guidelines for migraine headache: behavioral and physical treatments: American Academy of Neurology Guidelines. 2000 Accessed February 21, 2012; Available from: www.aan.com/professionals/practice/pdfs/gl0089.pdf.
Silberstein S. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review). Neurology. 2000;55(6):754–62.
Penzien D, Rains J, Andrasik F. Behavioral management of recurrent headache: three decades of experience and empiricism. Appl Psychophysiol Biofeedback. 2002;27:163–81.
Schwartz MS, Andrasik F. Biofeedback: a practitioner’s guide. 3rd ed. New York: Guilford Press; 2003.
Buse DC. Multidisciplinary migraine management. Pain Med News. 2014;12.
Pesa J, Lage MJ. The medical costs of migraine and comorbid anxiety and depression. Head J Head Face Pain. 2004;44(6):562–70.
Hawkins K, Wang S, Rupnow M. Indirect cost burden of migraine in the United States. J Occup Environ Med. 2007;49(4):368–74.
Stokes M et al. Cost of health care among patients with chronic and episodic migraine in Canada and the USA: results from the International Burden of Migraine Study (IBMS). Headache. 2011;51(7):1058–77.
Schafer AM et al. Direct costs of preventive headache treatments: comparison of behavioral and pharmacologic approaches. Headache. 2011;51(6):985–91. Provides evidence for the cost-effectiveness of behavioral approaches for headache prevention.
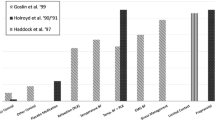
Haddock CK et al. Home-based behavioral treatments for chronic benign headache: a meta-analysis of controlled trials. Cephalalgia. 1997;17(2):113–8.
Rains J, Lipchik G, Penzien D. Behavioral facilitation of medical treatment for headache. Part I: review of headache treatment compliance. Head J Head Face Pain. 2006;46(9):1387–94.
Peters M et al. Patients’ decision-making for migraine and chronic daily headache management. A qualitative study. Cephalalgia. 2003;23(8):833–41.
Seng EK, Holroyd KA. Optimal use of acute headache medication: a qualitative examination of behaviors and barriers to their performance. Headache. 2013;53(9):1438–50.
Ramsey RR et al. Treatment adherence in patients with headache: a systematic review. Headache. 2014;54(5):795–816. A thorough systematic review of all types of treatment adherence (acute medications, preventive medications, lifestyle recommendations and behavioral management strategies) for headache disorders.
Tepper SJ. Medication-overuse headache. CONTIN Life Learn Neurol. 2012;18(4, Headache):807–22. doi:10.1212/01.CON.0000418644.32032.7b.
Andrasik F et al. Disability in chronic migraine with medication overuse: treatment effects at 3 years. Headache. 2007;47(9):1277–81.
Rains JC, Penzien DB, Lipchik GL. Behavioral facilitation of medical treatment for headache—part II: theoretical models and behavioral strategies for improving adherence. Headache. 2006;46(9):1395–403.
Dunbar-Jacob J et al. Adherence in chronic disease. Annu Rev Nurs Res. 2000;18:48–90.
Seng EK, Holroyd KA. Dynamics of changes in self-efficacy and locus of control expectancies in the behavioral and drug treatment of severe migraine. Ann Behav Med. 2010;40(3):235–47.
Nestoriuc Y et al. Biofeedback treatment for headache disorders: a comprehensive efficacy review. Appl Psychophysiol Biofeedback. 2008;33(3):125–40.
Blumenfeld A, Tischio M. Center of excellence for headache care: group model at Kaiser Permanente. Headache. 2003;43(5):431–40.
Lemstra M, Stewart B, Olszynski WP. Effectiveness of multidisciplinary intervention in the treatment of migraine: a randomized clinical trial. Headache. 2002;42(9):845–54.
Rothrock JF et al. The impact of intensive patient education on clinical outcome in a clinic-based migraine population. Headache. 2006;46(5):726–31.
Harpole LH et al. Headache management program improves outcome for chronic headache. Headache. 2003;43(7):715–24.
Holroyd KA et al. Enhancing the effectiveness of abortive therapy: a controlled evaluation of self-management training. Headache. 1989;29(3):148–53.
Cameron C. Patient compliance: recognition of factors involved and suggestions for promoting compliance with therapeutic regimens. J Adv Nurs. 1996;24(2):244–50.
Cady R et al. Nurse-based education: an office-based comparative model for education of migraine patients. Headache. 2008;48(4):564–9.
Smith TR, Nicholson RA, Banks JW. Migraine education improves quality of life in a primary care setting. Headache. 2010;50(4):600–12.
Holroyd KA et al. Effect of preventive (beta blocker) treatment, behavioural migraine management, or their combination on outcomes of optimised acute treatment in frequent migraine: randomised controlled trial. BMJ. 2010;341:c4871.
Cady RK et al. Rizatriptan 10-mg ODT for early treatment of migraine and impact of migraine education on treatment response. Headache. 2009;49(5):687–96.
Hahn SR et al. Healthcare provider–patient communication and migraine assessment: results of the American Migraine Communication Study, phase II. Curr Med Res Opin. 2008;24(6):1711–8.
Boyle D, Dwinnell B, Platt F. Invite, listen, and summarize: a patient-centered communication technique. Acad Med. 2005;80(1):29–32.
Benson H, Greenwood MM, Klemchuk H. The relaxation response: psychophysiologic aspects and clinical applications. Int J Psychiatry Med. 1975;6(1–2):87–98.
Jacobson E. Progressive relaxation. Chicago: University of Chicago Press; 1938.
Hall H. Hypnosis. In: Waldman S, editor. Pain management. Philadelphia: Saunders/Elsevier; 2011. p. 963–6.
Rime C, Andrasik F. Relaxation techniques and guided imagery. In: Waldman S, editor. Pain management. Philadelphia: Saunders/Elsevier; 2011. p. 967–75.
Smith JC. Relaxation, meditation & mindfulness: a mental health practitioner’s guide to new and traditional approaches. NY: Springer; 2005.
Goslin R, Gray RR, McCrory D. Behavioral and physical treatments for migraine headache. Technical review 2.2: available from: http://www.clinpol.mc.duke.edu (1999). [cited 2003 May 15].
Buse DC, Andrasik F. Behavioral medicine for migraine. Neurol Clin. 2009;27(2):445–65.
Penzien DB, Holroyd KA. Psychosocial interventions in the management of recurrent headache disorders. 2: description of treatment techniques. Behav Med. 1994;20(2):64–73.
Nestoriuc Y, Martin A. Efficacy of biofeedback for migraine: a meta-analysis. Pain. 2007;128(1–2):111–27.
Blanchard EB et al. Migraine and tension headache: a meta-analytic review. Behav Ther. 1980;11(5):613–31.
Blanchard EB, Andrasik F. Biofeedback treatment of vascular headache. In: Hatch JGFJP, Rugh JD, editors. Biofeedback: studies in clinical efficacy. New York: Plenum Press; 1987.
Holroyd KA, Penzien DB, Holm JE, Hursey KG. Behavioral treatment of recurrent headache: what does the literature say? In: American Association for the Study of Headache. San Francisco; 1984a, June.
Beck AT et al. Cognitive therapy of depression. New York: Guilford Press; 1979. p. 425.
Holroyd KA, Andrasik F. A cognitive-behavioral approach to recurrent tension and migraine headache. In: Kendall PE, editor. Advances in cognitive-behavioral research and therapy. New York: Academic; 1982. p. 276–320.
McCarran MS, Andrasik F. Migraine and tension headaches. In: Michelson L, Ascher M, editors. Anxiety and stress disorders: cognitive-behavioral assessment and treatment. NY: Guilford; 1987. p. 465–483.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215.
Holroyd K et al. Impaired functioning and quality of life in severe migraine: the role of catastrophizing and associated symptoms. Cephalalgia. 2007;27:1156–65.
French DJ et al. Perceived self-efficacy and headache-related disability. Headache. 2000;40(8):647–56.
Heath RL et al. Locus of control moderates the relationship between headache pain and depression. J Headache Pain. 2008;9(5):301–8.
Andrasik F. What does the evidence show? Efficacy of behavioural treatments for recurrent headaches in adults. Neurol Sci. 2007;28 Suppl 2:S70–7.
Penzien DB, Rains JC, Andrasik F. Behavioral management of recurrent headache: three decades of experience and empiricism. Appl Psychophysiol Biofeedback. 2002;27(2):163–81.
Blanchard EB et al. A controlled evaluation of the addition of cognitive therapy to a home-based biofeedback and relaxation treatment of vascular headache. Headache. 1990;30(6):371–6.
Mullally WJ, Hall K, Goldstein R. Efficacy of biofeedback in the treatment of migraine and tension type headaches. Pain Physician. 2009;12(6):1005–11.
Day MA et al. Mindfulness-based cognitive therapy for the treatment of headache pain: a pilot study. Clin J Pain. 2014;30(2):152–61.
Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8(2):163–90.
Dorflinger L, et al. A partnered approach to opioid management, guideline concordant care and the stepped care model of pain management. J Gen Intern Med. 2014;29:870–6.
Firth N, Barkham M, Kellett S. The clinical effectiveness of stepped care systems for depression in working age adults: a systematic review. J Affect Disord. 2014;170C:119–30.
Buse DC et al. Psychiatric comorbidities of episodic and chronic migraine. J Neurol. 2013;260(8):1960–9. A review of the most recent evidence regarding common psychiatric comorbidities of both episodic and chronic migraine.
Wang SJ, Chen PK, Fuh JL. Comorbidities of migraine. Front Neurol. 2010;1:16.
Smitherman TA, Rains JC, Penzien DB. Psychiatric comorbidities and migraine chronification. Curr Pain Headache Rep. 2009;13(4):326–31.
Lanteri-Minet M et al. Anxiety and depression associated with migraine: influence on migraine subjects’ disability and quality of life, and acute migraine management. Pain. 2005;118(3):319–26.
Ashina S et al. Depression and risk of transformation of episodic to chronic migraine. J Headache Pain. 2012;13(8):615–24.
Wang SJ et al. Quality of life differs among headache diagnoses: analysis of SF-36 survey in 901 headache patients. Pain. 2001;89(2–3):285–92.
Seng EK, Holroyd KA. Psychiatric comorbidity and response to preventative therapy in the treatment of severe migraine trial. Cephalalgia. 2012;32(5):390–400. A study that demonstrates moderation of headache changes during preventive behavioral and pharmacotherapy by the presence of a depression and/or anxiety disorder.
Compliance with Ethics Guidelines
Conflict of Interest
Alexandra B. Singer declares that he has no conflict of interest.
Dawn C. Buse has received consultancy fees and paid travel accommodations from Allergan Pharmaceuticals, grants from Allergan, the National Headache Foundation, Novartis, and Teva/NuPathe, and payment for manuscript preparation from the National Headache Foundation.
Elizabeth K. Seng has received honoraria payments from the Headache Cooperative of New England and paid travel accommodations from the International Headache Academy.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding authors
Additional information
This article is part of the Topical Collection on Headache
Rights and permissions
About this article
Cite this article
Singer, A.B., Buse, D.C. & Seng, E.K. Behavioral Treatments for Migraine Management: Useful at Each Step of Migraine Care. Curr Neurol Neurosci Rep 15, 14 (2015). https://doi.org/10.1007/s11910-015-0533-5
Published:
DOI: https://doi.org/10.1007/s11910-015-0533-5